Stretching and Releasing of Iliotibial Band Complex in Patients with Iliotibial Band Syndrome: A Narrative Review
Abstract
1. Introduction
2. Methods
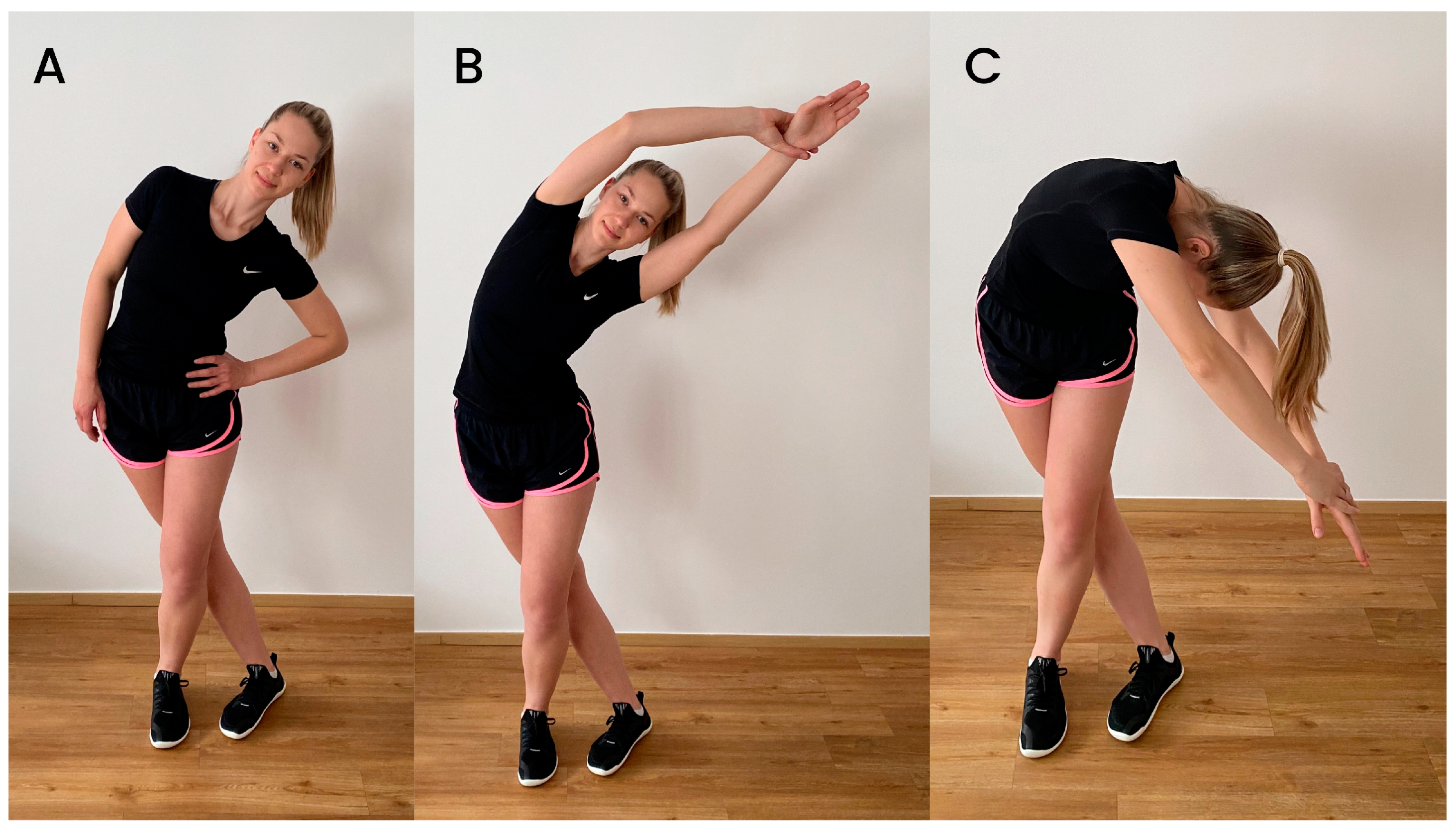
3. Methods of Stretching and Releasing ITB–TFL Complex
4. In Vitro and In Vivo Behavior Responses of Iliotibial Band to Stretching
5. Iliotibial Band Syndrome Etiology and Risk Factors
6. Clinical Studies Examining the Effects of ITB Stretching and Other Methods Purported to Stretch or “Release” the ITB
6.1. Effects on Pain
| Author (Year) | Population | Purpose | Intervention | Findings |
|---|---|---|---|---|
| Pepper et al., 2021 [27] | Healthy adults (18–50 years) with no ITBS history | To compare the immediate effects of stretching and foam rolling on ITB stiffness. | Stretching: Three bouts of a 7 s submaximal contraction in hip abduction followed by a 15 s stretch. FR: Five 3 min repetitions | No effects of either intervention on ITB stiffness, despite increases in hip RoM. |
| McKay et al., 2020 [24] | Female distance runners (19–45 years) with unilateral ITBS for at least 3 months | To assess the effectiveness of three different exercise regimens (stretching, conventional hip rehabilitation, and experimental exercises, which involve progressive increase in complexity) in female runners with ITBS. | Stretching (progressive stretching program included four ITB stretches that were held for 30–40 s and repeated 2–4 times, three times per week). Group B: Conventional exercise (focusing on hip muscles) Experimental hip strengthening exercise. The intervention lasted for eight weeks. | There were no statistical differences between the three groups. Nonsignificant improvement in pain was observed after stretching intervention. ITB stretching was reported to improve Y-balance test performance and movement quality in the single-leg mini-squat. |
| Afshari et al., 2023 [29] | Semi-elite athletes (20–40 years) with ITB shortness confirmed by the modified Ober’s test | To investigate the effect of active stretching techniques and self-myofascial release on improving the ITB flexibility and functional performance of athletes. | FR: foam rolling took about 3 min. PNF active stretching: contraction–relaxation technique for 3–5 min. Combination of FR/PNF | The mean of the active hip adduction RoM, single-leg hop test, lateral hop test, and vertical jump in all three groups increased significantly after the intervention compared to before. All three studied groups had similar changes over time, and no group was superior to the others. |
| Kasunich, 2003 [30] | Case report: long-distance runner (38 years) with low-back pain and sacroiliac pain and proposes ITB tightness as a possible causative factor | To investigate the effects of a multimodal therapy based on stretching and release methods on a single patient. | Chiropractic manipulative therapy, trigger point therapy and stretching of the ITB (once per day during first two weeks and twice per day during second two weeks, in side-lying position). The intervention lasted for 4 weeks. | The patient did not demonstrate much improvement until extensive stretching was included in the treatment plan. It is important to consider ITB tightness as a possible cause of low back and sacroiliac pain. |
