Role of Post-Operative Rehabilitation in TM Joint Arthritis: Functional Outcomes of Interposition Trapeziectomy vs. Prosthesis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Surgical Technique
2.3.1. Trapeziectomy with Ligament Reconstruction and Tendon Interposition (LRTI)
2.3.2. Trapeziometacarpal Joint Replacement
2.4. Post-Operative Management
2.5. Outcome Measures
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Clinical Outcomes by Group
3.3. Role of Rehabilitation
4. Discussion
4.1. Summary of Main Findings
4.2. Comparison with the Literature
4.3. Limitations of the Study
4.4. Clinical Implications
4.5. Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CMC | Carpo-metacarpal |
| OA | Osteoarthritis |
| DIP | Distal interphalangeal |
| TMC | Trapezio-metacarpal |
| AOL | Anterior oblique ligament |
| LRTI | Ligament reconstruction tendon interposition |
| APL | Abductor pollicis longus |
| FCR | Flexor carpi radialis |
| VAS | Visual analog scale |
| DASH | Disability of the arm, shoulder, and hand |
References
- Swigart, C.R. Arthritis of the base of the thumb. Curr. Rev. Musculoskelet. Med. 2008, 1, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Dahaghin, S.; Bierma-Zeinstra, S.M.; Ginai, A.Z.; Pols, H.A.; Hazes, J.M.; Koes, B.W. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann. Rheum. Dis. 2005, 64, 682–687. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.D.; Karl, J.W.; Strauch, R.J. Trapeziometacarpal joint stability: The evolving importance of the dorsal ligaments. Clin. Orthop. Relat. Res. 2014, 472, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Niu, J.; Zhang, Y.; LaValley, M.; Chaisson, C.E.; Aliabadi, P.; Felson, D.T. Symmetry and clustering of symptomatic hand osteoarthritis in elderly men and women: The Framingham Study. Rheumatology 2003, 42, 343–348. [Google Scholar] [CrossRef]
- Ladd, A.L. The Teleology of the Thumb: On Purpose and Design. J. Hand Surg. Am. 2018, 43, 248–259. [Google Scholar] [CrossRef]
- Abhishek, A.; Doherty, M. Diagnosis and clinical presentation of osteoarthritis. Rheum. Dis. Clin. N. Am. 2013, 39, 45–66. [Google Scholar] [CrossRef]
- Athlani, L.; De Almeida, Y.K.; Martins, A.; Seaourt, A.C.; Dap, F. Thumb basal joint arthritis in 2023. Orthop. Traumatol. Surg. Res. 2024, 110, 103772. [Google Scholar] [CrossRef]
- Ribak, S.; Ferreira, E.D.; Hirata, H.H.; Segura, E.L.; De Campos, R.B.; Tietzmann, A. Rhizarthrosis: Diagnostic assessment of rhizarthrosis clinical-radiological correlation. Int. Phys. Med. Rehabil. J. 2020, 5, 158–166. [Google Scholar] [CrossRef]
- Kennedy, C.D.; Manske, M.C.; Huang, J.I. Classifications in Brief: The Eaton-Littler Classification of Thumb Carpometacarpal Joint Arthrosis. Clin. Orthop. Relat. Res. 2016, 474, 2729–2733. [Google Scholar] [CrossRef]
