Reconstruction of Chronic Soft Tissue Mallet Fingers: Outcomes of Step-Plasty vs. Purse-String Suture
Abstract
1. Introduction
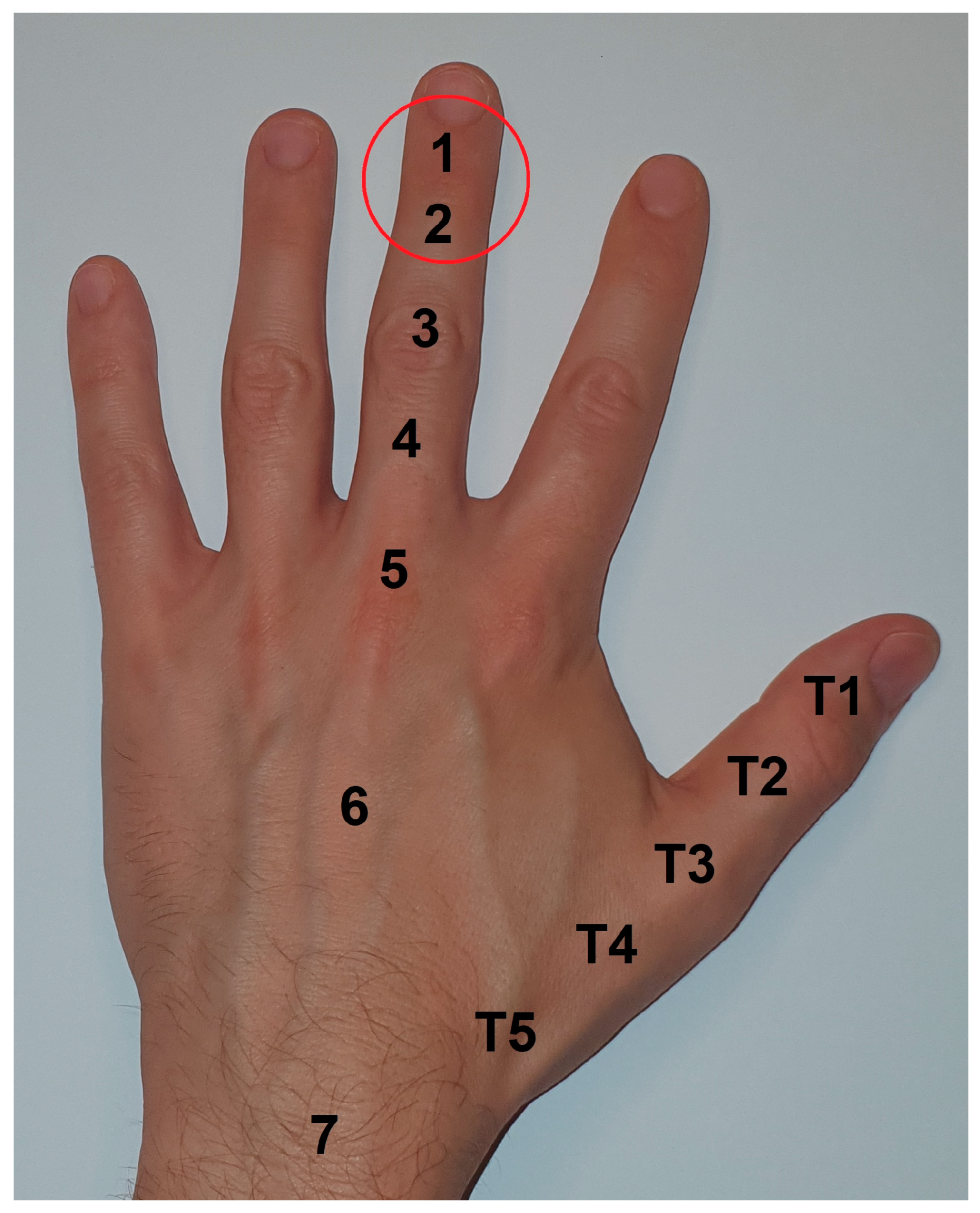
2. Materials and Methods
2.1. Study Design
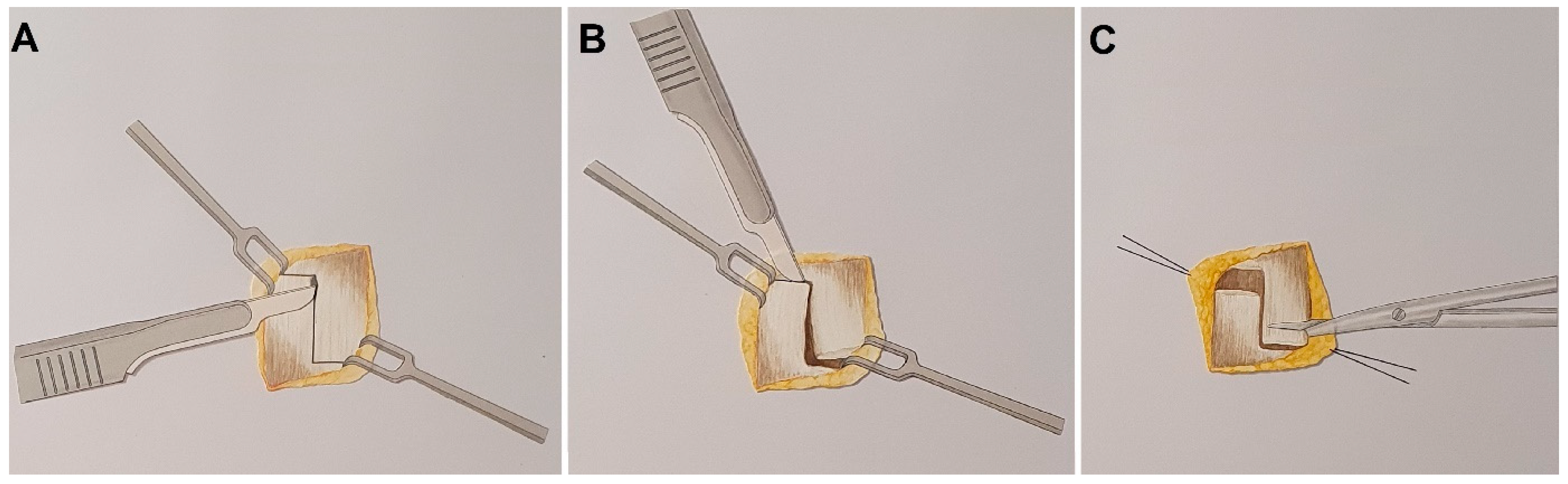
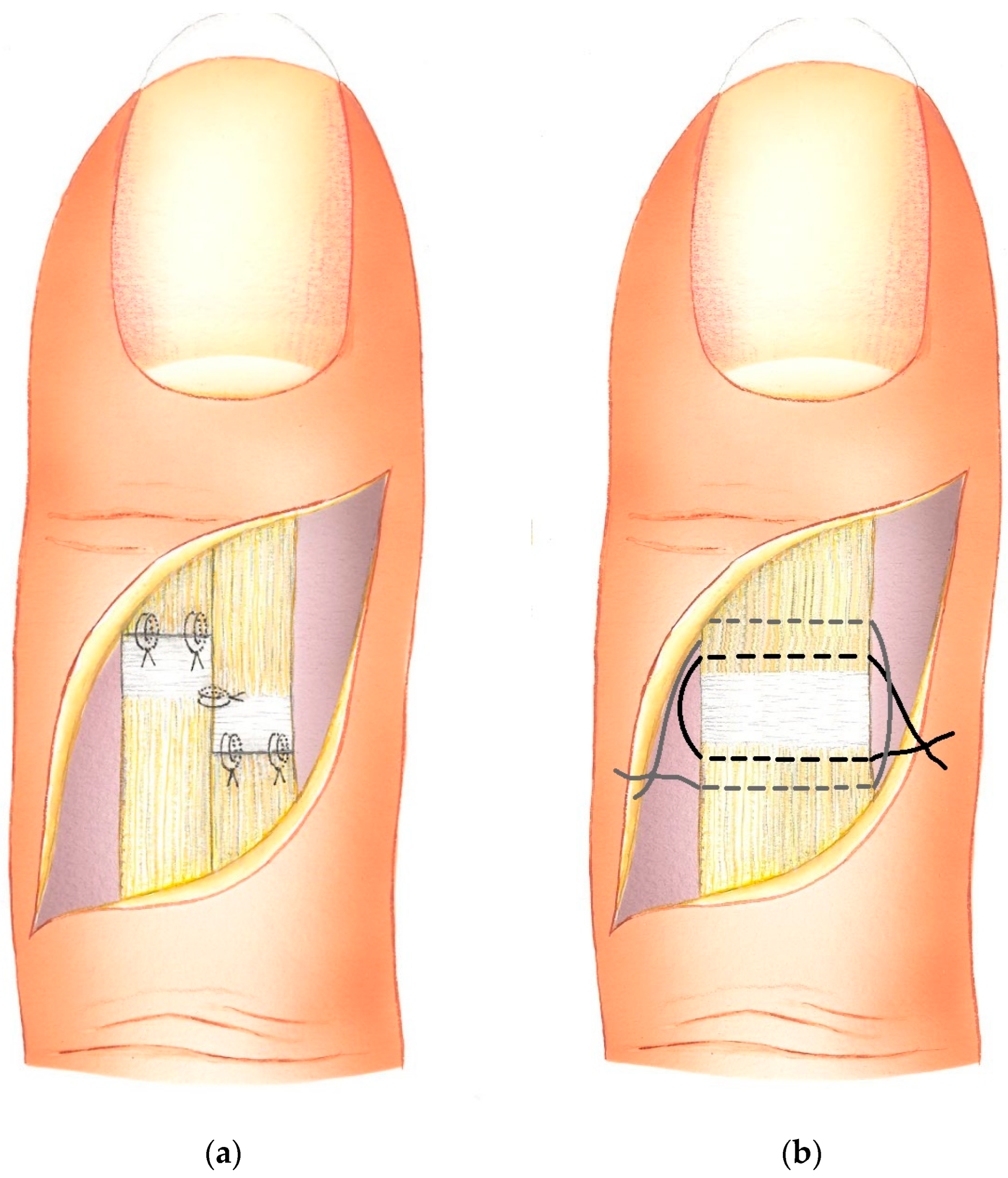
2.2. Surgical Procedures
2.3. Postoperative Care
3. Results
Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bendre, A.A.; Hartigan, B.J.; Kalainov, D.M. Mallet finger. J. Am. Acad. Orthop. Surg. 2005, 13, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Ramponi, D.R.; Hellier, S.D. Mallet Finger. Adv. Emerg. Nurs. J. 2019, 41, 198–203. [Google Scholar] [CrossRef]