| Friede et al., 2020 [32] | Recreational runners with ITBS and healthy controls (18–45 years) | To test ITB stiffness and isometric hip muscle strength in a sample of subjects clinically diagnosed with ITBS for comparison with a healthy control group, and to assess the effectiveness of a multimodal training program in strengthening the hip abductor and external rotator muscles and modulating ITB tone. | The intervention lasted for 6 weeks and consisted of: myofascial techniques addressing trigger points, strengthening exercises (for gluteal muscles and hip external rotators), stretching (twice a day, two sets of 60 s duration, 30 s inter-set break), foam rolling (three times for 60 s, 30 s break between sets). Intervention also consisted of measures aiming to improve neuromuscular control and lower extremity alignment during gait and running. | ITB tension is not increased in the affected legs of runners with ITBS compared to the healthy leg or a physical active control group, respectively. Following six weeks of physiotherapy, hip muscle strength (all directions but abduction), pain and lower extremity function were significantly improved. ITB stiffness was found to be increased compared to baseline measurements. |
| Sharp et al., 2012 [36] | Asymptomatic male non-professional rugby players (19–30 years) | To compare the relative effectiveness of two myofascial release techniques for the ITB: self-myofascial release (foam rolling), and Emmett technique. | Emmet technique used on the “ITB site” and the “sartorius and ITB site” (lasted for 5 min). FR: focused on TFL and ITB area, left and right side were treated (there was a maximum time of 60–90 s allocated for each region). Control: no intervention. | No significant improvements in active hip adduction RoM were observed after foam rolling. Emmet technique appeared to be more effective in hip RoM increase (2% increase in hip RoM after FR, 70% increase after Emmet technique). No significant effect of FR and Emmett technique on vertical jump height during countermovement jump was observed. |
| Park et al., 2022 [39] | Men cycling club members (20–45 years) with ITBS | To investigate the effect of one-time self-myofascial release using a foam roller via special tests, visual analog scale (VAS), and exercise performance on adult male cycling club members diagnosed with ITBS. | After the first 10 km cycling course, the control group had a static rest for 120 min. The FR group conducted the intervention using a foam roller for 20 min after a static rest of 100 min, and then both groups underwent a post-cycling special test after the second cycling on the same course. | Significant differences were observed in the FR group in VAS through Nobel’s compression test, ITB flexibility through Ober’s test, and VAS and power while cycling. No significant difference was observed in HR, cadence, and record time. |