- Dell, P.C.; Brushart, T.M.; Smith, R.J. Treatment of trapeziometacarpalarthritis: Results of resection arthroplasty. J. Hand Surg. 1978, 3, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Day, C.S.; Gelberman, R.; Patel, A.A.; Vogt, M.T.; Ditsios, K.; Boyer, M.I. Basal joint osteoarthritis of the thumb: A prospective trial of steroid injection and splinting. J. Hand Surg. Am. 2004, 29, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Hartigan, B.J.; Stern, P.J.; Kiefhaber, T.R. Thumb carpometacarpal osteoarthritis: Arthrodesis compared with ligament reconstruction and tendon interposition. J. Bone Jt. Surg. Am. 2001, 83, 1470–1478. [Google Scholar] [CrossRef]
- Slutsky, D.J. The role of arthroscopy in trapeziometacarpal arthritis. Clin. Orthop. Relat. Res. 2014, 472, 1173–1183. [Google Scholar] [CrossRef] [PubMed]
- Varley, G.W.; Calvey, J.; Hunter, J.B.; Barton, N.J.; Davis, T.R. Excision of the trapezium for osteoarthritis at the base of the thumb. J. Bone Jt. Surg. Br. 1994, 76, 964–968. [Google Scholar] [CrossRef]
- Pellegrini, V.D., Jr.; Burton, R.I. Surgical management of basal joint arthritis of the thumb. Part I. Long-term results of silicone implant arthroplasty. J. Hand Surg. Am. 1986, 11, 309–324. [Google Scholar] [CrossRef]
- Wolf, J.M.; Delaronde, S. Current trends in nonoperative and operative treatment of trapeziometacarpal osteoarthritis: A survey of US hand surgeons. J. Hand Surg. Am. 2012, 37, 77–82. [Google Scholar] [CrossRef]
- Merendi, G.; Fulchignoni, C.; Pietramala, S.; Rocchi, L. Trapeziectomy and suspension ligamentoplasty for surgical revision of trapeziometacarpal joint arthrodesis failure: Two cases. Hand Surg. Rehabil. 2022, 41, 400–403. [Google Scholar] [CrossRef] [PubMed]
- de la Caffiniere, J.Y.; Aucouturier, P. Trapezio-metacarpal arthroplasty by total prosthesis. Hand 1979, 11, 41–46. [Google Scholar] [CrossRef]
- Gerace, E.; Royaux, D.; Gaisne, E.; Ardouin, L.; Bellemère, P. Pyrocardan® implant arthroplasty for trapeziometacarpal osteoarthritis with a minimum follow-up of 5 years. Hand Surg. Rehabil. 2020, 39, 528–538. [Google Scholar] [CrossRef]
- Buffet, A.; Lucot-Royer, L.; Pichonnat, M.; Menu, G.; De Bie, A.; Obert, L.; Loisel, F. ISIS trapeziometacarpal arthroplasty: What are the outcomes in male patients? Hand Surg. Rehabil. 2022, 41, 463–469. [Google Scholar] [CrossRef]
- Holme, T.J.; Karbowiak, M.; Clements, J.; Sharma, R.; Craik, J.; Ellahee, N. Thumb CMCJ prosthetic total joint replacement: A systematic review. EFORT Open Rev. 2021, 6, 316–330. [Google Scholar] [CrossRef] [PubMed]
- Bonhof-Jansen, E.E.D.J.; Brink, S.M.; van Uchelen, J.H.; van der Sluis, C.K.; Broekstra, D.C. Immobilization, rehabilitation and complications classification after thumb trapeziometacarpal total joint arthroplasty. A scoping review. Hand Surg. Rehabil. 2024, 43, 101783. [Google Scholar] [CrossRef] [PubMed]