- Doyle, J.R. Extensor Tendons: Acute Injuries, 4th ed.; Green, D.P., Ed.; Churchill Livingstone: New York, NY, USA, 1999; p. 4. [Google Scholar]
- Wehbe, M.A.; Schneider, L.H. Mallet fractures. J. Bone Jt. Surg. Am. 1984, 66, 658–669. [Google Scholar] [CrossRef] [PubMed]
- Alla, S.R.; Deal, N.D.; Dempsey, I.J. Current concepts: Mallet finger. Hand 2014, 9, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Khera, B.; Chang, C.; Bhat, W. An overview of mallet finger injuries. Acta Biomed. 2021, 92, e2021246. [Google Scholar]
- Garberman, S.F.; Diao, E.; Peimer, C.A. Mallet finger: Results of early versus delayed closed treatment. J. Hand Surg. Am. 1994, 19, 850–852. [Google Scholar] [CrossRef] [PubMed]
- Kalainov, D.M.; Hoepfner, P.E.; Hartigan, B.J.; Carroll, C.t.; Genuario, J. Nonsurgical treatment of closed mallet finger fractures. J. Hand Surg. Am. 2005, 30, 580–586. [Google Scholar] [CrossRef]
- Patel, M.R.; Desai, S.S.; Bassini-Lipson, L. Conservative management of chronic mallet finger. J. Hand Surg. Am. 1986, 11, 570–573. [Google Scholar] [CrossRef]
- Valdes, K.; Naughton, N.; Algar, L. Conservative treatment of mallet finger: A systematic review. J. Hand Ther. 2015, 28, 237–245, quiz 246. [Google Scholar] [CrossRef]
- Meals, R.A. Mallet Finger Treatment & Management. 2024. Available online: https://emedicine.medscape.com/article/1242305-treatment?form=fpf (accessed on 19 August 2024).