| Pedowitz, 2005 [40] | Case report: 30-year-old distance runner with ITBS | To investigate the potential of osteopathic manipulative technique (OMT) called counterstrain on a single-case basis. | The intervention lasted for 2 weeks with OMT applied every 2 to 3 days. | One week after intervention the patient reported that he had been feeling well and had returned to his normal, full running activity by day. He also stated that he had been free of pain and feeling happier overall. His ability to perform the regular activities of daily life had improved. |
| Else and Moodley, 2010 [38] | Active runners or cyclists with ITBS and active or latent trigger points in the ITB (18–60 years) | To determine whether foam roller treatment of the ITB can be used as an effective treatment for ITBS in cyclists and runners and whether it is better to be used alone or in conjunction with spinal manipulation. | Intervention lasted for 3 weeks (6 treatment consultations). Group one: combination of both treatments. Group two: foam rolling (they held their weight over the foam roller on painful area for minimum of 120 s). Group three: lumbar spinal manipulation to the restricted segments. | Combination group showed the best improvement consistently across all forms of measurement. Group three had the smallest increase in overall improvement subjectively and objectively. All three treatment protocols were equally effective in treating ITBS as demonstrated by the statistically significant results. |
| Vaughan et al., 2014 [37] | Student asymptomatic population (both genders, mean age of 26.1 ± 6.7 years) | To investigate the effects of the application of a foam roller for three minutes to the right iliotibial band (ITB) of asymptomatic participants. | A three-minute session on the foam roller. | Results demonstrate a statistically significant increase in the pain pressure threshold at the lower thighimmediately post-bout; however, the difference was ameliorated five minutes later. |
| Mayer et al., 2020 [65] | Experienced (regarding FR) and nonexperienced athletes (healthy; both genders; 18–65 years) | To investigate muscle-specific and connective tissue-specific responses after FR in recreational athletes with different foam rolling experience. | FR: 5 trials per 45 s of foam rolling with 20 s of rest between each trial. | In experienced athletes, tissue stiffness of the ITB revealed a significant decrease of 13.2% at post-intervention (t1 = after 0 min) and 12.1% 6 h after intervention (=t3). In nonexperienced athletes, a 6.2% increase in stiffness was found at t1, which was not significantly different to baseline. For both groups, no significant ITB stiffness changes were found at further time points (30 min, 6 h or 24 h after intervention). |
6.2. Effects on Stiffness
6.3. Effects on Hip RoM
6.4. Effects on Function and Performance
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Der Worp, M.P.; Van Der Horst, N.; De Wijer, A.; Backx, F.J.G.; Van Der Sanden, M.W.G.N. Iliotibial Band Syndrome in Runners: A Systematic Review. Sports Med. 2012, 42, 969–992. [Google Scholar] [CrossRef] [PubMed]
