Effects of Implementing the Timed and Targeted Counselling Model on Pregnancy Outcomes and Newborn Survival in Rural Uganda: Protocol for a Quasi-Experimental Study
Abstract
1. Background
2. Methods
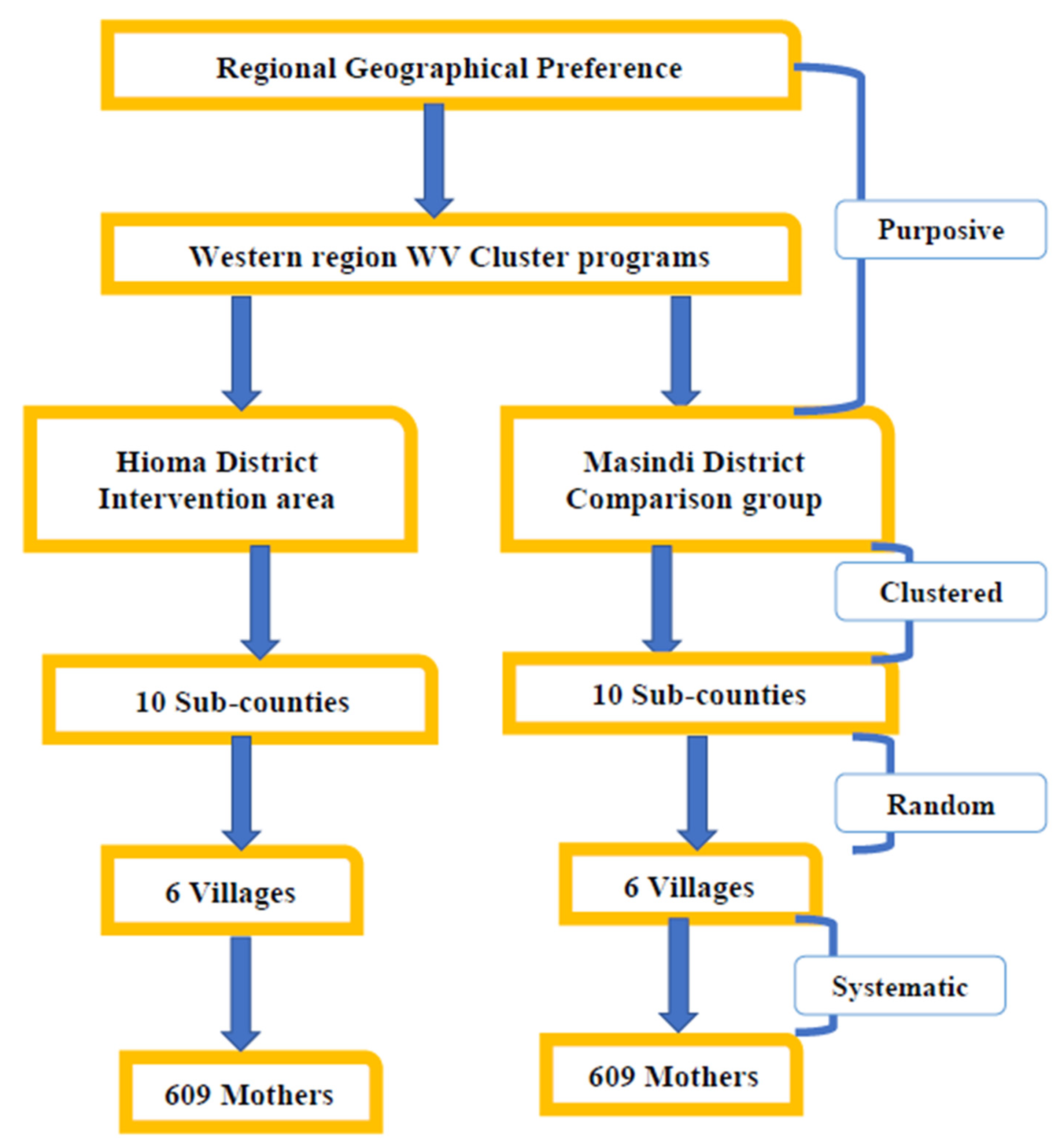
2.1. Study Design
2.2. Study Site
