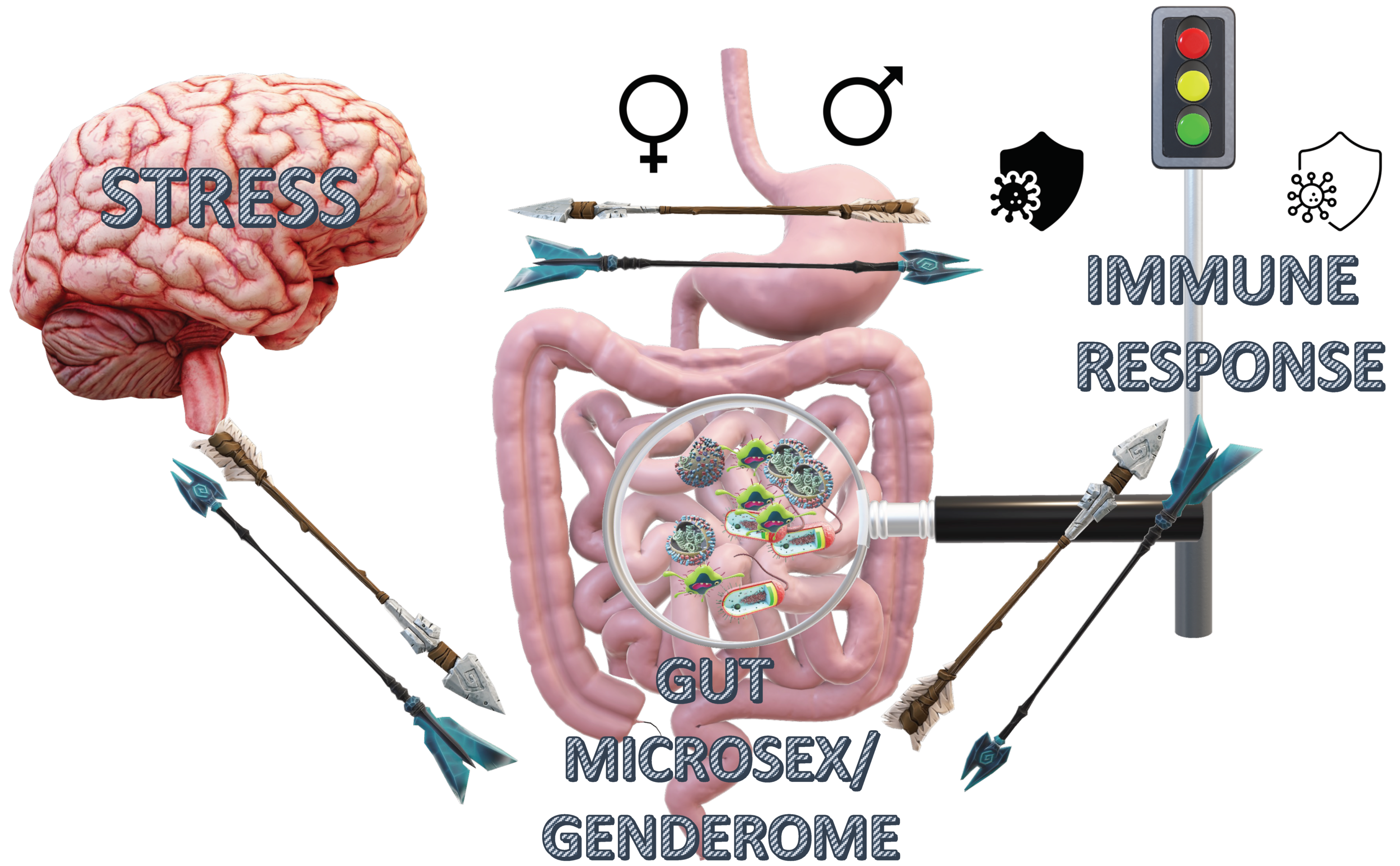
Gut Microsex/Genderome, Immunity and the Stress Response in the Sexes: An Updated Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Gut Microbiome in the Sexes: Gut Microsex/Genderome
3.2. Immunity and the Sexes
| Factor | Estrogens | Androgens | Progesterone |
|---|---|---|---|
| T cells |  Th1 differentiation, Th1 differentiation, TNF, IL-1β, IFN-γ, IL-4 TNF, IL-1β, IFN-γ, IL-4 Treg activation Treg activation T-cell apoptosis T-cell apoptosis |  Th1 response Th1 response T-cell proliferation T-cell proliferation IL-4 production IL-4 production Treg cells Treg cells | CD4+: IL-4 IL-4 Treg differentiation Treg differentiation IFN-γ IFN-γ proliferation proliferation T-dependent Ab responses T-dependent Ab responses Th17 differentiation Th17 differentiation IL-6 receptor IL-6 receptor |
CD8+: IFN-γ (MPA) IFN-γ (MPA) cytotoxicity (MPA) cytotoxicity (MPA) | |||
| B cells |  Activity Activity Antibody production Antibody production |  Antibody Antibodyproduction |  CD80 CD80 CD86 CD86 |
| Macrophages |  Phagocytosis Phagocytosis  TNF, IFN-γ, IL-6, IL-10 TNF, IFN-γ, IL-6, IL-10 TLR expression TLR expression Nitrite Nitrite |  Phagocytosis Phagocytosis TNF, iNOS, NO TNF, iNOS, NO TLR expression TLR expression IL-10, TGFβ IL-10, TGFβ |  iNOS, NO iNOS, NO TNF, IL1β TNF, IL1β FcγR expression FcγR expression microparticle release microparticle release |
| NK cells |  IFNγ IFNγ Granzyme B Granzyme B FASL FASL | ND * |  Apoptosis Apoptosis(Caspase dependent)  cytotoxicity cytotoxicity  IFN-γ IFN-γ |
| DCs |  Maturation Maturation Activation Activation TLR-7, TLR-9 TLR-7, TLR-9 CCL2, IL-6, IL-10, CXCL8 CCL2, IL-6, IL-10, CXCL8 |  IL-1β, IL-10, TNF IL-1β, IL-10, TNF |  CD40, CD80, CD86 CD40, CD80, CD86 IL-18, IL-10 IL-18, IL-10 TNF, IL-1β TNF, IL-1β |
| Neutrophils |  Numbers Numbers Degranulation Degranulation Elastase release Elastase release |  Numbers Numbers Kinases Kinases Leukotriene formation Leukotriene formation |  superoxide release superoxide release apoptosis apoptosis chemotaxis chemotaxis |
| Eosinophils |  Numbers Numbers Degranulation Degranulation Mobilization Mobilization |  Degranulation Degranulation |  Numbers Numbers Degranulation Degranulation |
| Autoimmunity/Autoinflammation |  |  | Dose -dependent action: Too high—  Too low—  |
| Firmicutes/Bacteroidetes ratio |  |  | ND * |
| Virome | Decrease in females | ND * | ND * |
| Mycobiome | ND * | ND * | ND * |
| Acute Stress Response (HPA axis—Cortisol, norepinephrine and epinephrine) | Upregulation of stress response, However, supportive of spatial memory during acute stress event | Suppression of HPA axis stress response in males | Progesterone results in inhibitory effects on HPA axis reactivity in females. |