- Taunton, J.E.; Ryan, M.B.; Clement, D.B.; McKenzie, D.C.; Lloyd-Smith, D.R.; Zumbo, B.D. A Retrospective Case-Control Analysis of 2002 Running Injuries. Br. J. Sports Med. 2002, 36, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Lavine, R. Iliotibial Band Friction Syndrome. Curr. Rev. Musculoskelet. Med. 2010, 3, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Benca, E.; Listabarth, S.; Flock, F.K.J.; Pablik, E.; Fischer, C.; Walzer, S.M.; Dorotka, R.; Windhager, R.; Ziai, P. Analysis of Running-Related Injuries: The Vienna Study. J. Clin. Med. 2020, 9, 438. [Google Scholar] [CrossRef] [PubMed]
- Holmes, J.C.; Pruitt, A.L.; Whalen, N.J. Iliotibial Band Syndrome in Cyclists. Am. J. Sports Med. 1993, 21, 419–424. [Google Scholar] [CrossRef]
- Devan, M.; Pescatello, L.; Faghri, P.; Anderson, J. A Prospective Study of Overuse Knee Injuries among Female Athletes with Muscle Imbalances and Structural Abnormalities. J. Athl. Train. 2004, 39, 263–267. [Google Scholar]
- Rumball, J.S.; Lebrun, C.M.; Di Ciacca, S.R.; Orlando, K. Rowing Injuries. Sports Med. 2005, 35, 537–555. [Google Scholar] [CrossRef]
- Martinez-Velez, A.; Suwan, P.; Dua, A. Iliotibial Band Syndrome in Non-Athletes. Minerva Anestesiol. 2020, 86, 1111–1112. [Google Scholar] [CrossRef]
- Beals, C.; Flanigan, D. A Review of Treatments for Iliotibial Band Syndrome in the Athletic Population. J. Sports Med. 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Bolia, I.K.; Gammons, P.; Scholten, D.J.; Weber, A.E.; Waterman, B.R. Operative Versus Nonoperative Management of Distal Iliotibial Band Syndrome—Where Do We Stand? A Systematic Review. Arthrosc. Sports Med. Rehabil. 2020, 2, e399–e415. [Google Scholar] [CrossRef]
- Charles, D.; Rodgers, C. A Literature Review and Clinical Commentary on the Development of Iliotibial Band Syndrome in Runners. Int. J. Sports Phys. Ther. 2020, 15, 460–470. [Google Scholar] [CrossRef] [PubMed]
- Messier, S.P.; Edwards, D.G.; Martin, D.F.; Lowery, R.B.; Cannon, D.W.; James, M.K.; Curl, W.W.; Read, H.M.; Hunter, D.M. Etiology of Iliotibial Band Friction Syndrome in Distance Runners. Med. Sci. Sports Exerc. 1995, 27, 951–960. [Google Scholar] [CrossRef]
- Fairclough, J.; Hayashi, K.; Toumi, H.; Lyons, K.; Bydder, G.; Phillips, N.; Best, T.M.; Benjamin, M. Is Iliotibial Band Syndrome Really a Friction Syndrome? J. Sci. Med. Sport 2007, 10, 74–76. [Google Scholar] [CrossRef] [PubMed]
- Aderem, J.; Louw, Q.A. Biomechanical Risk Factors Associated with Iliotibial Band Syndrome in Runners: A Systematic Review. BMC Musculoskelet. Disord. 2015, 16, 356. [Google Scholar] [CrossRef] [PubMed]
- Grau, S.; Krauss, I.; Maiwald, C.; Best, R.; Horstmann, T. Hip Abductor Weakness Is Not the Cause for Iliotibial Band Syndrome. Int. J. Sports Med. 2008, 29, 579–583. [Google Scholar] [CrossRef] [PubMed]
- Friede, M.C.; Innerhofer, G.; Fink, C.; Alegre, L.M.; Csapo, R. Conservative Treatment of Iliotibial Band Syndrome in Runners: Are We Targeting the Right Goals? Phys. Ther. Sport 2022, 54, 44–52. [Google Scholar] [CrossRef]