2.3. Ethics Approval and Consent to Participate
2.4. Study Population
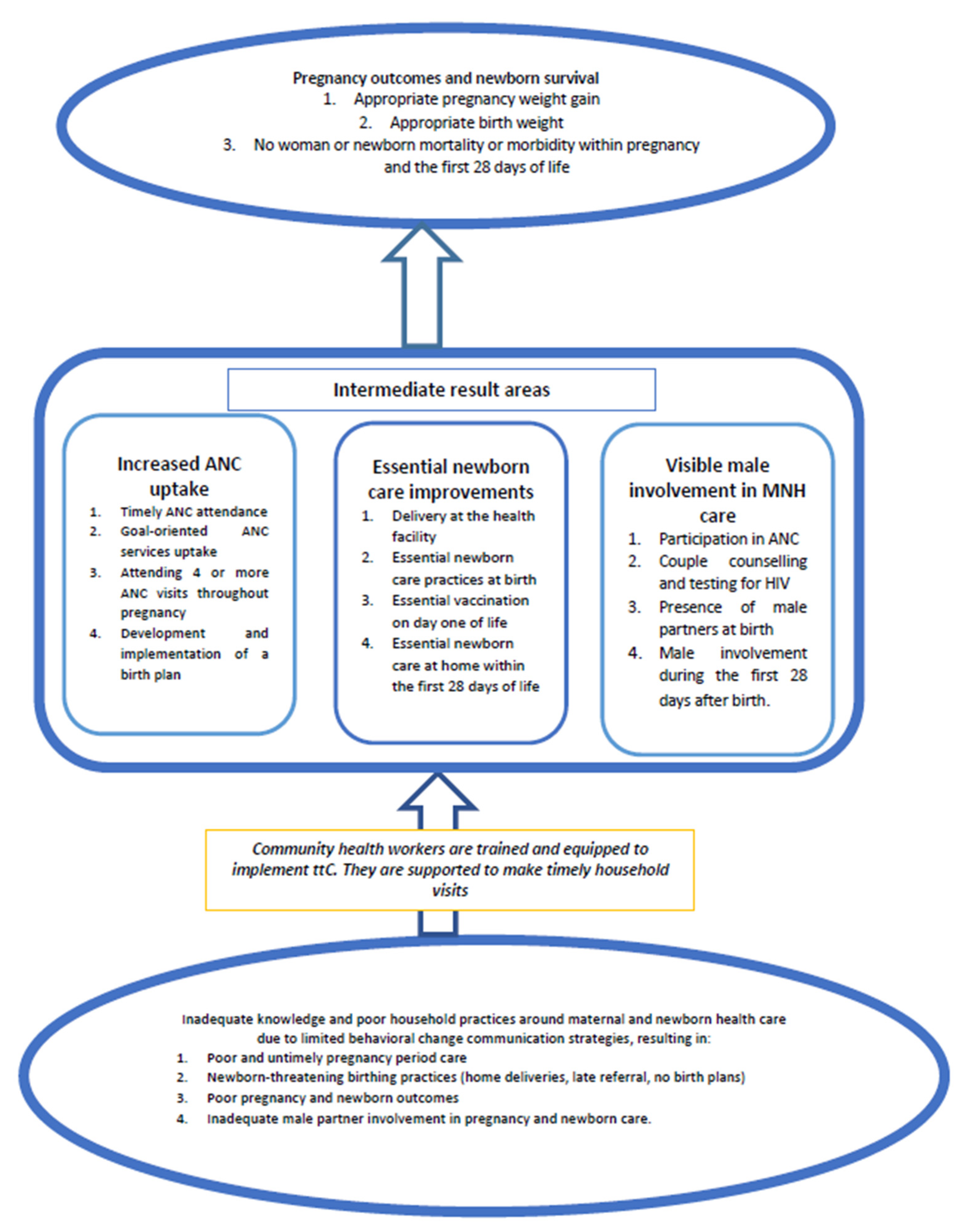
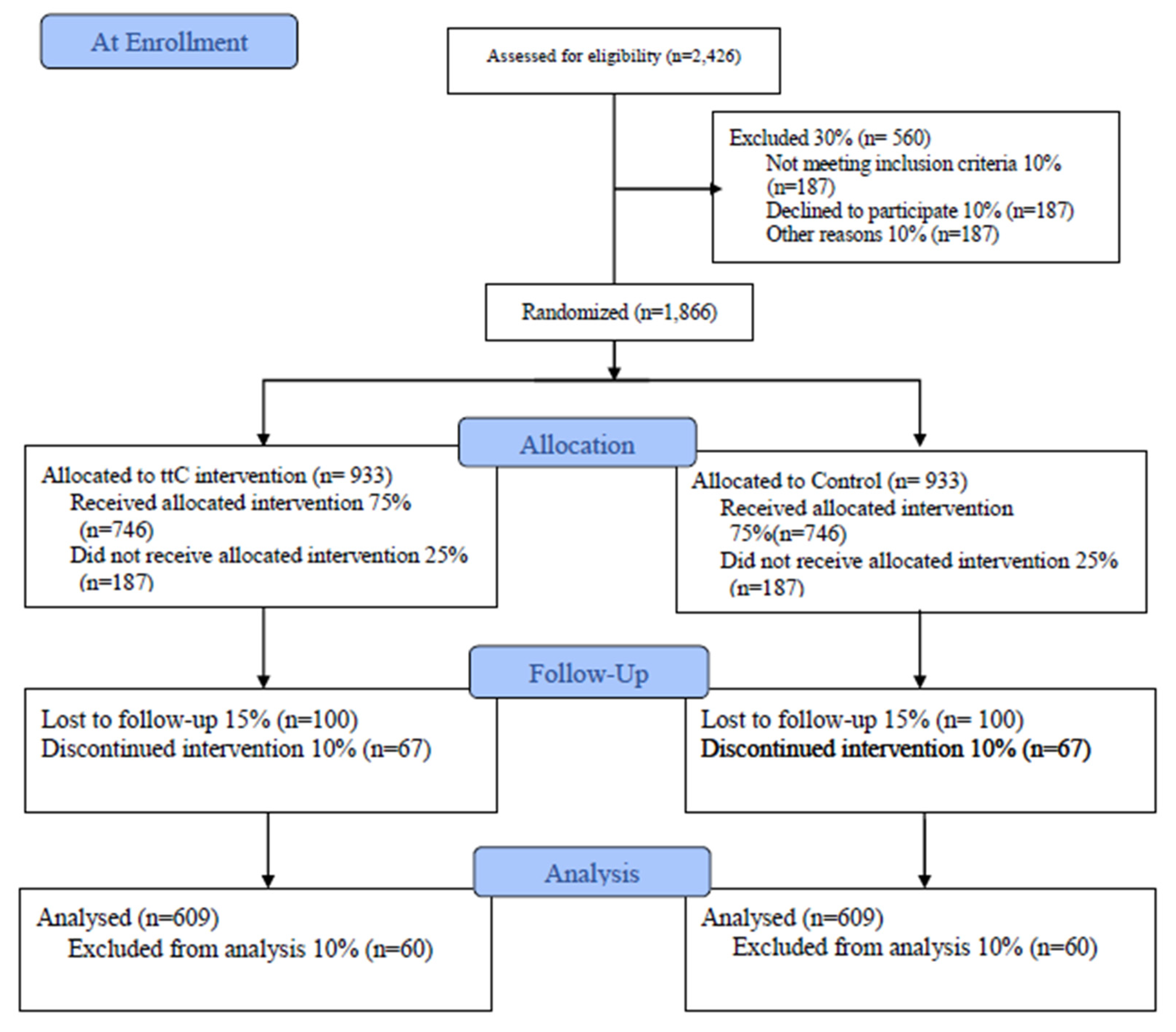
2.5. Conceptual Framework
2.6. Intervention
2.7. Delivery of Services in the Control District
2.8. Sample Size
2.9. Study Timelines
2.10. Sampling Procedure
2.11. Study Instruments
- The Ugandan VHT household register (VHTR): This will be the entry basis into the community for both study sites. All mothers to be included in the study must have been registered by the VHT at the household level in this household register.
