Class II Skeletal Malocclusion and Prevalence of Temporomandibular Disorders. An Epidemiological Pilot Study on Growing Subjects
Abstract
1. Introduction
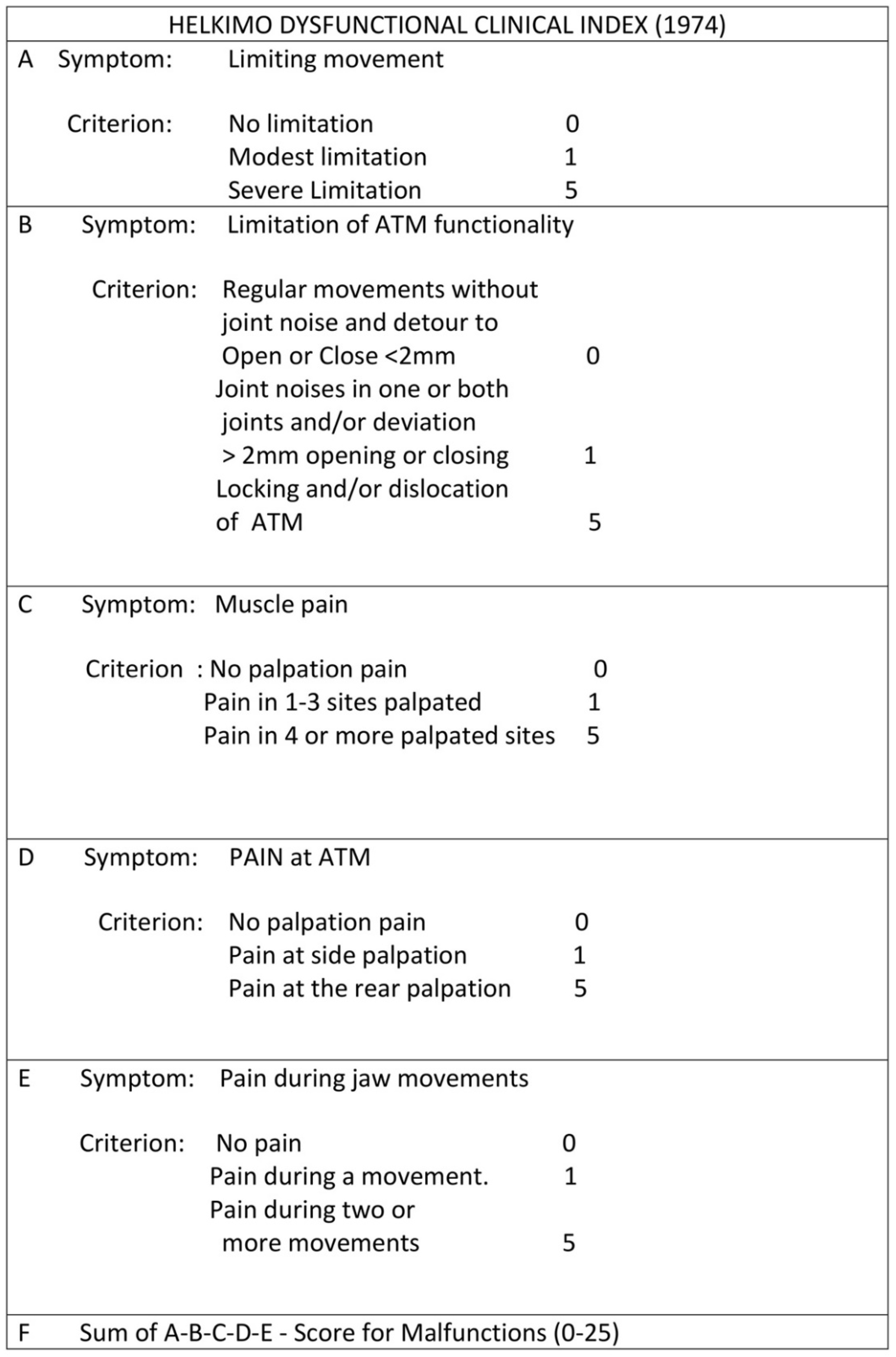
2. Materials and Methods
- 1.
- Inclusion Criteria
- (i)
- Patients with presence of skeletal Class I, Class II, or Class III;
- (ii)
- Patients who provided signed informed consent, according to the World.
- 2.
- Exclusion Criteria
- (i)
- History of trauma;
- (ii)
- Previous orthodontic and/or gnathologic and/or physical therapies;
- (iii)
- Presence of further structural malformations in the areas of interest;
- (iv)
- Presence of uncontrolled systemic disease.
