Improved Antibiotic Prescribing for Acute Conjunctivitis After Operational Research: A Before-and-After Study in a Ghanaian Eye Hospital
Abstract
1. Introduction
- A total of 29% of patients receiving antibiotics had been prescribed them inappropriately, according to STG recommendations.
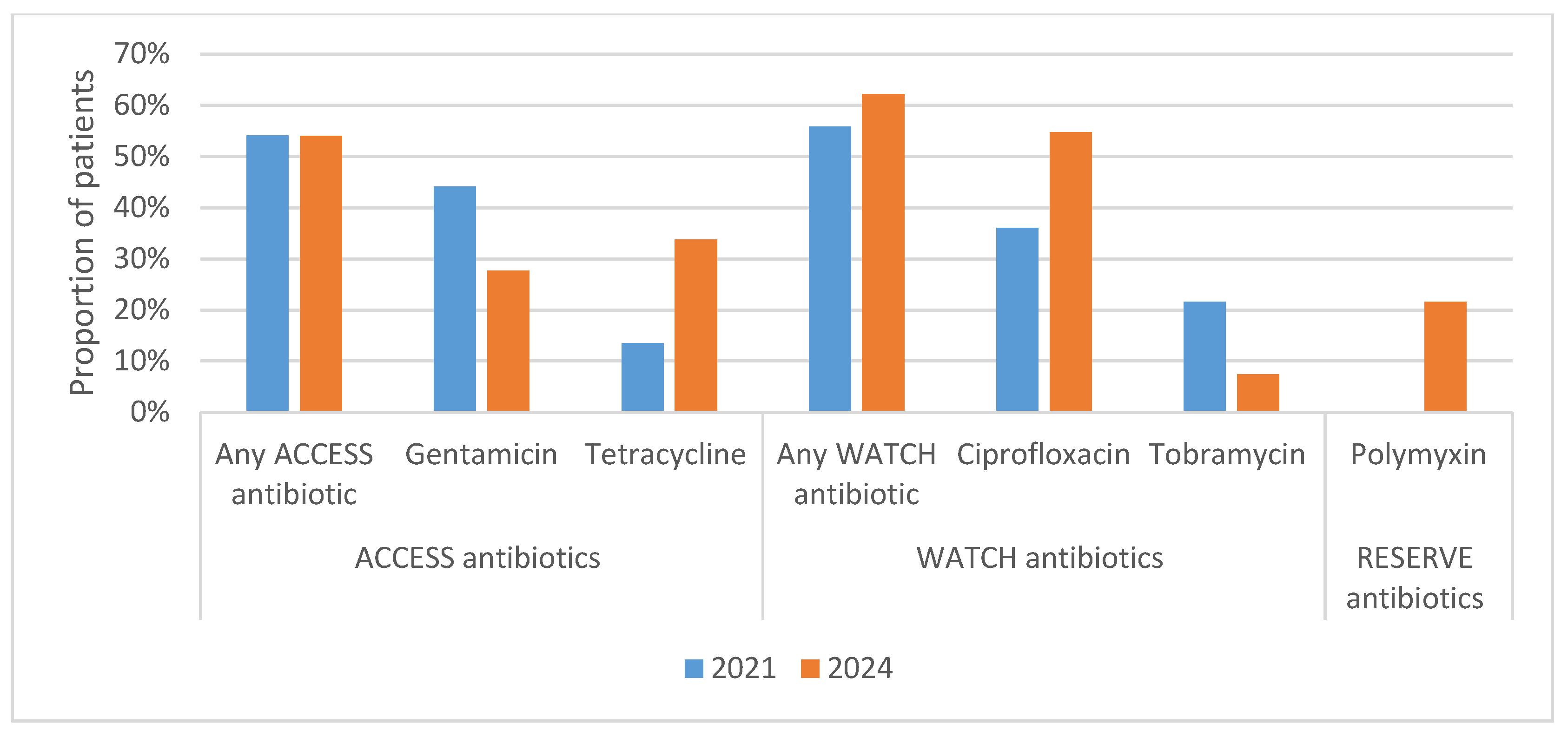
- A total of 56% of patients receiving antibiotics were prescribed antibiotics from the WATCH category of the WHO AWaRe scheme and the remainder prescribed antibiotics from the ACCESS category.
- To meet and brief the management of BAMCEC on the outcome and implications of the study.