- Hadeed, A.; Tapscott, D.C. Iliotibial Band Friction Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Strauss, E.J.; Kim, S.; Calcei, J.G.; Park, D. Iliotibial Band Syndrome: Evaluation and Management. Am. Acad. Orthop. Surg. 2011, 19, 728–736. [Google Scholar] [CrossRef]
- Khaund, R.; Flynn, S. Iliotibial Band Syndrome: A Common Source of Knee Pain. Am. Fam. Physician 2005, 71, 1545–1550. [Google Scholar]
- McGuine, T.A.; Winterstein, A.P.; Carr, K.; Hetzel, S. Changes in Health-Related Quality of Life and Knee Function After Knee Injury in Young Female Athletes. Orthop. J. Sports Med. 2014, 2, 232596711453098. [Google Scholar] [CrossRef]
- Maghroori, R.; Karshenas, L.; Khosrawi, S. Shockwave Therapy Versus Dry Needling for the Management of Iliotibial Band Syndrome: A Randomized Clinical Trial. Galen Med. J. 2021, 10, e2174. [Google Scholar] [CrossRef]
- Watcharakhueankhan, P.; Chapman, G.J.; Sinsurin, K.; Jaysrichai, T.; Richards, J. The Immediate Effects of Kinesio Taping on Running Biomechanics, Muscle Activity, and Perceived Changes in Comfort, Stability and Running Performance in Healthy Runners, and the Implications to the Management of Iliotibial Band Syndrome. Gait Posture 2022, 91, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Fredericson, M.; Wolf, C. Iliotibial Band Syndrome in Runners. Sports Med. 2005, 35, 451–459. [Google Scholar] [CrossRef] [PubMed]
- McKay, J.; Maffulli, N.; Aicale, R.; Taunton, J. Iliotibial Band Syndrome Rehabilitation in Female Runners: A Pilot Randomized Study. J. Orthop. Surg. Res. 2020, 15, 188. [Google Scholar] [CrossRef] [PubMed]
- Beers, A.; Ryan, M.; Kasubuchi, Z.; Fraser, S.; Taunton, J.E. Effects of Multi-Modal Physiotherapy, Including Hip Abductor Strengthening, in Patients with Iliotibial Band Friction Syndrome. Physiother. Can. 2008, 60, 180–188. [Google Scholar] [CrossRef]
- Fredericson, M.; White, J.J.; MacMahon, J.M.; Andriacchi, T.P. Quantitative Analysis of the Relative Effectiveness of 3 Iliotibial Band Stretches. Arch. Phys. Med. Rehabil. 2002, 83, 589–592. [Google Scholar] [CrossRef]
- Pepper, T.M.; Brismée, J.M.; Sizer, P.S.; Kapila, J.; Seeber, G.H.; Huggins, C.A.; Hooper, T.L. The Immediate Effects of Foam Rolling and Stretching on Iliotibial Band Stiffness: A Randomized Controlled Trial. Int. J. Sports Phys. Ther. 2021, 16, 651–661. [Google Scholar] [CrossRef]
- Tateuchi, H.; Shiratori, S.; Ichihashi, N. The Effect of Three-Dimensional Postural Change on Shear Elastic Modulus of the Iliotibial Band. J. Electromyogr. Kinesiol. 2016, 28, 137–142. [Google Scholar] [CrossRef]
- Afshari, E.; Kajbafvala, M.; Mohsenifar, H.; Abbasi, L. Comparison of the Immediate Effect of Active Stretching Techniques and Self-Myofascial Release on the Flexibility of the Iliotibial Band and Functional Activities in Semi-Elite Athletes: A Randomized Clinical Trial. Middle East J. Rehabil. Health Stud. 2023, 10, e134802. [Google Scholar] [CrossRef]
- Kasunich, N.J. Changes in Low Back Pain in a Long Distance Runner after Stretching the Iliotibial Band. J. Chiropr. Med. 2003, 2, 37–40. [Google Scholar] [CrossRef]
- McConnel, J.; Fulkerson, J. The Knee: Patellofemoral Ad Soft Tissue Injuries. In Athletic Injuries and Rehabilitation; Zachazweski, J., Magee, D., Quillen, W., Eds.; W.B. Saunders Co.: Philadelphia, PA, USA, 1996; p. 721. [Google Scholar]