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baccetti, T.; Franchi, L. Shape-coordinate and tensor analysis of skeletal changes in children with treated Class III malocclusions. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 622–633. [Google Scholar] [CrossRef]
- Baccetti, T.; Antonini, A.; Franchi, L.; Tonti, M.; Tollaro, I. Glenoid fossa position in different facial types: A cephalometric study. Br. J. Orthod. 1997, 24, 55–59. [Google Scholar] [CrossRef]
- Okeson, J.P.; de Kanter, R.J. Temporomandibular disorders in the medical practice. J. Fam. Pract. 1996, 43, 347–356. [Google Scholar] [PubMed]
- Helkimo, M. Studies on function and dysfunction of the masticatory system. I. An epidemiological investigation of symptoms of dysfunction in Lapps in the north of Finland. Proc. Finn. Dent. Soc. 1974, 70, 37–49. [Google Scholar] [PubMed]
- Costen, J.B. A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. 1934. Ann. Otol. Rhinol. Laryngol. 1997, 106, 805–819. [Google Scholar] [CrossRef] [PubMed]
- Riolo, M.L.; Brandt, D.; TenHave, T.R. Associations between occlusal characteristics and signs and symptoms of TMJ dysfunction in children and young adults. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 467–477. [Google Scholar] [CrossRef]
- Henrikson, T.; Ekberg, E.C.; Nilner, M. Symptoms and signs of temporomandibular disorders in girls with normal occlusion and Class II malocclusion. Acta Odontol. Scand. 1997, 55, 229–235. [Google Scholar] [CrossRef]
- Sonnesen, L.; Bakke, M.; Solow, B. Malocclusion traits and symptoms and signs of temporomandibular disorders in children with severe malocclusion. Eur. J. Orthod. 1998, 20, 543–559. [Google Scholar] [CrossRef]
- Kerstens, H.C.; Tuinzing, D.B.; van der Kwast, W.A. Temporomandibular joint symptoms in orthognathic surgery. J. Cranio-Maxillofac. Surg. 1989, 17, 215–218. [Google Scholar] [CrossRef]
- Solberg, W.K.; Bibb, C.A.; Nordstrom, B.B.; Hansson, T.L. Malocclusion associated with temporomandibular joint changes in young adults at autopsy. Am. J. Orthod. 1986, 89, 326–330. [Google Scholar] [CrossRef]
- O’Ryan, F.; Epker, B.N. Temporomandibular joint function and morphology: Observations on the spectra of normalcy. Oral Surg. Oral Med. Oral Pathol. 1984, 58, 272–279. [Google Scholar] [CrossRef]
- Schellhas, K.P. Unstable occlusion and temporomandibular joint disease. J. Clin. Orthod. 1989, 23, 332–337. [Google Scholar]
- Leonardi, R.M.; Aboulazm, K.; Giudice, A.L.; Ronsivalle, V.; D’Antò, V.; Lagravère, M.; Isola, G. Evaluation of mandibular changes after rapid maxillary expansion: A CBCT study in youngsters with unilateral posterior crossbite using a surface-to-surface matching technique. Clin. Oral Investig. 2021, 25, 1775–1785. [Google Scholar] [CrossRef]
- Upton, L.G.; Scott, R.F.; Hayward, J.R. Major maxillomandibular malrelations and temporomandibular joint pain-dysfunction. J. Prosthet. Dent. 1984, 51, 686–690. [Google Scholar] [CrossRef]
- Magnusson, T.; Ahlborg, G.; Svartz, K. Function of the masticatory system in 20 patients with mandibular hypo- or hyperplasia after correction by a sagittal split osteotomy. Int. J. Oral Maxillofac. Surg. 1990, 19, 289–293. [Google Scholar] [CrossRef]
- White, C.S.; Dolwick, M.F. Prevalence and variance of temporomandibular dysfunction in orthognathic surgery patients. Int. J. Adult Orthod. Orthognath. Surg. 1992, 7, 7–14. [Google Scholar]
- Le Bell, Y.; Lehtinen, R.; Peltomaki, T.; Peltola, J. Function of masticatory system after surgical-orthodontic correction of maxillomandibular discrepancies. Proc. Finn. Dent. Soc. 1993, 89, 101–107. [Google Scholar]
- Sadowsky, C.; BeGole, E.A. Long-term status of temporomandibular joint function and functional occlusion after orthodontic treatment. Am. J. Orthod. 1980, 78, 201–212. [Google Scholar] [CrossRef]
- Reynders, R.M. Orthodontics and temporomandibular disorders: A review of the literature (1966–1988). Am. J. Orthod. Dentofac. Orthop. 1990, 97, 463–471. [Google Scholar] [CrossRef]
- Seligman, D.A.; Pullinger, A.G. The role of functional occlusal relationships in temporomandibular disorders: A review. J. Craniomandib. Disord. 1991, 5, 265–279. [Google Scholar] [PubMed]
- Wadhwa, L.; Utreja, A.; Tewari, A. A study of clinical signs and symptoms of temporomandibular dysfunction in subjects with normal occlusion, untreated, and treated malocclusions. Am. J. Orthod. Dentofac. Orthop. 1993, 103, 54–61. [Google Scholar] [CrossRef]