- To meet and brief the Head of Ghana Eye Care Secretariat on the outcome and implications of the study.
- To meet and brief BAMCEC prescribers on the outcome and implications of the study.
- To establish a Local Antibiotic Stewardship Team (LAST).
- To monitor the use of antibiotics in the Eye Clinic by the LAST.
- To conduct Continuing Professional Development (CPD) training related to antibiotic prescribing through the Drugs and Therapeutic Committee at BAMCEC.
- Replication of the study in other eye care facilities with the oversight of the Ghana Eye Care Secretariat.
2. Materials and Methods
2.1. Study Design
2.2. Settings
2.2.1. General Setting
2.2.2. Specific Setting
2.3. Operational Definitions
- Appropriateness: (a) antibiotics prescribed for acute bacterial conjunctivitis; (b) not prescribing antibiotics in the absence of acute bacterial conjunctivitis.
- Inappropriateness: (a) not prescribing antibiotics when there is acute bacterial conjunctivitis; (b) prescribing antibiotics when there is no indication of bacterial conjunctivitis except where there are extenuating circumstances.
2.4. Study Population
- All cases of acute conjunctivitis from 1 January to 31 December 2021 at BAMCEC who were not prescribed antibiotics;
- All cases of acute conjunctivitis that were reported at BAMCEC from 1 January to 31 December 2024.
2.5. Inclusion Criteria
2.6. Data Variables and Sources of Data
2.7. Data Collection and Entry
2.8. Data Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics
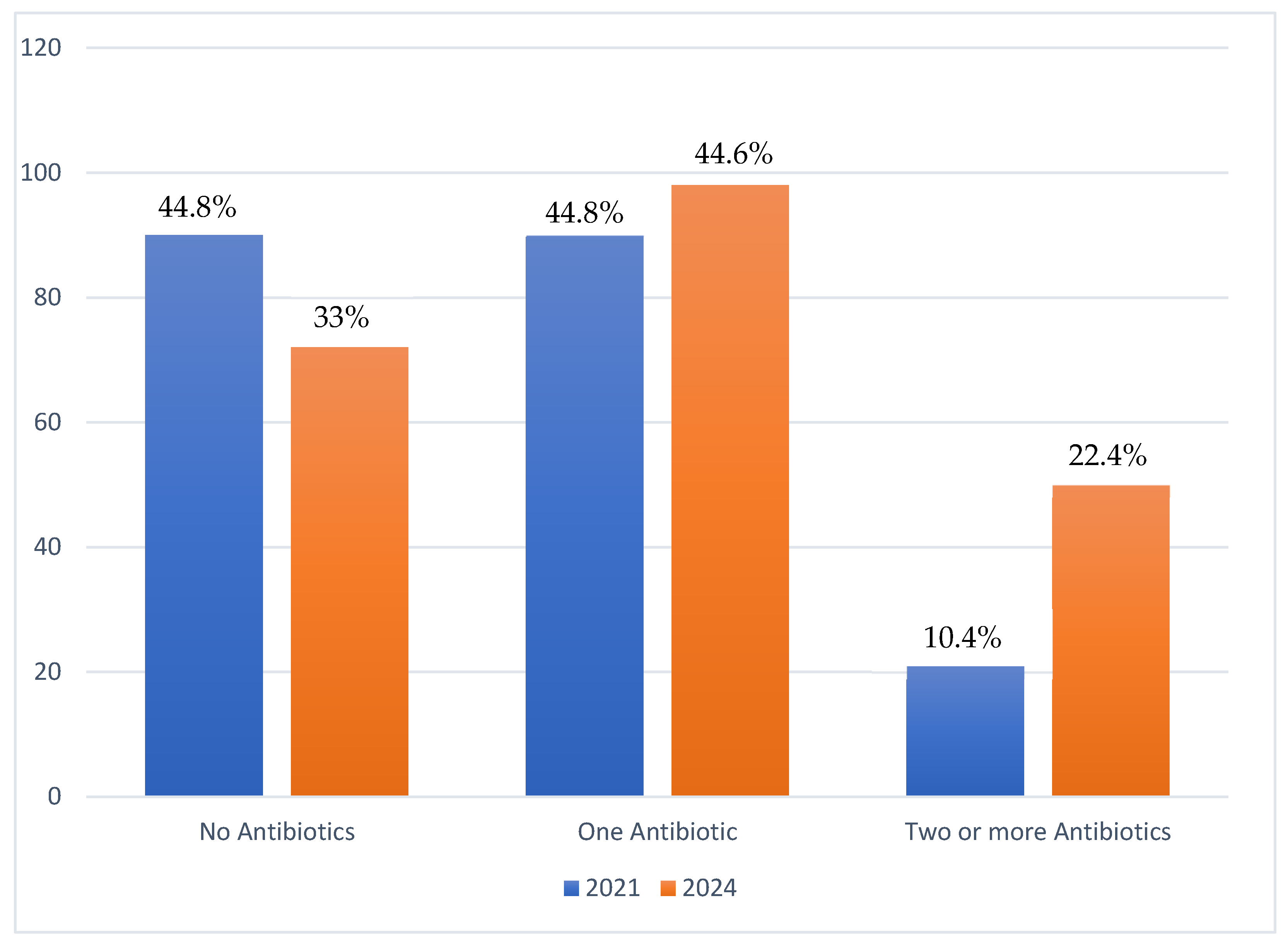
3.2. Proportions of Patients Prescribed Antibiotics
3.3. Appropriateness of Prescribing Antibiotics for Treatment of AC in a Ghanaian Eye Hospital
3.4. Types and Proportions of Antibiotics Prescribed per the WHO AWaRe Classification
4. Discussion
- Monitor the use of antibiotics in the eye clinic by the Local Antibiotic Stewardship Team (LAST);