- Friede, M.C.; Klauser, A.; Fink, C.; Csapo, R. Stiffness of the Iliotibial Band and Associated Muscles in Runner’s Knee: Assessing the Effects of Physiotherapy through Ultrasound Shear Wave Elastography. Phys. Ther. Sport 2020, 45, 126–134. [Google Scholar] [CrossRef]
- Thomas, E.; Bianco, A.; Paoli, A.; Palma, A. The Relation between Stretching Typology and Stretching Duration: The Effects on Range of Motion. Int. J. Sports Med. 2018, 39, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Curran, P.F.; Fiore, R.D.; Crisco, J.J. A Comparison of the Pressure Exerted on Soft Tissue by 2 Myofascial Rollers. J. Sport Rehabil. 2008, 17, 432–442. [Google Scholar] [CrossRef]
- MacDonald, G.Z.; Penney, M.D.H.; Mullaley, M.E.; Cuconato, A.L.; Drake, C.D.J.; Behm, D.G.; Button, D.C. An Acute Bout of Self-Myofascial Release Increases Range of Motion Without a Subsequent Decrease in Muscle Activation or Force. J. Strength Cond. Res. 2013, 27, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Sharp, V. A Comparative Study Between Self Myofascial Release and Emmett Technique Effectiveness in the Management of Fascial (Iliotibial Band) Tightness. Bachelor’s Thesis, Queen’s University, Kingston, ON, Canada, 2012. [Google Scholar]
- Vaughan, B.; McLaughlin, P.; Lepley, A.S. Immediate Changes in Pressure Pain Threshold in the Iliotibial Band Using a Myofascial (Foam) Roller. Int. J. Ther. Rehabil. 2014, 21, 569–574. [Google Scholar] [CrossRef]
- Else, J.; Moodley, M. The Effectiveness of Foam Rolling Treatment Versus Chiropractic Manipulative Therapy in the Management of Iliotibial Band Friction Syndrome in Runners and Cyclists. Master’s Thesis, University of Johannesburg, Johannesburg, South Africa, 2010. [Google Scholar]
- Park, J.J.; Lee, H.S.; Kim, J.-H. Effect of Acute Self-Myofascial Release on Pain and Exercise Performance for Cycling Club Members with Iliotibial Band Friction Syndrome. Int. J. Environ. Res. Public Health 2022, 19, 15993. [Google Scholar] [CrossRef]
- Pedowitz, R.N. Use of Osteopathic Manipulative Treatment for Iliotibial Band Friction Syndrome. J. Am. Osteopath. Assoc. 2005, 105, 563–567. [Google Scholar]
- Falvey, E.C.; Clark, R.A.; Franklyn-Miller, A.; Bryant, A.L.; Briggs, C.; McCrory, P.R. Iliotibial Band Syndrome: An Examination of the Evidence behind a Number of Treatment Options. Scand. J. Med. Sci. Sports 2010, 20, 580–587. [Google Scholar] [CrossRef]
- Wilhelm, M.; Matthijs, O.; Browne, K.; Seeber, G.; Matthijs, A.; Sizer, P.S.; Brismée, J.-M.; James, C.R.; Gilbert, K.K. Deformation Response of the Iliotibial Band-Tensor Fascia Lata Complex to Clinical-Grade Longitudinal Tension Loading in-Vitro. Int. J. Sports Phys. Ther. 2017, 12, 16–24. [Google Scholar]
- Seeber, G.H.; Wilhelm, M.P.; Sizer, P.S., Jr.; Guthikonda, A.; Matthijs, A.; Matthijs, O.C.; Lazovic, D.; Brismée, J.; Gilbert, K.K. The Tensile Behaviors of the Iliotibial Band—A Cadaveric Investigation. Int. J. Sports Phys. Ther. 2020, 15, 451–459. [Google Scholar] [CrossRef]