- Lamaris, G.A.; Matthew, M.K. The Diagnosis and Management of Mallet Finger Injuries. Hand 2017, 12, 223–228. [Google Scholar] [CrossRef]
- Nakamura, K.; Nanjyo, B. Reassessment of surgery for mallet finger. Plast. Reconstr. Surg. 1994, 93, 141–149, discussion 150-141. [Google Scholar] [CrossRef]
- Georg, H. Zur Behandlung des geschlossenen Strecksehnenabrisses am Fingerendglied. Langenbecks Arch. Klin. Chir. 1959, 292, 485–486. [Google Scholar] [CrossRef]
- Lind, J.; Hansen, L.B. Abbrevatio: A new operation for chronic mallet finger. J. Hand Surg. Br. 1989, 14, 347–349. [Google Scholar] [CrossRef]
- Iselin, F.; Levame, J.; Godoy, J. A simplified technique for treating mallet fingers: Tenodermodesis. J. Hand Surg. Am. 1977, 2, 118–121. [Google Scholar] [CrossRef]
- Shin, E.K.; Bae, D.S. Tenodermodesis for chronic mallet finger deformities in children. Tech. Hand Up. Extrem. Surg. 2007, 11, 262–265. [Google Scholar] [CrossRef]
- Thompson, J.S.; Littler, J.W.; Upton, J. The spiral oblique retinacular ligament (SORL). J. Hand Surg. Am. 1978, 3, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Katzman, S.S.; Gibeault, J.D.; Dickson, K.; Thompson, J.D. Use of a Herbert screw for interphalangeal joint arthrodesis. Clin. Orthop. Relat. Res. 1993, 296, 127–132. [Google Scholar] [CrossRef]
- Kleinert, H.E.; Verdan, C. Report of the Committee on Tendon Injuries (International Federation of Societies for Surgery of the Hand). J. Hand Surg. Am. 1983, 8, 794–798. [Google Scholar] [CrossRef]
- Diao, E.; Hariharan, J.S.; Soejima, O.; Lotz, J.C. Effect of peripheral suture depth on strength of tendon repairs. J. Hand Surg. Am. 1996, 21, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.D. Principles and Techniques of Tendon and Ligament Repair; The Podiatry Institute: Decatur, GA, USA, 2010; pp. 290–294. Available online: www.podiatryinstitute.com/pdfs/Update_2010/2010_52.pdf (accessed on 1 August 2024).
- Baumeister, R.G.; Hofmann, T. Step-plasty for therapy of chronic subcutaneous ruptures of extensor tendons of finger end joints. Handchir. Mikrochir. Plast. Chir. 1992, 24, 292–295. [Google Scholar] [PubMed]
- Debrunner, H.U. Gelenkmessung (Neutral-0-Methode), Längenmessung, Umfangmessung; Bulletin des Offiziellen Organs der Arbeitsgemein-schaft für Osteosynthesefragen: Bern, Switzerland, 1971. [Google Scholar]
- Gajdosik, R.L.; Bohannon, R.W. Clinical measurement of range of motion. Review of goniometry emphasizing reliability and validity. Phys. Ther. 1987, 67, 1867–1872. [Google Scholar] [CrossRef]
- Crawford, G.P. The molded polythene splint for mallet finger deformities. J. Hand Surg. Am. 1984, 9, 231–237. [Google Scholar] [CrossRef]
- Levante, S.; Belkadi, A.; Ebelin, M. Surgical treatment of chronic mallet finger by shortening–suture of the tendon scar. Sixty six cases. Chir. Main 2003, 22, 13–18. [Google Scholar] [CrossRef]
- Elliot, D.; McGrouther, D.A. The excursions of the long extensor tendons of the hand. J. Hand Surg. Br. 1986, 11, 77–80. [Google Scholar] [CrossRef]
- Burton, R.I. Extensor Tendons: Late Reconstruction, 5th ed.; Churchill Livingstone: New York, NY, USA, 1988. [Google Scholar]