| Chronic Stress Response (HPA axis—Cortisol, norepinephrine and epinephrine) | Upregulation of stress response, However, supportive of spatial memory during acute stress event | Suppression of HPA axis stress response in males | Downregulation of the stress response/Upregulation of the GABAminergic system |
3.3. Stress Response in the Sexes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karlstadt, R.; Hogan, D.; Foxx-Orenstein, A. Normal Physiology of the Gastrointestinal Tract and Gender Differences. In Principles of Gender-Specific Medicine; Elsevier: Amsterdam, The Netherlands, 2007; Volume 1, pp. 377–396. [Google Scholar]
- Marchesi, J.R.; Ravel, J. The vocabulary of microbiome research: A proposal. Microbiome 2015, 3, 31. [Google Scholar] [CrossRef] [PubMed]
- Stefanaki, C.; Peppa, M.; Mastorakos, G.; Chrousos, G.P. Examining the gut bacteriome, virome, and mycobiome in glucose metabolism disorders: Are we on the right track? Metabolism Clin. Exp. 2017, 73, 52–66. [Google Scholar] [CrossRef] [PubMed]
- Ahearn-Ford, S.; Berrington, J.E.; Stewart, C.J. Development of the gut microbiome in early life. Exp. Physiol. 2022, 107, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Vemuri, R.; Sylvia, K.E.; Klein, S.L.; Forster, S.C.; Plebanski, M.; Eri, R.; Flanagan, K.L. The microgenderome revealed: Sex differences in bidirectional interactions between the microbiota, hormones, immunity and disease susceptibility. Semin. Immunopathol. 2019, 41, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Mulak, A.; Larauche, M.; Tache, Y. Sexual Dimorphism in the Gut Microbiome: Microgenderome or Microsexome? J. Neurogastroenterol. Motil. 2022, 28, 332–333. [Google Scholar] [CrossRef] [PubMed]
- Kim, N. Sexual Dimorphism in the Gut Microbiome: Microgenderome or Microsexome? Author’s Reply. J. Neurogastroenterol. Motil. 2022, 28, 334. [Google Scholar] [CrossRef] [PubMed]
- Amador-Patarroyo, M.J.; Rodriguez-Rodriguez, A.; Montoya-Ortiz, G. How does age at onset influence the outcome of autoimmune diseases? Autoimmune Dis. 2012, 2012, 251730. [Google Scholar] [CrossRef]
- Brenhouse, H.C.; Schwarz, J.M. Immunoadolescence: Neuroimmune development and adolescent behavior. Neurosci. Biobehav. Rev. 2016, 70, 288–299. [Google Scholar] [CrossRef]
- De Gruijter, N.M.; Naja, M.; Peckham, H.; Radziszewska, A.; Kinsella, M.; Glenister, J.; Rosser, E.C.; Butler, G.E.; Jury, E.C.; Ciurtin, C. A systematic review exploring the bidirectional relationship between puberty and autoimmune rheumatic diseases. Pediatr. Rheumatol. 2021, 19, 47. [Google Scholar] [CrossRef]
- Huang, Q.; Kahn, C.R.; Altindis, E. Viral Hormones: Expanding Dimensions in Endocrinology. Endocrinology 2019, 160, 2165–2179. [Google Scholar] [CrossRef]
- Baker, J.M.; Al-Nakkash, L.; Herbst-Kralovetz, M.M. Estrogen–gut microbiome axis: Physiological and clinical implications. Maturitas 2017, 103, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Ervin, S.M.; Li, H.; Lim, L.; Roberts, L.R.; Liang, X.; Mani, S.; Redinbo, M.R. Gut microbial beta-glucuronidases reactivate estrogens as components of the estrobolome that reactivate estrogens. J. Biol. Chem. 2019, 294, 18586–18599. [Google Scholar] [CrossRef] [PubMed]