- The ttC register (ttCR): This will provide the data required for the intervention implementation analysis (process evaluation). It will also be the entry point for mothers to be included in the study and the VHTs are responsible for documentation using this register. The tool captures day-to-day visit activities between the household and the VHT.
- Study Questionnaire (SQ): This has been developed specifically to collect data that will be used for outcome results at the end of the intervention. An expert staff member in ttC has provided guidance that led to the revision of the tool in line with the sub-objectives. Furthermore, two researchers were asked to critically review the tool in line with the standard objectives. Their comments have been incorporated into the tool. More pre-testing of the tool will be done at the field level during the training of the enumerators.
2.12. Study Variables
3. Data Management and Analysis
3.1. Dissemination of Results
3.2. Study Strength and Weaknesses
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Maternal Mortality. Available online: https://www.who.int/en/news-room/fact-sheets/detail/maternal-mortality (accessed on 19 September 2019).
- Catharine, B. WHO Report: Triple Pace of Progress to Achieve SDGs’ Maternal Mortality Target. Available online: http://sdg.iisd.org/news/who-report-triple-pace-of-progress-to-achieve-sdgs-maternal-mortality-target/ (accessed on 19 November 2015).
- Girum, T.; Wasie, A. Correlates of maternal mortality in developing countries: An ecological study in 82 countries. Matern. Health Neonatol. Perinatol. 2017, 3, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Uganda, 2010, Village Health Team A Handbook to Improve Health in Communities. Available online: https://www.thecompassforsbc.org/project-examples/village-health-team-handbook (accessed on 1 January 2011).
- United Nations, Department of Economic and Social Affairs, 2015, Sustainable Development Goal 3. Ensure Healthy Lives and Promote Well-Being for All at All Ages. Available online: https://sdgs.un.org/goals/goal3 (accessed on 2 June 2016).
- Healthy Newborn Network. The Reproductive Maternal Newborn and Child Health Sharpened Plan for Uganda. Available online: https://www.healthynewbornnetwork.org/resource/reproductive-maternal-newborn-and-child-health-sharpened-plan-for-uganda/ (accessed on 4 November 2013).
- The Republic of Uganda. Final Millennium Development Goals Report for Uganda 2015. Available online: http://www.ug.undp.org/content/uganda/en/home/library/mdg/final-millennium-development-goals-report-for-uganda-2015.htmlDfa (accessed on 29 October 2015).
- Haines, A.; Sanders, D.; Lehmann, U.; Rowe, A.K.; Lawn, J.E.; Jan, S.; Walker, D.G.; Bhutta, Z. Achieving child survival goals: Potential contribution of community health workers. Lancet 2007, 369, 2121–2131. [Google Scholar] [CrossRef]
- Serbanescu, F.; Goodwin, M.M.; Binzen, S.; Morof, D.; Asiimwe, A.R.; Kelly, L.; Wakefield, C.; Picho, B.; Healey, J.; Nalutaaya, A.; et al. Addressing the First Delay in Saving Mothers, Giving Life Districts in Uganda and Zambia: Approaches and Results for Increasing Demand for Facility Delivery Services. Glob. Health Sci. Pract. 2019, 7, S48–S67. [Google Scholar] [CrossRef]
- Uganda Bureau of Statistics Kampala. Uganda Demographic and Health Survey 2016. Available online: https://www.health.go.ug/sites/default/files/Demographic%20and%20Health%20Survey.pdf (accessed on 1 March 2017).
- Tweheyo, R.; Konde-Lule, J.; Tumwesigye, N.M.; Sekandi, J.N. Male partner attendance of skilled antenatal care in peri-urban Gulu district, Northern Uganda. BMC Pregnancy Childbirth 2010, 10, 53–62. [Google Scholar] [CrossRef] [PubMed]
- MOH. Participants Manual for Village Health Team Members; MOH: Kampala, Uganda, 2008. [Google Scholar]
- World Vision. TTC-A Family-Inclusive Behaviour Change Model for the Life-course. Available online: http://www.wvi.org/health/timed-and-targeted-counseling-ttc (accessed on 23 June 2018).