- Caggiari, G.; Polese, F.; Rosetti, C.; Ciurlia, E.; Brusoni, M.; Leone, A.; Pisanu, F.; Manunta, A.F.; Doria, C.; Manca, M. Suspension arthroplasty in the treatment of thumb carpometacarpal osteoarthritis. Orthop. Rev. 2021, 12, 8514. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guzzini, M.; Arioli, L.; Annibaldi, A.; Pecchia, S.; Latini, F.; Ferretti, A. Interposition Arthroplasty versus Dual Cup Mobility Prosthesis in Treatment of Trapeziometacarpal Joint Osteoarthritis: A Prospective Randomized Study. Hand 2024, 19, 1260–1268. [Google Scholar] [CrossRef]
- Piccirilli, E.; di Sette, P.; Rampoldi, M.; Primavera, M.; Salvati, C.; Tarantino, U. Comparative Analysis of Prosthetic (Touch) and Arthroplastic Surgeries for Trapeziometacarpal Arthrosis: Functional Outcomes and Patient Satisfaction with a 2-Year Follow-Up. J. Hand Surg. Glob. Online 2024, 6, 500–503. [Google Scholar] [CrossRef]
- Falkner, F.; Tümkaya, A.M.; Thomas, B.; Böcker, A.; Aman, M.; Bickert, B.; Harhaus, L.; Panzram, B. Resection arthroplasty versus dual mobility prosthesis in the treatment of trapeziometacarpal joint osteoarthritis: A 3 year non-randomized prospective study. J. Orthop. 2024, 57, 72–78. [Google Scholar] [CrossRef]
- Burton, R.I.; Pellegrini, V.D., Jr. Surgical management of basal joint arthritis of the thumb Part, I.I. Ligament reconstruction with tendon interposition arthroplasty. J. Hand Surg. Am. 1986, 11, 324–332. [Google Scholar] [CrossRef]
- Kriegs-Au, G.; Petje, G.; Fojtl, E.; Ganger, R.; Zachs, I. Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. A prospective randomized study. J. Bone Jt. Surg. Am. 2004, 86, 209–218. [Google Scholar] [CrossRef]
- Wolfe, T.; Chu, J.Y.; Woods, T.; Lubahn, J.D. A systematic review of postoperative hand therapy management of basal joint arthritis. Clin. Orthop. Relat. Res. 2014, 472, 1190–1197. [Google Scholar] [CrossRef]
| Type of surgery | Trapeziectomy | 31 |
| Joint replacement | 30 | |
| Gender | Male | 11 |
| Female | 50 | |
| Mean Age | 64.95 years old | Range 51–80 |
| Affected hand | Right | 32 |
| Left | 29 | |
| Eaton–Littler stage | I | 0 |
| II | 22 | |
| III | 35 | |
| IV | 4 | |
| Follow-up | 9.68 months | Range 6–35 |
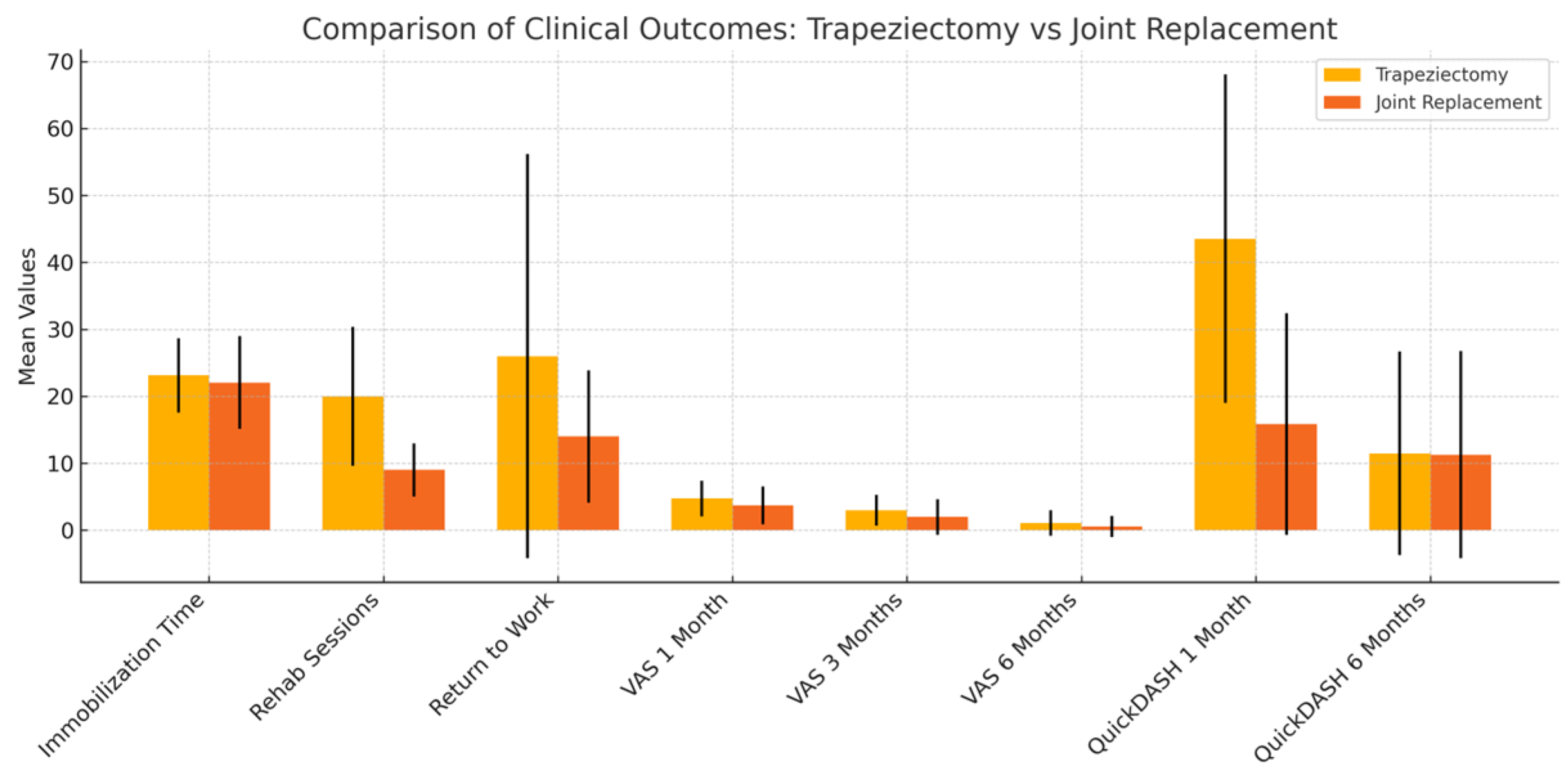
| Trapeziectomy | Joint Replacement | p-Value | |
|---|---|---|---|
| Rehabilitation | 17 | 11 | |
| Time of immobilization (m, SD) | 23.12 ± 5.53 | 22.06 ± 6.95 | 0.153 |
| N° rehabilitation sessions (m, SD) | 20 ± 10.38 | 9 ± 3.97 | 0.015 |
| Return to work (days) (m, SD) | 26 ± 30.18 | 14 ± 9.89 | 0.021 |
| VAS 1 month (m, SD) | 4.73 ± 2.65 | 3.71 ± 2.84 | 0.195 |
| VAS 3 months (m, SD) | 3.00 ± 2.29 | 1.97 ± 2.67 | 0.120 |
| VAS 6 months (m, SD) | 1.07 ± 1.92 | 0.58 ± 1.57 | 0.309 |
| quickDASH 1 month (m, SD) | 43.53 ± 24.54 | 15.87 ± 16.53 | <0.001 |
| quickDASH 6 months (m, SD) | 11.48 ± 15.19 | 11.29 ± 15.46 | 0.967 |
| Rehab | No Rehab | p-Value | |