- Leonardi, R.; Perrotta, R.E.; Almeida, L.E.; Loreto, C.; Musumeci, G. Lubricin in synovial fluid of mild and severe temporomandibular joint internal derangements. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e793–e799. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Barbato, E.; Cosentino, L.; Ferraro, C.M.; Leonardi, R. Alveolar bone changes after rapid maxillary expansion with tooth-born appliances: A systematic review. Eur. J. Orthod. 2018, 40, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Quinzi, V.; Ronsivalle, V.; Farronato, M.; Nicotra, C.; Indelicato, F.; Isola, G. Evaluation of Imaging Software Accuracy for 3-Dimensional Analysis of the Mandibular Condyle. A Comparative Study Using a Surface-to-Surface Matching Technique. Int. J. Environ. Res. Public Health 2020, 17, 4789. [Google Scholar] [CrossRef]
- Fichera, G.; Polizzi, A.; Scapellato, S.; Palazzo, G.; Indelicato, F. Craniomandibular Disorders in Pregnant Women: An Epidemiological Survey. J. Funct. Morphol. Kinesiol. 2020, 5, 36. [Google Scholar] [CrossRef]
- Leonardi, R.; Lo Giudice, A.; Rugeri, M.; Muraglie, S.; Cordasco, G.; Barbato, E. Three-dimensional evaluation on digital casts of maxillary palatal size and morphology in patients with functional posterior crossbite. Eur. J. Orthod. 2018, 40, 556–562. [Google Scholar] [CrossRef]
- Loreto, C.; Chiarenza, G.P.; Musumeci, G.; Castrogiovanni, P.; Imbesi, R.; Ruggeri, A.; Almeida, L.E.; Leonardi, R. ADAM10 localization in temporomandibular joint disk with internal derangement: An ex vivo immunohistochemical study. Acta Histochem. 2016, 118, 293–298. [Google Scholar] [CrossRef][Green Version]
- Leonardi, R.; Muraglie, S.; Lo Giudice, A.; Aboulazm, K.S.; Nucera, R. Evaluation of mandibular symmetry and morphology in adult patients with unilateral posterior crossbite: A CBCT study using a surface-to-surface matching technique. Eur. J. Orthod. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lo Giudice, A.; Rustico, L.; Caprioglio, A.; Migliorati, M.; Nucera, R. Evaluation of condylar cortical bone thickness in patient groups with different vertical facial dimensions using cone-beam computed tomography. Odontology 2020, 108, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Loreto, C.; Leonardi, R.; Musumeci, G.; Pannone, G.; Castorina, S. An ex vivo study on immunohistochemical localization of MMP-7 and MMP-9 in temporomandibular joint discs with internal derangement. Eur. J. Histochem. 2013, 57, e12. [Google Scholar] [CrossRef] [PubMed]
| Group A (N = 25) | Females 92% (N = 23) | Males 8% (N = 2) |
|---|---|---|
| Class I | 4 (16%) | 0 |
| Class II | 12 (48%) | 1 (4%) |
| Class III | 7 (28%) | 1 (4%) |
| Group B (N = 30) | Females 40%(N = 12) | Males 60% (N = 18) |
|---|---|---|
| Class I | 8 (26.7%) | 10 (33.3%) |
| Class II | 3 (10%) | 5 (16.7%) |
| Class III | 1 (3.3%) | 3 (10%) |
| Group A TMD | Group A Prevalence (%) N = 25 |
|---|---|
| DI | 64% (16) |
| DII | 28% (7) |
| DIII | 8% (2) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fichera, G.; Ronsivalle, V.; Santonocito, S.; Aboulazm, K.S.; Isola, G.; Leonardi, R.; Palazzo, G. Class II Skeletal Malocclusion and Prevalence of Temporomandibular Disorders. An Epidemiological Pilot Study on Growing Subjects. J. Funct. Morphol. Kinesiol. 2021, 6, 63. https://doi.org/10.3390/jfmk6030063
Fichera G, Ronsivalle V, Santonocito S, Aboulazm KS, Isola G, Leonardi R, Palazzo G. Class II Skeletal Malocclusion and Prevalence of Temporomandibular Disorders. An Epidemiological Pilot Study on Growing Subjects. Journal of Functional Morphology and Kinesiology. 2021; 6(3):63. https://doi.org/10.3390/jfmk6030063
Chicago/Turabian StyleFichera, Grazia, Vincenzo Ronsivalle, Simona Santonocito, Khaled S. Aboulazm, Gaetano Isola, Rosalia Leonardi, and Giuseppe Palazzo. 2021. "Class II Skeletal Malocclusion and Prevalence of Temporomandibular Disorders. An Epidemiological Pilot Study on Growing Subjects" Journal of Functional Morphology and Kinesiology 6, no. 3: 63. https://doi.org/10.3390/jfmk6030063
APA StyleFichera, G., Ronsivalle, V., Santonocito, S., Aboulazm, K. S., Isola, G., Leonardi, R., & Palazzo, G. (2021). Class II Skeletal Malocclusion and Prevalence of Temporomandibular Disorders. An Epidemiological Pilot Study on Growing Subjects. Journal of Functional Morphology and Kinesiology, 6(3), 63. https://doi.org/10.3390/jfmk6030063