- Conduct Continuing Professional Development (CPD) training related to antibiotic prescribing through the Drugs and Therapeutic Committee (DTC) at BAMCEC.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shekhawat, N.S.; Shtein, R.M.; Blachley, T.S.; Stein, J.D. Antibiotic Prescription Fills for Acute Conjunctivitis among Enrollees in a Large United States Managed Care Network. Ophthalmology 2017, 124, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Leibowitz, H.M.; Pratt, M.V.; Flagstad, I.J.; Berrospi, A.R.; Kundsin, R. Human Conjunctivitis: II. Treatment. Arch. Ophthalmol. 1976, 94, 1752–1756. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, M.B.; Croasdale, C.R. The Red Eye: A Clinical Guide to a Rapid and Accurate Diagnosis. In Cornea; Mosby: St. Louis, MO, USA, 1997; pp. 438–445. [Google Scholar]
- Varu, D.M.; Rhee, M.K.; Akpek, E.K.; Amescua, G.; Farid, M.; Garcia-Ferrer, F.J.; Lin, A.; Musch, D.C.; Mah, F.S.; Dunn, S.P. Conjunctivitis Preferred Practice Pattern®. Ophthalmology 2019, 126, P94–P169. [Google Scholar] [CrossRef] [PubMed]
- Azari, A.A.; Arabi, A. Conjunctivitis: A Systematic Review. J. Ophthalmic Vis. Res. 2020, 15, 372–395. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, T.P.; Jeng, B.H.; McDonald, M.; Raizman, M.B. Acute Conjunctivitis: Truth and Misconceptions. Curr. Med. Res. Opin. 2009, 25, 1953–1961. [Google Scholar] [CrossRef] [PubMed]
- Cronau, H.; Kankanala, R.R.; Mauger, T. Diagnosis and Management of Red Eye in Primary Care. Am. Fam. Physician 2010, 81, 137–144. [Google Scholar] [PubMed]
- Ryder, E.C.; Benson, S. Conjunctivitis. In StatPearls; StatPearls Publishing LLC: Treasure Island, FL, USA, 2020; p. 7431717. [Google Scholar]
- Azari, A.A.; Barney, N.P. Conjunctivitis: A Systematic Review of Diagnosis and Treatment. JAMA 2013, 310, 1721–1730. [Google Scholar] [CrossRef] [PubMed]
- Smith, G. Differential Diagnosis of Red Eye. Pediatr. Nurs. 2010, 36, 213–215. [Google Scholar] [PubMed]
- Ministry of Health. Ghana National Drugs Programme: Standard Treatment Guidelines, 7th ed.; Ministry of Health: Accra, Ghana, 2017; ISBN 9789988257873.
