Patients’ Perception of Childbirth According to the Delivery Method: The Experience in Our Clinic
Highlights
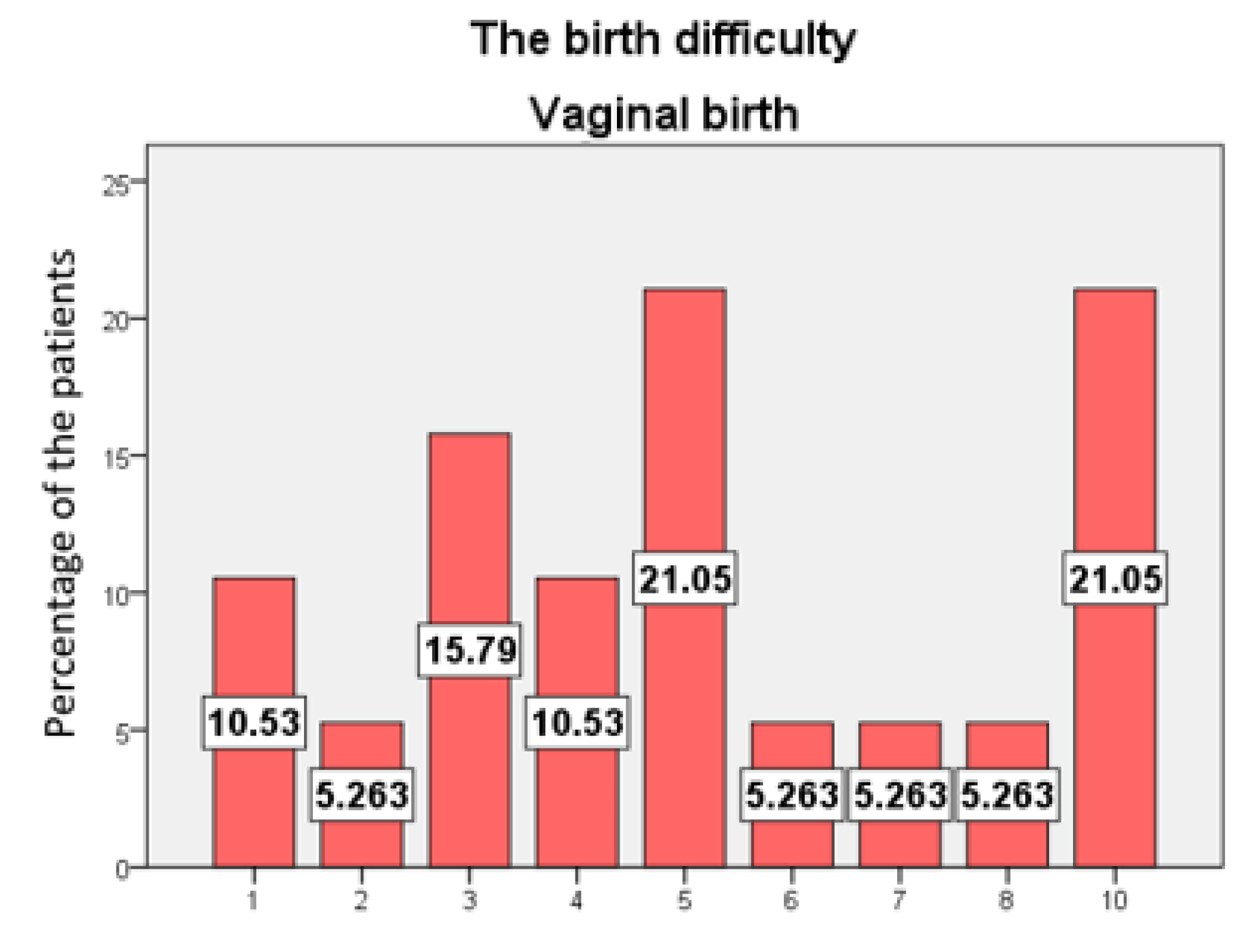