- Wang, H.K.; Ting-Fang Shih, T.; Lin, K.H.; Wang, T.G. Real-Time Morphologic Changes of the Iliotibial Band during Therapeutic Stretching; an Ultrasonographic Study. Man. Ther. 2008, 13, 334–340. [Google Scholar] [CrossRef]
- Besomi, M.; Salomoni, S.E.; Hug, F.; Tier, L.; Vicenzino, B.; Hodges, P.W. Exploration of Shear Wave Elastography Measures of the Iliotibial Band during Different Tasks in Pain-Free Runners. Phys. Ther. Sport 2021, 50, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Orchard, J.W.; Fricker, P.A.; Abud, A.T.; Mason, B.R. Biomechanics of Iliotibial Band Friction Syndrome in Runners. Am. J. Sports Med. 1996, 24, 375–379. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, J.; Hayashi, K.; Toumi, H.; Lyons, K.; Bydder, G.; Phillips, N.; Best, T.M.; Benjamin, M. The Functional Anatomy of the Iliotibial Band during Flexion and Extension of the Knee: Implications for Understanding Iliotibial Band Syndrome. J. Anat. 2006, 208, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Everhart, J.S.; Kirven, J.C.; Higgins, J.; Hair, A.; Chaudhari, A.A.M.W.; Flanigan, D.C. The Relationship between Lateral Epicondyle Morphology and Iliotibial Band Friction Syndrome: A Matched Case–Control Study. Knee 2019, 26, 1198–1203. [Google Scholar] [CrossRef]
- Stickley, C.D.; Presuto, M.M.; Radzak, K.N.; Bourbeau, C.M.; Hetzler, R.K. Dynamic Varus and the Development of Iliotibial Band Syndrome. J. Athl. Train. 2018, 53, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Ferber, R.; Noehren, B.; Hamill, J.; Davis, I. Competitive Female Runners with a History of Iliotibial Band Syndrome Demonstrate Atypical Hip and Knee Kinematics. J. Orthop. Sports Phys. Ther. 2010, 40, 52–58. [Google Scholar] [CrossRef]
- Noehren, B.; Davis, I.; Hamill, J. ASB Clinical Biomechanics Award Winner 2006. Prospective Study of the Biomechanical Factors Associated with Iliotibial Band Syndrome. Clin. Biomech. 2007, 22, 951–956. [Google Scholar] [CrossRef]
- Brown, A.M.; Zifchock, R.A.; Hillstrom, H.J.; Song, J.; Tucker, C.A. The Effects of Fatigue on Lower Extremity Kinematics, Kinetics and Joint Coupling in Symptomatic Female Runners with Iliotibial Band Syndrome. Clin. Biomech. 2016, 39, 84–90. [Google Scholar] [CrossRef]
- Foch, E.; Aubol, K.; Milner, C.E. Relationship between Iliotibial Band Syndrome and Hip Neuromechanics in Women Runners. Gait Posture 2020, 77, 64–68. [Google Scholar] [CrossRef]
- Dos Anjos Rabelo, N.D.; Lucareli, P.R.G. Do Hip Muscle Weakness and Dynamic Knee Valgus Matter for the Clinical Evaluation and Decision-Making Process in Patients with Patellofemoral Pain? Braz. J. Phys. Ther. 2018, 22, 105–109. [Google Scholar] [CrossRef]
- Eng, C.M.; Arnold, A.S.; Lieberman, D.E.; Biewener, A.A. The Capacity of the Human Iliotibial Band to Store Elastic Energy during Running. J. Biomech. 2015, 48, 3341–3348. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, J.R.; MacIntosh, B.R. Changes in Achilles Tendon Stiffness and Energy Cost Following a Prolonged Run in Trained Distance Runners. PLoS ONE 2018, 13, e0202026. [Google Scholar] [CrossRef] [PubMed]