|---|---|---|---|
| Return to work (days) (m, SD) | 41.21 ± 33.9 | 33.57 ± 27.4 | 0.14 |
| VAS 1 month (m, SD) | 4.76 ± 2.87 | 3.75 ± 2.65 | 0.08 |
| VAS 3 months (m, SD) | 3.16 ± 2.54 | 1.86 ± 2.36 | 0.02 |
| VAS 6 months (m, SD) | 1.56 ± 2.45 | 0.29 ± 1.14 | 0.03 |
| quickDASH 1 month (m, SD) | 33.85 ± 27.50 | 25.54 ± 22.48 | 0.10 |
| quickDASH 6 months (m, SD) | 13.10 ± 17.80 | 6.95 ± 14.08 | 0.06 |
| Rehab | No Rehab | p-Value | |
|---|---|---|---|
| Return to work (days) (m, SD) | 31.84 ± 10.68 | 26.43 ± 6.26 | 0.223 |
| VAS 1 month (m, SD) | 3.39 ± 2.95 | 4.63 ± 2.46 | 0.298 |
| VAS 3 months (m, SD) | 1.67 ± 2.61 | 2.75 ± 2.83 | 0.340 |
| VAS 6 months (m, SD) | 0.25 ± 0.78 | 1.67 ± 2.85 | 0.052 |
| quickDASH 1 month (m, SD) | 16.01 ± 17.35 | 15.31 ± 15.31 | 0.919 |
| quickDASH 6 months (m, SD) | 6.66 ± 10.54 | 25.00 ± 20.58 | 0.016 |
| Rehab | No Rehab | p-Value | |
|---|---|---|---|
| Return to work (days) (m, SD) | 51.63 ± 33.94 | 43.33 ± 15.34 | 0.356 |
| VAS 1 month (m, SD) | 5.4 ± 2.8 | 3.61 ± 2.25 | 0.041 |
| VAS 3 months (m, SD) | 3.4 ± 2.50 | 2.41 ± 2.19 | 0.147 |
| VAS 6 months (m, SD) | 1.42 ± 2.45 | 0.58 ± 1.44 | 0.139 |
| quickDASH 1 month (m, SD) | 46.62 ± 26.39 | 40.20 ± 22.00 | 0.247 |
| quickDASH 6 months (m, SD) | 13.55 ± 17.08 | 9.7 ± 14.08 | 0.278 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fulchignoni, C.; Pietramala, S.; Arioli, L.; Gerace, E.; De Mauro, D.; Frittella, G.; Di Dio, E.; Grauso, M.; Merendi, G.; Rocchi, L. Role of Post-Operative Rehabilitation in TM Joint Arthritis: Functional Outcomes of Interposition Trapeziectomy vs. Prosthesis. J. Funct. Morphol. Kinesiol. 2025, 10, 198. https://doi.org/10.3390/jfmk10020198
Fulchignoni C, Pietramala S, Arioli L, Gerace E, De Mauro D, Frittella G, Di Dio E, Grauso M, Merendi G, Rocchi L. Role of Post-Operative Rehabilitation in TM Joint Arthritis: Functional Outcomes of Interposition Trapeziectomy vs. Prosthesis. Journal of Functional Morphology and Kinesiology. 2025; 10(2):198. https://doi.org/10.3390/jfmk10020198
Chicago/Turabian StyleFulchignoni, Camillo, Silvia Pietramala, Leopoldo Arioli, Emanuele Gerace, Domenico De Mauro, Giulia Frittella, Elisa Di Dio, Mirko Grauso, Gianfranco Merendi, and Lorenzo Rocchi. 2025. "Role of Post-Operative Rehabilitation in TM Joint Arthritis: Functional Outcomes of Interposition Trapeziectomy vs. Prosthesis" Journal of Functional Morphology and Kinesiology 10, no. 2: 198. https://doi.org/10.3390/jfmk10020198
APA StyleFulchignoni, C., Pietramala, S., Arioli, L., Gerace, E., De Mauro, D., Frittella, G., Di Dio, E., Grauso, M., Merendi, G., & Rocchi, L. (2025). Role of Post-Operative Rehabilitation in TM Joint Arthritis: Functional Outcomes of Interposition Trapeziectomy vs. Prosthesis. Journal of Functional Morphology and Kinesiology, 10(2), 198. https://doi.org/10.3390/jfmk10020198