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial Resistance: A Global Multifaceted Phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Organization World Health. Global Antimicrobial Resistance and Use Surveillance System (GLASS); Antibiotic Use Data for 2022; World Health Organization: Geneva, Switzerland, 2025. [Google Scholar]
- Centres for Disease Control and Prevention. US Department of Health and Human Services. Antibiotic Resistance Threats in the United States; CDC: Atlanta, GA, USA, 2013; p. 4768623. Available online: https://www.cdc.gov/Drugresistance/Pdf/Ar-Threats-2013-508.Pdf (accessed on 1 August 2025).
- Kapi, A. The Evolving Threat of Antimicrobial Resistance: Options for Action. Indian J. Med. 2014, 139, 182. [Google Scholar]
- Asamoah, B.; Labi, A.-K.; Gupte, H.A.; Davtyan, H.; Peprah, G.M.; Adu-Gyan, F.; Nair, D.; Muradyan, K.; Jessani, N.S.; Sekyere-Nyantakyi, P. High Resistance to Antibiotics Recommended in Standard Treatment Guidelines in Ghana: A Cross-Sectional Study of Antimicrobial Resistance Patterns in Patients with Urinary Tract Infections between 2017–2021. Int. J. Environ. Res. Public Health 2022, 19, 16556. [Google Scholar] [CrossRef] [PubMed]
- Donkor, E.S.; Odoom, A.; Osman, A.; Darkwah, S.; Kotey, F.C.N. A Systematic Review on Antimicrobial Resistance in Ghana from a One Health Perspective. Antibiotics 2024, 13, 662. [Google Scholar] [CrossRef] [PubMed]
- Walana, W.; Vicar, E.K.; Kuugbee, E.D.; Sakida, F.; Baba, I. Antimicrobial Resistance of Clinical Bacterial Isolates According to the WHO’ s AWaRe and the ECDC-MDR Classifications: The Pattern in Ghana’ s Bono East Region Introduction. Front. Antibiot. Front. Antibiot. 2023, 2, 1291046. [Google Scholar] [CrossRef]
- Ahmed, H.; Zolfo, M.; Williams, A.; Ashubwe-Jalemba, J.; Tweya, H.; Adeapena, W.; Labi, A.; Adomako, L.A.B.; Addico, G.N.D.; Banu, R.A.; et al. Antibiotic-Resistant Bacteria in Drinking Water from the Greater Accra Region, Ghana: A Cross-Sectional Study, December 2021–March 2022. Int. J. Environ. Res. Public Health 2022, 19, 12300. [Google Scholar] [CrossRef] [PubMed]
- Ohene Larbi, R.; Adeapena, W.; Ayim-Akonor, M.; Ansa, E.D.O.; Tweya, H.; Terry, R.F.; Labi, A.K.; Harries, A.D. Antimicrobial, Multi-Drug and Colistin Resistance in Enterobacteriaceae in Healthy Pigs in the Greater Accra Region of Ghana, 2022: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 449. [Google Scholar] [CrossRef] [PubMed]
- Sefah, I.A.; Quagraine, A.M.; Kurdi, A.; Mudenda, S.; Godman, B. Audit of Antibiotic Utilization Patterns and Practice for Common Eye Infections at the Ambulatory Clinic of a Teaching Hospital in Ghana: Findings and Implications. PLoS ONE 2024, 19, e0313019. [Google Scholar] [CrossRef] [PubMed]
- Hope, P.K.F.; Lynen, L.; Mensah, B.; Appiah, F.; Kamau, E.M.; Ashubwe-Jalemba, J.; Peprah Boaitey, K.; Adomako, L.A.B.; Alaverdyan, S.; Appiah-Thompson, B.L.; et al. Appropriateness of Antibiotic Prescribing for Acute Conjunctivitis: A Cross-Sectional Study at a Specialist Eye Hospital in Ghana, 2021. Int. J. Environ. Res. Public Health 2022, 19, 11723. [Google Scholar] [CrossRef] [PubMed]
- Spellberg, B.; Hansen, G.R.; Kar, A.; Cordova, C.D.; Price, L.B.; Johnson, J.R. Antibiotic Resistance in Humans and Animals; National Academy of Medicine (NAM) Perspective: Washington, DC, USA, 2016. [Google Scholar]
- Frieri, M.; Kumar, K.; Boutin, A. Antibiotic Resistance. J. Infect. Public Health 2017, 10, 369–378. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report of the 6 Meeting: WHO Advisory Group on Integrated Survaillance of Antimicrobial Resistance with AGISAR 5-Year Strategic Framework of the Global Action Plan on Antimicribial Resistance; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Ministry of Health. Ghana National Action Plan for Antimicrobial Use and Resistance Republic of Ghana; Ministry of Health: Accra, Ghana, 2017; ISBN 9789988266554.