- UNFPA, 2014, How the Government and Organizations Have Disseminated and Applied the Technical Guidance on the Human Rights Based Approach To Eliminating Preventable Maternal Mortality and Morbidity in Humanitarian Settings. Available online: https://www.ohchr.org/Documents/Issues/Women/WRGS/FollowUp2018/UNFPA_DRC.pdf (accessed on 1 June 2014).
- The Republic of Uganda. National Population and Housing Census 2014–Area Specific Profile Series (Hoima District). Available online: https://www.ubos.org/wp-content/uploads/publications/2014CensusProfiles/HOIMA.pdf (accessed on 1 April 2017).
- The Republic of Uganda. National Population and Housing Census 2014–Area Specific Profile Series (Masindi District). Available online: https://www.ubos.org/wp-content/uploads/publications/2014CensusProfiles/MASINDI.pdf (accessed on 1 April 2017).
- Ministry of Health Knowledge Management Portal. Village Health Team: Strategy and Operational Guidelines. Available online: http://library.health.go.ug/publications/health-education/village-health-team-strategy-and-operational-guidelines (accessed on 19 March 2010).
- Tran, N.T.; Portela, A.; de Bernis, L.; Beek, K. Developing Capacities of Community Health Workers in Sexual and Reproductive, Maternal, Newborn, Child, and Adolescent Health: A Mapping and Review of Training Resources. PLoS ONE 2014, 15, e94948. [Google Scholar] [CrossRef]
- World Vision International, 2018, Timed and Targeted Counselling for Health & Nutrition (2nd Edition): A Comprehensive Training Course for Community Health Workers. Available online: https://www.wvi.org/sites/default/files/ttCFacilitatorsManual_Methodology.FINAL_.pdf (accessed on 1 January 2018).
- World Vision Uganda. Directorate of Health, Nutrition and HIV: Implementation Guidelines for the Timed and Targeted Counselling; World Vision Uganda: Kampala, Uganda, 2014. [Google Scholar]
- Ministry of Health. Essential Maternal and Neonatal Clinical Care Guidelines; Ministry of Health: Kampala, Uganda, 2009. [Google Scholar]
- MOH. Road Map for Accelerating the Reduction of Maternal and Neonatal Mortality and Morbidity in Uganda; Report; MOH: Kampala, Uganda, 2008. [Google Scholar]
- UNFPA Uganda. The Mama Kit Innovator. Available online: https://uganda.unfpa.org/en/news/mama-kit-innovator (accessed on 16 October 2012).
- Ministry of Health. VHT/ICCM Register for Uganda; Ministry of Health: Kampala, Uganda, 2010. [Google Scholar]
- BMAU, Ministry of Finance, Planning and Economic Development, Health Workers’ Shortage in Uganda: Where Should the Government Focus Its Efforts? 2013. Available online: http://www.finance.go.ug/dmdocuments/6-13%20Health%20Workers%20Shortage%20in%20Uganda%20May%202013.pdf (accessed on 16 October 2012).
- Ministry of Health. Government of Uganda: Mother and Child Passport; Ministry of Health: Kampala, Uganda, 2012. [Google Scholar]
- Campbell, M.J.; Walters, S.J. How to Design, Analyze and Report Cluster Randomized Trials in Medicine and Health Related Research; John Wiley & Sons Ltd.: Chichester, UK, 2014. [Google Scholar]
- The Center for Health Statistics, Statistical Analysis Division. Alabama Vital Statistics; Alabama Department of Public Health Center for Health Statistics Division of Statistical Analysis Post Office Box: Montgomery, AL, USA, 2004.
- Ministry of Health, 2018, Health Management Information System (HMIS) in Uganda. Available online: https://mets.or.ug/health-management-information-system-hmis-in-uganda/ (accessed on 9 February 2018).
- World Health Organization. Social Determinants of Sexual and Reproductive Health: Informing Future Research and Programmer Implementation; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Richard, M.K. Explainer: Local Government Structures in Uganda. 2010. Available online: https://www.theguardian.com/katine/2009/dec/14/local-government-explainer (accessed on 14 December 2009).