- Collden, H.; Landin, A.; Wallenius, V.; Elebring, E.; Fandriks, L.; Nilsson, M.E.; Ryberg, H.; Poutanen, M.; Sjogren, K.; Vandenput, L.; et al. The gut microbiota is a major regulator of androgen metabolism in intestinal contents. Am. J. Physiol. Endocrinol. Metab. 2019, 317, E1182–E1192. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.; Kim, N. Roles of Sex Hormones and Gender in the Gut Microbiota. J. Neurogastroenterol. Motil. 2021, 27, 314–325. [Google Scholar] [CrossRef]
- Shin, J.H.; Park, Y.H.; Sim, M.; Kim, S.A.; Joung, H.; Shin, D.M. Serum level of sex steroid hormone is associated with diversity and profiles of human gut microbiome. Res. Microbiol. 2019, 170, 192–201. [Google Scholar] [CrossRef]
- He, S.; Li, H.; Yu, Z.; Zhang, F.; Liang, S.; Liu, H.; Chen, H.; Lu, M. The Gut Microbiome and Sex Hormone-Related Diseases. Front. Microbiol. 2021, 12, 711137. [Google Scholar] [CrossRef]
- Tyborowska, A.; Volman, I.; Niermann, H.C.M.; Pouwels, J.L.; Smeekens, S.; Cillessen, A.H.N.; Toni, I.; Roelofs, K. Early-life and pubertal stress differentially modulate grey matter development in human adolescents. Sci. Rep. 2018, 8, 9201. [Google Scholar] [CrossRef]
- Sakai, J. Core Concept: How synaptic pruning shapes neural wiring during development and, possibly, in disease. Proc. Natl. Acad. Sci. USA 2020, 117, 16096–16099. [Google Scholar] [CrossRef]
- Hollister, E.B.; Riehle, K.; Luna, R.A.; Weidler, E.M.; Rubio-Gonzales, M.; Mistretta, T.A.; Raza, S.; Doddapaneni, H.V.; Metcalf, G.A.; Muzny, D.M.; et al. Structure and function of the healthy pre-adolescent pediatric gut microbiome. Microbiome 2015, 3, 36. [Google Scholar] [CrossRef]
- Shames, R.S. Gender differences in the development and function of the immune system. J. Adolesc. Health 2002, 30, 59–70. [Google Scholar] [CrossRef]
- Li, X.; Cheng, W.; Shang, H.; Wei, H.; Deng, C. The Interplay between Androgen and Gut Microbiota: Is There a Microbiota-Gut-Testis Axis. Reprod. Sci. 2022, 29, 1674–1684. [Google Scholar] [CrossRef]
- Markle, J.G.; Frank, D.N.; Mortin-Toth, S.; Robertson, C.E.; Feazel, L.M.; Rolle-Kampczyk, U.; von Bergen, M.; McCoy, K.D.; Macpherson, A.J.; Danska, J.S. Sex differences in the gut microbiome drive hormone-dependent regulation of autoimmunity. Science 2013, 339, 1084–1088. [Google Scholar] [CrossRef]
- Wallis, A.; Butt, H.; Ball, M.; Lewis, D.P.; Bruck, D. Support for the Microgenderome: Associations in a Human Clinical Population. Sci. Rep. 2016, 6, 19171. [Google Scholar] [CrossRef]
- Jacobsen, H.; Klein, S.L. Sex Differences in Immunity to Viral Infections. Front. Immunol. 2021, 12, 720952. [Google Scholar] [CrossRef]