- Zanichelli, V.; Sharland, M.; Cappello, B.; Moja, L.; Getahun, H.; Pessoa-Silva, C.; Sati, H.; van Weezenbeek, C.; Balkhy, H.; Simão, M.; et al. The WHO AWaRe (Access, Watch, Reserve) Antibiotic Book and Prevention of Antimicrobial Resistance. Bull. World Health Organ. 2023, 101, 290–296. [Google Scholar] [CrossRef]
- Ghana Statistical Service Press Release. Available online: https://census2021.statsghana.gov.gh/presspage.php?readmorenews=MTQ1MTUyODEyMC43MDc1&Press-Release-on-Provisional-Results#:~:text=Today%2C%2022nd%20September%202021,and%20Housing%20Census%20(PHC).&text=Ghana’s%20population%20figure%20from%20the,structures%20were%20for%20residential%20use (accessed on 19 July 2024).
- Cuschieri, S. The STROBE Guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | 2021 (N = 201) | 2024 (N = 220) | p-Value 1 | ||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Age group (years) | |||||
| <5 | 78 | (38.8) | 46 | (20.9) | <0.001 |
| 5–17 | 43 | (21.4) | 44 | (20.0) | |
| ≥18 | 80 | (39.8) | 130 | (59.1) | |
| Sex | |||||
| Male | 89 | (44.3) | 101 | (45.9) | 0.737 |
| Female | 112 | (55.7) | 119 | (54.1) | |
| Residence | |||||
| Ashanti | 0 | (0) | 2 | (0.9) | <0.001 |
| Central | 163 | (81.1) | 212 | (96.4) | |
| Western | 32 | (15.9) | 6 | (2.7) | |
| Western North | 5 | (2.5) | 0 | (0) | |
| Greater Accra | 1 | (0.5) | 0 | (0) | |
| Prescriber cadre | |||||
| Ophthalmologist | 2 | (1.0) | 0 | (0) | 0.008 |
| Optometrist | 107 | (53.2) | 145 | (65.9) | |
| Ophthalmic nurse | 92 | (45.8) | 75 | (34.1) | |
| Type of acute conjunctivitis | |||||
| Bacterial | NA | 89 | (40.4) | - | |
| Viral | NA | 20 | (9.1) | ||
| Non-infectious | NA | 111 | (50.5) | ||
| Prescribed antibiotics | |||||
| Yes | 111 | (55.2) | 148 | (67.3) | 0.011 |
| No | 90 | (44.8) | 72 | (32.7) | |
| Variable | Total | Antibiotic Prescription | OR | (95% CI) | aOR | (95% CI) | p-Value | |
|---|---|---|---|---|---|---|---|---|
| n | (%) 1 | |||||||
| Year | ||||||||
| 2021 | 201 | 111 | (55.2) | Ref | Ref | |||
| 2024 | 220 | 148 | (67.3) | 1.67 | (1.12–2.47) | 2.51 | (1.51–4.19) | <0.001 |
| Age (years) | ||||||||
| <5 | 124 | 113 | (91.1) | 7.60 | (3.58–16.10) | 10.01 | (4.57–21.9) | <0.001 |
| 5–17 | 87 | 50 | (57.5) | Ref | Ref | |||
| ≥18 | 210 | 96 | (45.7) | 0.62 | (0.37–1.03) | 0.52 | (0.29–0.93) | 0.027 |
| Sex | ||||||||
| Male | 190 | 117 | (61.6) | Ref | Ref | |||
| Female | 231 | 142 | (61.5) | 0.99 | (0.67–1.48) | 1.16 | (072–1.86) | 0.525 |
| Region | ||||||||
| Central | 375 | 248 | (66.1) | 6.29 | (2.89–13.7) | 2.26 | (0.95–5.41) | 0.067 |
| Western | 38 | 9 | (23.7) | Ref | Ref | |||
| Other regions | 8 | 2 | (25.0) | 1.07 | (0.18–6.28) | 0.59 | (0.07–5.01) | 0.634 |
| Prescriber cadre | ||||||||
| Optometrist | 254 | 164 | (64.6) | 1.38 | (0.92–2.06) | 2.13 | (1.29–3.39) | 0.003 |
| Ophthalmic nurse | 167 | 95 | (56.9) | Ref | Ref | |||