- Kyaddondo, D.; Mugerwa, K.; Byamugisha, J.; Oladapo, O.T.; Bohren, M.A. Expectations and needs of Ugandan women for improved quality of childbirth care in health facilities: A qualitative study. Int. J. Gynecol. Obs. 2017, 139, 38–46. [Google Scholar] [CrossRef]
- Dantas, J.A.R.; Singh, D.; Lample, M. Factors affecting utilization of health facilities for labour and childbirth: A case study from rural Uganda. BMC Pregnancy Childbirth 2020, 20, 39. [Google Scholar] [CrossRef] [PubMed]
| Visit | Timing | Services Delivered by the VHTs |
|---|---|---|
| 1 | Before or at 3 months | Focuses on suspected pregnant mothers registered as ttC candidates. They are counselled on how to care for themselves during pregnancy, a list of danger signs during pregnancy is explained, and the family is encouraged to notify the VHT in the case of any of these danger signs. Families are counselled on what to do during pregnancy and when giving birth. Women pregnant for less than three months are advised to start antenatal care at three months. |
| 2 | At 4 months of pregnancy | This is to affirm that the pregnant mother went for ANC. The pregnant women are encouraged to go for the second ANC visit. Pregnant women are educated on the advantages of exclusive breastfeeding of children until 6 months of age and continuous breastfeeding until they reach the age of 2. Advantages of giving birth in a health facility and hand washing will be highlighted during this visit. |
| 3 | At 6 months of pregnancy | Discuss the birth plan, timing and place of the birth, exploring potential challenges faced by expectant mothers in reaching the health facility and ways of overcoming these challenges. Expectant mothers are given information on the different family planning methods and where to go for services, and are encouraged to utilize one of the methods after delivery. |
| 4 | 8 months of pregnancy | The mother is educated about the early signs of true labor, danger signs during labor will be explained to the households, as well as appropriate action to take in the case of these danger signs. The mother is also encouraged to deliver at a health facility and have some emergency money available. This is also the visit at which the mother needs to have a clean birthing kit available (the “Mama Kit” [23]). |
| 5–7 | The newborn period | This visit is done three times in the first week after birth, on Days 1, 3 and 7. The VHT ensures that exclusive breastfeeding and essential maternal and newborn care are not only understood but also practiced. Mothers are educated on the need to seek health care if the neonate develops fever and/or a cough, and the need to go for routine growth monitoring and immunization. |
| 8 | When the baby is one month and 2 weeks | Malaria prevention is discussed here, as well as other illnesses, danger signs in the baby and immunization for the baby and hygiene practices. The VHT checks whether the child’s growth card has been plotted, gives support for exclusive breastfeeding, checks if the child has had its HIV confirmatory test as part of the prevention of mother-to-child transition of HIV program and whether the mother has any ideas about family planning methods. |
| Visit | Timing | Services Delivered by the VHTs |
|---|---|---|
| ANC | Pregnancy period | Ensuring that mothers actually attend ANC as early as required to acquire the initial goal-oriented services. Making the four visits to the household with a pregnant woman. |
| Newborn | Newborn (28 days) | Ensuring that the cord is healing, the baby is breastfeeding and that the initial immunization has been given to the child. Ensuring that the birth took place at the health facility and—if the birth happened at home—the VHT refers the mother and baby pair to the facility. |
| PNC | Postnatal period | Checking on the 6th hour that the health worker gives PNC. Visit the household around the 6th day and visit around 6 weeks after delivery to check whether the mother has plans of having the last PNC visit. |
| Immunization | Up to 9 months after birth | Conduct household mobilization visits to check on the completeness and preparedness for child immunization [26]. The Day 1 visit is for the VHT to check on the first day immunization. The VHT visits the household at around the 6th week after birth and then at around 10 weeks and 14 weeks after delivery. |