- Park, H.; Bourla, A.B.; Kastner, D.L.; Colbert, R.A.; Siegel, R.M. Lighting the fires within: The cell biology of autoinflammatory diseases. Nat. Rev. Immunol. 2012, 12, 570–580. [Google Scholar] [CrossRef]
- McCreary, J.K.; Erickson, Z.T.; Paxman, E.; Kiss, D.; Montina, T.; Olson, D.M.; Metz, G.A.S. The rat cumulative allostatic load measure (rCALM): A new translational assessment of the burden of stress. Environ. Epigenetics 2019, 5, dvz005. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA–A scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Valeri, F.; Endres, K. How biological sex of the host shapes its gut microbiota. Front. Neuroendocrinol. 2021, 61, 100912. [Google Scholar] [CrossRef] [PubMed]
- Nagpal, R.; Kurakawa, T.; Tsuji, H.; Takahashi, T.; Kawashima, K.; Nagata, S.; Nomoto, K.; Yamashiro, Y. Evolution of gut Bifidobacterium population in healthy Japanese infants over the first three years of life: A quantitative assessment. Sci. Rep. 2017, 7, 10097. [Google Scholar] [CrossRef] [PubMed]
- Vander Wyst, K.B.; Ortega-Santos, C.P.; Toffoli, S.N.; Lahti, C.E.; Whisner, C.M. Diet, adiposity, and the gut microbiota from infancy to adolescence: A systematic review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2021, 22, e13175. [Google Scholar] [CrossRef]
- Wilmanski, T.; Diener, C.; Rappaport, N.; Patwardhan, S.; Wiedrick, J.; Lapidus, J.; Earls, J.C.; Zimmer, A.; Glusman, G.; Robinson, M.; et al. Gut microbiome pattern reflects healthy ageing and predicts survival in humans. Nat. Metab. 2021, 3, 274–286. [Google Scholar] [CrossRef]
- Ma, Z.S.; Li, W. How and Why Men and Women Differ in Their Microbiomes: Medical Ecology and Network Analyses of the Microgenderome. Adv. Sci. 2019, 6, 1902054. [Google Scholar] [CrossRef] [PubMed]
- Yurkovetskiy, L.; Burrows, M.; Khan, A.A.; Graham, L.; Volchkov, P.; Becker, L.; Antonopoulos, D.; Umesaki, Y.; Chervonsky, A.V. Gender bias in autoimmunity is influenced by microbiota. Immunity 2013, 39, 400–412. [Google Scholar] [CrossRef]
- Haro, C.; Rangel-Zuniga, O.A.; Alcala-Diaz, J.F.; Gomez-Delgado, F.; Perez-Martinez, P.; Delgado-Lista, J.; Quintana-Navarro, G.M.; Landa, B.B.; Navas-Cortes, J.A.; Tena-Sempere, M.; et al. Intestinal Microbiota Is Influenced by Gender and Body Mass Index. PLoS ONE 2016, 11, e0154090. [Google Scholar] [CrossRef]
- Koliada, A.; Moseiko, V.; Romanenko, M.; Lushchak, O.; Kryzhanovska, N.; Guryanov, V.; Vaiserman, A. Sex differences in the phylum-level human gut microbiota composition. BMC Microbiol. 2021, 21, 131. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Unno, T.; Kim, B.Y.; Park, M.S. Sex Differences in Gut Microbiota. World J. Men’s Health 2020, 38, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Ding, T.; Schloss, P.D. Dynamics and associations of microbial community types across the human body. Nature 2014, 509, 357–360. [Google Scholar] [CrossRef] [PubMed]