| Variable | Total | Appropriate Antibiotic Prescription | OR | (95% CI) | aOR | (95% CI) | p-Value | |
|---|---|---|---|---|---|---|---|---|
| n | (%) 1 | |||||||
| Year | ||||||||
| 2021 | 111 | 79 | (71.2) | Ref | Ref | |||
| 2024 | 148 | 129 | (87.2) | 2.75 | (1.46–5.18) | 2.76 | (1.32–5.78) | 0.007 |
| Age (years) | ||||||||
| <5 | 113 | 93 | (82.3) | 2.61 | (1.23–5.55) | 3.04 | (1.41–6.76) | 0.005 |
| 5–17 | 50 | 32 | (64.0) | Ref | Ref | |||
| ≥18 | 96 | 83 | (86.5) | 3.59 | (1.57–8.17) | 2.22 | (0.87–5.67) | 0.093 |
| Sex | ||||||||
| Male | 117 | 92 | (78.6) | Ref | Ref | |||
| Female | 142 | 116 | (81.7) | 1.21 | (0.65–2.24) | 1.07 | (0.55–2.06) | 0.833 |
| Region | ||||||||
| Central | 248 | 199 | (80.2) | 1.16 | (0.23–5.76) | 1.18 | (0.21–6.69) | 0.846 |
| Western | 9 | 7 | (77.8) | Ref | Ref | |||
| Other regions | 2 | 2 | (100.0) | - | - | |||
| Prescriber cadre | ||||||||
| Optometrist | 164 | 137 | (83.5) | 1.71 | (0.92–3.19) | 1.43 | (0.73–2.80) | 0.297 |
| Ophthalmic nurse | 95 | 71 | (74.7) | Ref | Ref | |||
| 2021 (N = 131) | 2024 (N = 215) | p-Value 2 | |||
|---|---|---|---|---|---|
| n | (%) 1 | n | (%) 1 | ||
| Access antibiotics | 64 | (48.8) | 91 | (42.3) | <0.001 |
| Watch antibiotics | 67 | (51.2) | 92 | (42.8) | |
| Reserve antibiotics | 0 | (0) | 32 | (14.9) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ansong, H.K.; Nair, D.; Koomson, J.A.; Amponsah, O.K.O.; Acquah, J.F.; Buckman, J.; Ramsay, A.; Hope, P.K.F. Improved Antibiotic Prescribing for Acute Conjunctivitis After Operational Research: A Before-and-After Study in a Ghanaian Eye Hospital. Trop. Med. Infect. Dis. 2025, 10, 301. https://doi.org/10.3390/tropicalmed10110301
Ansong HK, Nair D, Koomson JA, Amponsah OKO, Acquah JF, Buckman J, Ramsay A, Hope PKF. Improved Antibiotic Prescribing for Acute Conjunctivitis After Operational Research: A Before-and-After Study in a Ghanaian Eye Hospital. Tropical Medicine and Infectious Disease. 2025; 10(11):301. https://doi.org/10.3390/tropicalmed10110301
Chicago/Turabian StyleAnsong, Henry Kissinger, Divya Nair, Joana Abokoma Koomson, Obed Kwabena Offe Amponsah, Jane Frances Acquah, James Buckman, Andrew Ramsay, and Paa Kwesi Fynn Hope. 2025. "Improved Antibiotic Prescribing for Acute Conjunctivitis After Operational Research: A Before-and-After Study in a Ghanaian Eye Hospital" Tropical Medicine and Infectious Disease 10, no. 11: 301. https://doi.org/10.3390/tropicalmed10110301
APA StyleAnsong, H. K., Nair, D., Koomson, J. A., Amponsah, O. K. O., Acquah, J. F., Buckman, J., Ramsay, A., & Hope, P. K. F. (2025). Improved Antibiotic Prescribing for Acute Conjunctivitis After Operational Research: A Before-and-After Study in a Ghanaian Eye Hospital. Tropical Medicine and Infectious Disease, 10(11), 301. https://doi.org/10.3390/tropicalmed10110301