| Study Period | ||||||||
|---|---|---|---|---|---|---|---|---|
| Enrolment | Allocation | Post-Allocation | Close-Out | |||||
| TIMEPOINT | Feb’19 | Nov’19 | Jan’20 | Jun’20 | Jan’21 | Jun’21 | Jan’22 | Feb’22 |
| Enrolment | ||||||||
| Eligibility screen | X | X | X | X | X | |||
| Informed consent | X | X | X | X | X | X | ||
| Allocation | X | X | X | X | X | |||
| Interventions | ||||||||
| [ttC implementation] | X | X | X | X | X | |||
| [Control implementation] | X | X | X | X | X | |||
| Assessments | ||||||||
| Baseline | X | X | ||||||
| MTR Outcomes | X | X | ||||||
| ETR Outcome | X | |||||||
| No | Variable | Description of Variable | Tool to Be Used |
|---|---|---|---|
| Dependent Variables | |||
| 1 | Appropriate pregnancy weight gain at end of months pregnancy | Pregnancy weight gain of 11.5 kg to 16 kg by the end of the pregnancy | SQ |
| 2 | Newborn morbidity within the first 28 days of life | Newborn morbidity (focusing on cord infections, sepsis, asphyxia, fever, common flu and cold and diarrhea, pneumonia) within the first 28 days of life | SQ and ttCR |
| 3 | Appropriate birth weight | Appropriate birth weight of 2.5 kg or more | SQ |
| 4 | Mortality of newborns and mothers | If the mother died during pregnancy or childbirth, if the baby died either during pregnancy, childbirth or within the first 28 days of life. | SQ and ttCR |
| 5 | Overall maternal wellness | During pregnancy or newborn period, a mother does not develop sepsis, urinary tract infections, obstruction during birth or any danger signs during this period. | SQ and ttCR |
| Independent Variables | |||
| 1 | Uptake of timely goal-oriented ANC | With a focus on the recommended four visits, the associated recommended services offered during these visits and timeliness of attendance. | VHTR, SQ and ttCR |
| 2 | Clean birthing practices | Birth attended by a skilled health provider, delivery happened in a health facility and a mama kit was used during the process. | SQ and ttCR |
| 3 | Essential newborn care practices (ENC) during the newborn period | Early initiation of breastfeeding, cord care practices, baby thermal care, sustained breastfeeding and baby WASH practices. | SQ and ttCR |
| 4 | Positive male involvement in pregnancy and newborn care | Man participates in at least one ANC, does an HIV test with the mother, available during birth, supports mother to help her rest, contributes finances for related logistics. | SQ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babughirana, G.; Gerards, S.; Mokori, A.; Musasizi, B.; Isabirye, N.; Baigereza, I.C.; Rukanda, G.; Bussaja, E.; Kremers, S.; Gubbels, J. Effects of Implementing the Timed and Targeted Counselling Model on Pregnancy Outcomes and Newborn Survival in Rural Uganda: Protocol for a Quasi-Experimental Study. Methods Protoc. 2020, 3, 73. https://doi.org/10.3390/mps3040073
Babughirana G, Gerards S, Mokori A, Musasizi B, Isabirye N, Baigereza IC, Rukanda G, Bussaja E, Kremers S, Gubbels J. Effects of Implementing the Timed and Targeted Counselling Model on Pregnancy Outcomes and Newborn Survival in Rural Uganda: Protocol for a Quasi-Experimental Study. Methods and Protocols. 2020; 3(4):73. https://doi.org/10.3390/mps3040073
Chicago/Turabian StyleBabughirana, Geoffrey, Sanne Gerards, Alex Mokori, Benon Musasizi, Nathan Isabirye, Isaac Charles Baigereza, Grace Rukanda, Emmanuel Bussaja, Stef Kremers, and Jessica Gubbels. 2020. "Effects of Implementing the Timed and Targeted Counselling Model on Pregnancy Outcomes and Newborn Survival in Rural Uganda: Protocol for a Quasi-Experimental Study" Methods and Protocols 3, no. 4: 73. https://doi.org/10.3390/mps3040073
APA StyleBabughirana, G., Gerards, S., Mokori, A., Musasizi, B., Isabirye, N., Baigereza, I. C., Rukanda, G., Bussaja, E., Kremers, S., & Gubbels, J. (2020). Effects of Implementing the Timed and Targeted Counselling Model on Pregnancy Outcomes and Newborn Survival in Rural Uganda: Protocol for a Quasi-Experimental Study. Methods and Protocols, 3(4), 73. https://doi.org/10.3390/mps3040073