- Mitev, K.; Taleski, V. Association between the Gut Microbiota and Obesity. Open Access Maced. J. Med. Sci. 2019, 7, 2050–2056. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, R.; Cheung, A.S.; Pang, K.; Saffery, R.; Novakovic, B. Sexual Dimorphism in Innate Immunity: The Role of Sex Hormones and Epigenetics. Front. Immunol. 2020, 11, 604000. [Google Scholar] [CrossRef] [PubMed]
- Elgendy, I.Y.; Pepine, C.J. Why are women better protected from COVID-19: Clues for men? Sex and COVID-19. Int. J. Cardiol. 2020, 315, 105–106. [Google Scholar] [CrossRef]
- Sever, R.; Glass, C.K. Signaling by nuclear receptors. Cold Spring Harb. Perspect. Biol. 2013, 5, a016709. [Google Scholar] [CrossRef]
- Ma, W.T.; Gao, F.; Gu, K.; Chen, D.K. The Role of Monocytes and Macrophages in Autoimmune Diseases: A Comprehensive Review. Front. Immunol. 2019, 10, 1140. [Google Scholar] [CrossRef]
- Gay, L.; Melenotte, C.; Lakbar, I.; Mezouar, S.; Devaux, C.; Raoult, D.; Bendiane, M.K.; Leone, M.; Mege, J.L. Sexual Dimorphism and Gender in Infectious Diseases. Front. Immunol. 2021, 12, 698121. [Google Scholar] [CrossRef] [PubMed]
- Krainer, J.; Siebenhandl, S.; Weinhausel, A. Systemic autoinflammatory diseases. J. Autoimmun. 2020, 109, 102421. [Google Scholar] [CrossRef] [PubMed]
- Hughes, G.C. Progesterone and autoimmune disease. Autoimmun. Rev. 2012, 11, A502–A514. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.O.; Kamilaris, T.C.; Chrousos, G.P.; Gold, P.W. Mechanisms of stress: A dynamic overview of hormonal and behavioral homeostasis. Neurosci. Biobehav. Rev. 1992, 16, 115–130. [Google Scholar] [CrossRef]
- Wirth, M.M. Beyond the HPA Axis: Progesterone-Derived Neuroactive Steroids in Human Stress and Emotion. Front. Endocrinol. 2011, 2, 19. [Google Scholar] [CrossRef]
- Hokenson, R.E.; Short, A.K.; Chen, Y.; Pham, A.L.; Adams, E.T.; Bolton, J.L.; Swarup, V.; Gall, C.M.; Baram, T.Z. Unexpected Role of Physiological Estrogen in Acute Stress-Induced Memory Deficits. J. Neurosci. Off. J. Soc. Neurosci. 2021, 41, 648–662. [Google Scholar] [CrossRef]
- Sheng, J.A.; Tan, S.M.L.; Hale, T.M.; Handa, R.J. Androgens and Their Role in Regulating Sex Differences in the Hypothalamic/Pituitary/Adrenal Axis Stress Response and Stress-Related Behaviors. Androg. Clin. Res. Ther. 2021, 2, 261–274. [Google Scholar] [CrossRef] [PubMed]
- Gordon, J.L.; Peltier, A.; Grummisch, J.A.; Sykes Tottenham, L. Estradiol Fluctuation, Sensitivity to Stress, and Depressive Symptoms in the Menopause Transition: A Pilot Study. Front. Psychol. 2019, 10, 1319. [Google Scholar] [CrossRef] [PubMed]
- Stephens, M.A.; Mahon, P.B.; McCaul, M.E.; Wand, G.S. Hypothalamic-pituitary-adrenal axis response to acute psychosocial stress: Effects of biological sex and circulating sex hormones. Psychoneuroendocrinology 2016, 66, 47–55. [Google Scholar] [CrossRef]