- Ulusoy, M.G.; Karalezli, N.; Kocer, U.; Uysal, A.; Karaaslan, O.; Kankaya, Y.; Aslan, C. Pull-in suture technique for the treatment of mallet finger. Plast. Reconstr. Surg. 2006, 118, 696–702. [Google Scholar] [CrossRef]
- Hume, M.C.; Gellman, H.; McKellop, H.; Brumfield, R.H., Jr. Functional range of motion of the joints of the hand. J. Hand Surg. Am. 1990, 15, 240–243. [Google Scholar] [CrossRef]
- Geyman, J.P.; Fink, K.; Sullivan, S.D. Conservative versus surgical treatment of mallet finger: A pooled quantitative literature evaluation. J. Am. Board. Fam. Pract. 1998, 11, 382–390. [Google Scholar] [CrossRef] [PubMed]
| Crawfords’s Evaluation Criteria (1984) [26] | |||||
|---|---|---|---|---|---|
| Grade | Excellent | Good | Fair | Poor | |
| Description | Full DIP joint extension, full flexion, no pain | 0–10 degrees of extension deficit, full, flexion, no pain | 10–25 degrees of extension deficit, any flexion loss, no pain | More than 25 degrees of extension deficit, or persistent pain | |
| Levantes’s Evaluation Criteria (2003) [27] | |||||
| Grade | Very good | Good | Middle | Bad | Failure |
| Description | ED < 5°, CAM > 60° | ED < 15°, CAM > 50° | ED < 25°, CAM > 40° | ED < 35°, CAM > 30° | ED < 40°, CAM < 20° |
| Operative Procedure | Excellent | Good | Fair | Poor | Complications |
|---|---|---|---|---|---|
| step-plasty | 10 24% | 17 41% | 12 28% | 3 7% | 2 (osteitis) 3%. |
| purse-string | 8 22% | 6 16% | 16 43% | 7 19% | 1 (dystrophic reaction) |
| Operative Procedure | Very Good | Good | Middle | Bad | Failure |
|---|---|---|---|---|---|
| step-plasty | 10 24% | 18 42% | 7 17% | 7 17% | - - |
| purse-string | 7 19% | 7 19% | 14 37% | 6 17% | 3 8% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demmer, W.; Frick, A.; Baumeister, R.G.H.; Haas-Lützenberger, E.; Thierfelder, N.; Mert, S.; Ehrl, D.; Giunta, R.; Stäuble, C.G. Reconstruction of Chronic Soft Tissue Mallet Fingers: Outcomes of Step-Plasty vs. Purse-String Suture. J. Funct. Morphol. Kinesiol. 2024, 9, 144. https://doi.org/10.3390/jfmk9030144
Demmer W, Frick A, Baumeister RGH, Haas-Lützenberger E, Thierfelder N, Mert S, Ehrl D, Giunta R, Stäuble CG. Reconstruction of Chronic Soft Tissue Mallet Fingers: Outcomes of Step-Plasty vs. Purse-String Suture. Journal of Functional Morphology and Kinesiology. 2024; 9(3):144. https://doi.org/10.3390/jfmk9030144
Chicago/Turabian StyleDemmer, Wolfram, Andreas Frick, Rüdiger G. H. Baumeister, Elisabeth Haas-Lützenberger, Nikolaus Thierfelder, Sinan Mert, Denis Ehrl, Riccardo Giunta, and Christiane G. Stäuble. 2024. "Reconstruction of Chronic Soft Tissue Mallet Fingers: Outcomes of Step-Plasty vs. Purse-String Suture" Journal of Functional Morphology and Kinesiology 9, no. 3: 144. https://doi.org/10.3390/jfmk9030144
APA StyleDemmer, W., Frick, A., Baumeister, R. G. H., Haas-Lützenberger, E., Thierfelder, N., Mert, S., Ehrl, D., Giunta, R., & Stäuble, C. G. (2024). Reconstruction of Chronic Soft Tissue Mallet Fingers: Outcomes of Step-Plasty vs. Purse-String Suture. Journal of Functional Morphology and Kinesiology, 9(3), 144. https://doi.org/10.3390/jfmk9030144