- Noehren, B.; Schmitz, A.; Hempel, R.; Westlake, C.; Black, W. Assessment of Strength, Flexibility, and Running Mechanics in Men with Iliotibial Band Syndrome. J. Orthop. Sports Phys. Ther. 2014, 44, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Foch, E.; Reinbolt, J.A.; Zhang, S.; Fitzhugh, E.C.; Milner, C.E. Associations between Iliotibial Band Injury Status and Running Biomechanics in Women. Gait Posture 2015, 41, 706–710. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.-G.; Jan, M.-H.; Lin, K.-H.; Wang, H.-K. Assessment of Stretching of the Iliotibial Tract with Ober and Modified Ober Tests: An Ultrasonographic Study. Arch. Phys. Med. Rehabil. 2006, 87, 1407–1411. [Google Scholar] [CrossRef]
- Willett, G.M.; Keim, S.A.; Shostrom, V.K.; Lomneth, C.S. An Anatomic Investigation of the Ober Test. Am. J. Sports Med. 2016, 44, 696–701. [Google Scholar] [CrossRef]
- Baxter, C.; Mc Naughton, L.R.; Sparks, A.; Norton, L.; Bentley, D. Impact of Stretching on the Performance and Injury Risk of Long-Distance Runners. Res. Sports Med. 2017, 25, 78–90. [Google Scholar] [CrossRef]
- Lauersen, J.B.; Andersen, T.E.; Andersen, L.B. Strength Training as Superior, Dose-Dependent and Safe Prevention of Acute and Overuse Sports Injuries: A Systematic Review, Qualitative Analysis and Meta-Analysis. Br. J. Sports Med. 2018, 52, 1557–1563. [Google Scholar] [CrossRef]
- Lopez, P.; Radaelli, R.; Taaffe, D.R.; Newton, R.U.; Galvão, D.A.; Trajano, G.S.; Teodoro, J.L.; Kraemer, W.J.; Häkkinen, K.; Pinto, R.S. Resistance Training Load Effects on Muscle Hypertrophy and Strength Gain: Systematic Review and Network Meta-Analysis. Med. Sci. Sports Exerc. 2021, 53, 1206–1216. [Google Scholar] [CrossRef]
- Westcott, W.L. Resistance Training Is Medicine. Curr. Sports Med. Rep. 2012, 11, 209–216. [Google Scholar] [CrossRef]
- Mayer, I.; Hoppe, M.W.; Freiwald, J.; Heiss, R.; Engelhardt, M.; Grim, C.; Lutter, C.; Huettel, M.; Forst, R.; Hotfiel, T. Different Effects of Foam Rolling on Passive Tissue Stiffness in Experienced and Nonexperienced Athletes. J. Sport Rehabil. 2020, 29, 926–933. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Opara, M.; Kozinc, Ž. Stretching and Releasing of Iliotibial Band Complex in Patients with Iliotibial Band Syndrome: A Narrative Review. J. Funct. Morphol. Kinesiol. 2023, 8, 74. https://doi.org/10.3390/jfmk8020074
Opara M, Kozinc Ž. Stretching and Releasing of Iliotibial Band Complex in Patients with Iliotibial Band Syndrome: A Narrative Review. Journal of Functional Morphology and Kinesiology. 2023; 8(2):74. https://doi.org/10.3390/jfmk8020074
Chicago/Turabian StyleOpara, Manca, and Žiga Kozinc. 2023. "Stretching and Releasing of Iliotibial Band Complex in Patients with Iliotibial Band Syndrome: A Narrative Review" Journal of Functional Morphology and Kinesiology 8, no. 2: 74. https://doi.org/10.3390/jfmk8020074
APA StyleOpara, M., & Kozinc, Ž. (2023). Stretching and Releasing of Iliotibial Band Complex in Patients with Iliotibial Band Syndrome: A Narrative Review. Journal of Functional Morphology and Kinesiology, 8(2), 74. https://doi.org/10.3390/jfmk8020074