- Heck, A.L.; Handa, R.J. Sex differences in the hypothalamic-pituitary-adrenal axis’ response to stress: An important role for gonadal hormones. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2019, 44, 45–58. [Google Scholar] [CrossRef] [PubMed]
- Nouri, A.; Hashemzadeh, F.; Soltani, A.; Saghaei, E.; Amini-Khoei, H. Progesterone exerts antidepressant-like effect in a mouse model of maternal separation stress through mitigation of neuroinflammatory response and oxidative stress. Pharm. Biol. 2020, 58, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Patchev, V.K.; Hayashi, S.; Orikasa, C.; Almeida, O.F. Implications of estrogen-dependent brain organization for gender differences in hypothalamo-pituitary-adrenal regulation. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 1995, 9, 419–423. [Google Scholar] [CrossRef]
- Rosinger, Z.J.; Jacobskind, J.S.; Bulanchuk, N.; Malone, M.; Fico, D.; Justice, N.J.; Zuloaga, D.G. Characterization and gonadal hormone regulation of a sexually dimorphic corticotropin-releasing factor receptor 1 cell group. J. Comp. Neurol. 2019, 527, 1056–1069. [Google Scholar] [CrossRef] [PubMed]
- Sheng, J.A.; Bales, N.J.; Myers, S.A.; Bautista, A.I.; Roueinfar, M.; Hale, T.M.; Handa, R.J. The Hypothalamic-Pituitary-Adrenal Axis: Development, Programming Actions of Hormones, and Maternal-Fetal Interactions. Front. Behav. Neurosci. 2020, 14, 601939. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, K.; Yoshino, K.; Sanada, K.; Beppu, H.; Akiyama, Y.; Nishimura, H.; Tanaka, K.; Sonoda, S.; Ueno, H.; Yoshimura, M.; et al. Effect of oestrogen-dependent vasopressin on HPA axis in the median eminence of female rats. Sci. Rep. 2019, 9, 5153. [Google Scholar] [CrossRef] [PubMed]
- Weiser, M.J.; Handa, R.J. Estrogen impairs glucocorticoid dependent negative feedback on the hypothalamic-pituitary-adrenal axis via estrogen receptor alpha within the hypothalamus. Neuroscience 2009, 159, 883–895. [Google Scholar] [CrossRef] [PubMed]
- Vamvakopoulos, N.C.; Chrousos, G.P. Hormonal regulation of human corticotropin-releasing hormone gene expression: Implications for the stress response and immune/inflammatory reaction. Endocr. Rev. 1994, 15, 409–420. [Google Scholar] [CrossRef]
- Vamvakopoulos, N.C.; Chrousos, G.P. Evidence of direct estrogenic regulation of human corticotropin-releasing hormone gene expression. Potential implications for the sexual dimophism of the stress response and immune/inflammatory reaction. J. Clin. Investig. 1993, 92, 1896–1902. [Google Scholar] [CrossRef]
- Ruiz, D.; Padmanabhan, V.; Sargis, R.M. Stress, Sex, and Sugar: Glucocorticoids and Sex-Steroid Crosstalk in the Sex-Specific Misprogramming of Metabolism. J. Endocr. Soc. 2020, 4, bvaa087. [Google Scholar] [CrossRef] [PubMed]
- Zuloaga, D.G.; Heck, A.L.; De Guzman, R.M.; Handa, R.J. Roles for androgens in mediating the sex differences of neuroendocrine and behavioral stress responses. Biol. Sex Differ. 2020, 11, 44. [Google Scholar] [CrossRef]
- Snell, D.M.; Turner, J.M.A. Sex Chromosome Effects on Male-Female Differences in Mammals. Curr. Biol. 2018, 28, R1313–R1324. [Google Scholar] [CrossRef]
- Moisan, M.P. Sexual Dimorphism in Glucocorticoid Stress Response. Int. J. Mol. Sci. 2021, 22, 3139. [Google Scholar] [CrossRef] [PubMed]
- Stefanaki, C.; Michos, A.; Roma-Giannikou, E.; Mantzou, A.; Paltoglou, G.; Landis, D.; Bacopoulou, F. Adolescents with Prediabetes Lack Key Species by Quantitative, Core Gut Microbiome Analysis—A Case-Control Study. In Proceedings of the ENDO 2016, Boston, MA, USA, 1–4 April 2016. [Google Scholar]
- Dogra, S.K.; Kwong Chung, C.; Wang, D.; Sakwinska, O.; Colombo Mottaz, S.; Sprenger, N. Nurturing the Early Life Gut Microbiome and Immune Maturation for Long Term Health. Microorganisms 2021, 9, 2110. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, S.; Selma-Royo, M.; Arboleya, S.; Martinez-Costa, C.; Solis, G.; Suarez, M.; Fernandez, N.; de Los Reyes-Gavilan, C.G.; Diaz-Coto, S.; Martinez-Camblor, P.; et al. Levels of Predominant Intestinal Microorganisms in 1 Month-Old Full-Term Babies and Weight Gain during the First Year of Life. Nutrients 2021, 13, 2412. [Google Scholar] [CrossRef] [PubMed]
- Flak, M.B.; Neves, J.F.; Blumberg, R.S. Welcome to the microgenderome. Science 2013, 339, 1044–1045. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Yun, C.; Pang, Y.; Qiao, J. The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut Microbes 2021, 13, 1894070. [Google Scholar] [CrossRef]
- Bagchi, B.; Corbel, Q.; Khan, I.; Payne, E.; Banerji, D.; Liljestrand-Ronn, J.; Martinossi-Allibert, I.; Baur, J.; Sayadi, A.; Immonen, E.; et al. Sexual conflict drives micro- and macroevolution of sexual dimorphism in immunity. BMC Biol. 2021, 19, 114. [Google Scholar] [CrossRef]
- Ruggieri, A.; Anticoli, S.; D’Ambrosio, A.; Giordani, L.; Viora, M. The influence of sex and gender on immunity, infection and vaccination. Ann. dell’Istituto Super. Sanita 2016, 52, 198–204. [Google Scholar] [CrossRef]
- Tsigos, C.; Kyrou, I.; Kassi, E.; Chrousos, G.P. Stress: Endocrine Physiology and Pathophysiology. In Endotext; Feingold, K.R., Anawalt, B., Boyce, A., Chrousos, G., de Herder, W.W., Dhatariya, K., Dungan, K., Hershman, J.M., Hofland, J., Kalra, S., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Chrousos, G.P. Stress and disorders of the stress system. Nat. Rev. Endocrinol. 2009, 5, 374–381. [Google Scholar] [CrossRef]
- Stefanaki, C.; Pervanidou, P.; Boschiero, D.; Chrousos, G.P. Chronic stress and body composition disorders: Implications for health and disease. Hormones 2018, 17, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Stefanaki, C.; Michos, A.; Latsios, G.; Tousoulis, D.; Peppa, M.; Zosi, P.; Boschiero, D.; Bacopoulou, F. Sexual Dimorphism of Heart Rate Variability in Adolescence: A Case-Control Study on Depression, Anxiety, Stress Levels, Body Composition, and Heart Rate Variability in Adolescents with Impaired Fasting Glucose. Int. J. Environ. Res. Public Health 2020, 17, 2688. [Google Scholar] [CrossRef]
- Stefanaki, C.; Paltoglou, G.; Mastorakos, G.; Chrousos, G.P. Chronic Stress and Steatosis of Muscles, Bones, Liver, and Pancreas—A Review. Horm. Res. Paediatr. 2022. [Google Scholar] [CrossRef] [PubMed]
- Oyola, M.G.; Handa, R.J. Hypothalamic-pituitary-adrenal and hypothalamic-pituitary-gonadal axes: Sex differences in regulation of stress responsivity. Stress 2017, 20, 476–494. [Google Scholar] [CrossRef]
- Elderman, M.; Hugenholtz, F.; Belzer, C.; Boekschoten, M.; van Beek, A.; de Haan, B.; Savelkoul, H.; de Vos, P.; Faas, M. Sex and strain dependent differences in mucosal immunology and microbiota composition in mice. Biol. Sex Differ. 2018, 9, 26. [Google Scholar] [CrossRef]
- Maffei, S.; Forini, F.; Canale, P.; Nicolini, G.; Guiducci, L. Gut Microbiota and Sex Hormones: Crosstalking Players in Cardiometabolic and Cardiovascular Disease. Int. J. Mol. Sci. 2022, 23, 7154. [Google Scholar] [CrossRef] [PubMed]
- Stefanaki, C.; Valsamakis, G.; Mastorakos, G. Gut Microbiome, Diabetes, and Obesity: Complex Interplay of Physiology. In Gut Microbiome-Related Diseases and Therapies; Gazouli, M., Theodoropoulos, G., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 169–181. [Google Scholar]
- Stefanaki, C.; Mastorakos, G.; Chrousos, G.P. Gut Microbiome and Mental Stress-Related Disorders: The Interplay of Classic and Microbial Endocrinology. In Gut Microbiome-Related Diseases and Therapies; Gazouli, M., Theodoropoulos, G., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 229–242. [Google Scholar]
- Stefanaki, C. The Gut Microbiome Beyond the Bacteriome–The Neglected Role of Virome and Mycobiome in Health and Disease. Microbiome Metab. Diagn. Ther. Other Strateg. Appl. 2019, 27–32. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefanaki, C.; Bacopoulou, F.; Chrousos, G.P. Gut Microsex/Genderome, Immunity and the Stress Response in the Sexes: An Updated Review. Sexes 2022, 3, 533-545. https://doi.org/10.3390/sexes3040039
Stefanaki C, Bacopoulou F, Chrousos GP. Gut Microsex/Genderome, Immunity and the Stress Response in the Sexes: An Updated Review. Sexes. 2022; 3(4):533-545. https://doi.org/10.3390/sexes3040039
Chicago/Turabian StyleStefanaki, Charikleia, Flora Bacopoulou, and George P. Chrousos. 2022. "Gut Microsex/Genderome, Immunity and the Stress Response in the Sexes: An Updated Review" Sexes 3, no. 4: 533-545. https://doi.org/10.3390/sexes3040039
APA StyleStefanaki, C., Bacopoulou, F., & Chrousos, G. P. (2022). Gut Microsex/Genderome, Immunity and the Stress Response in the Sexes: An Updated Review. Sexes, 3(4), 533-545. https://doi.org/10.3390/sexes3040039