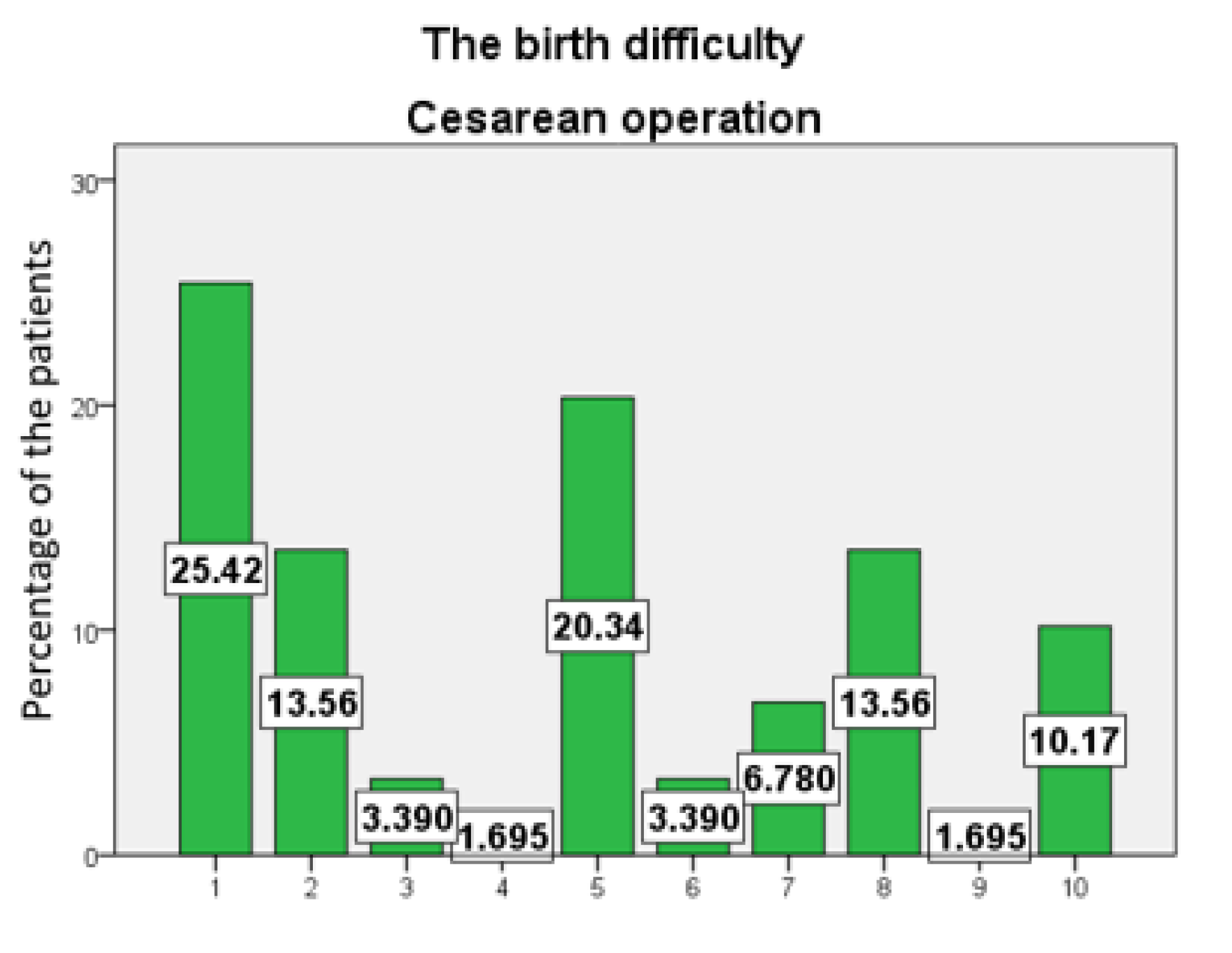
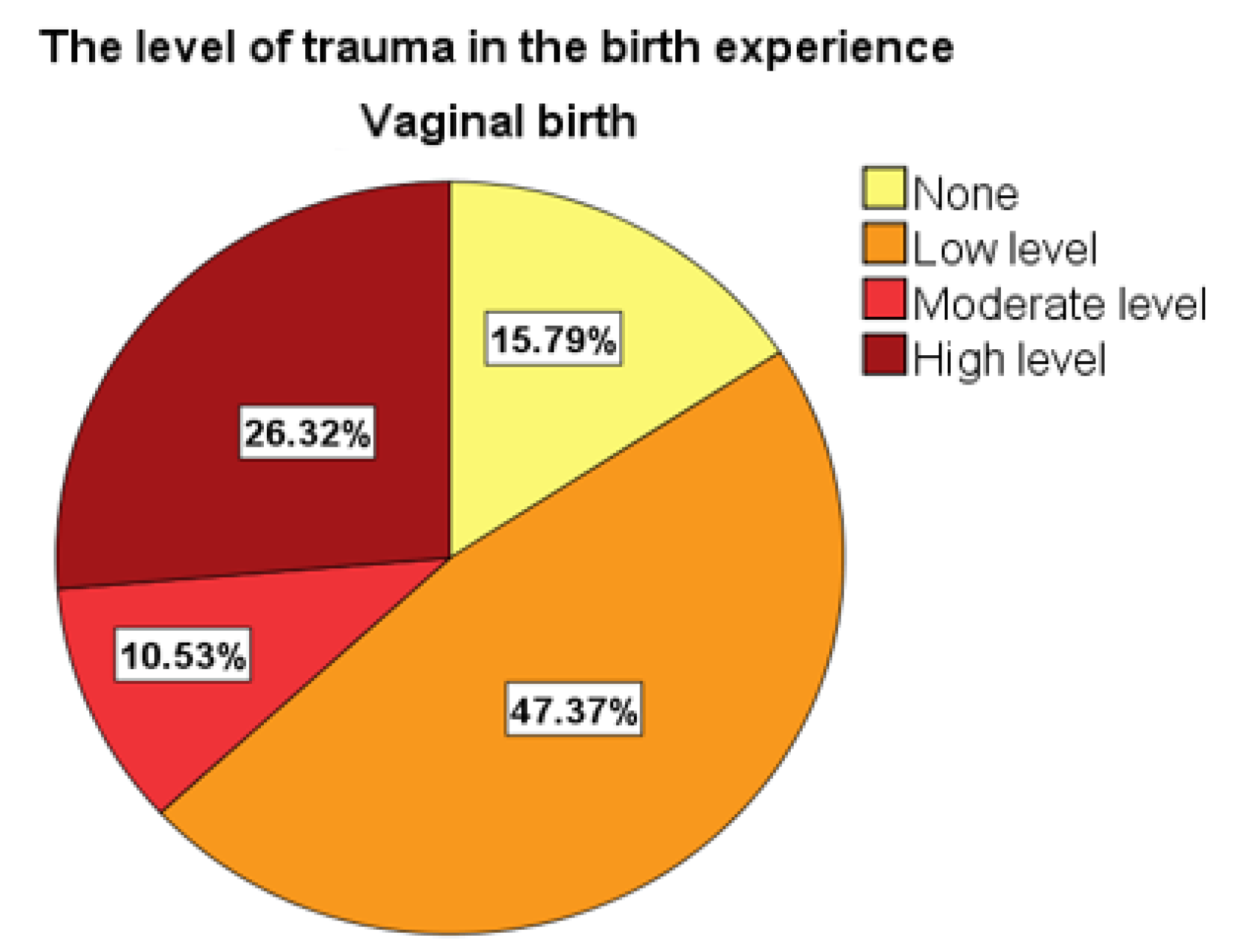
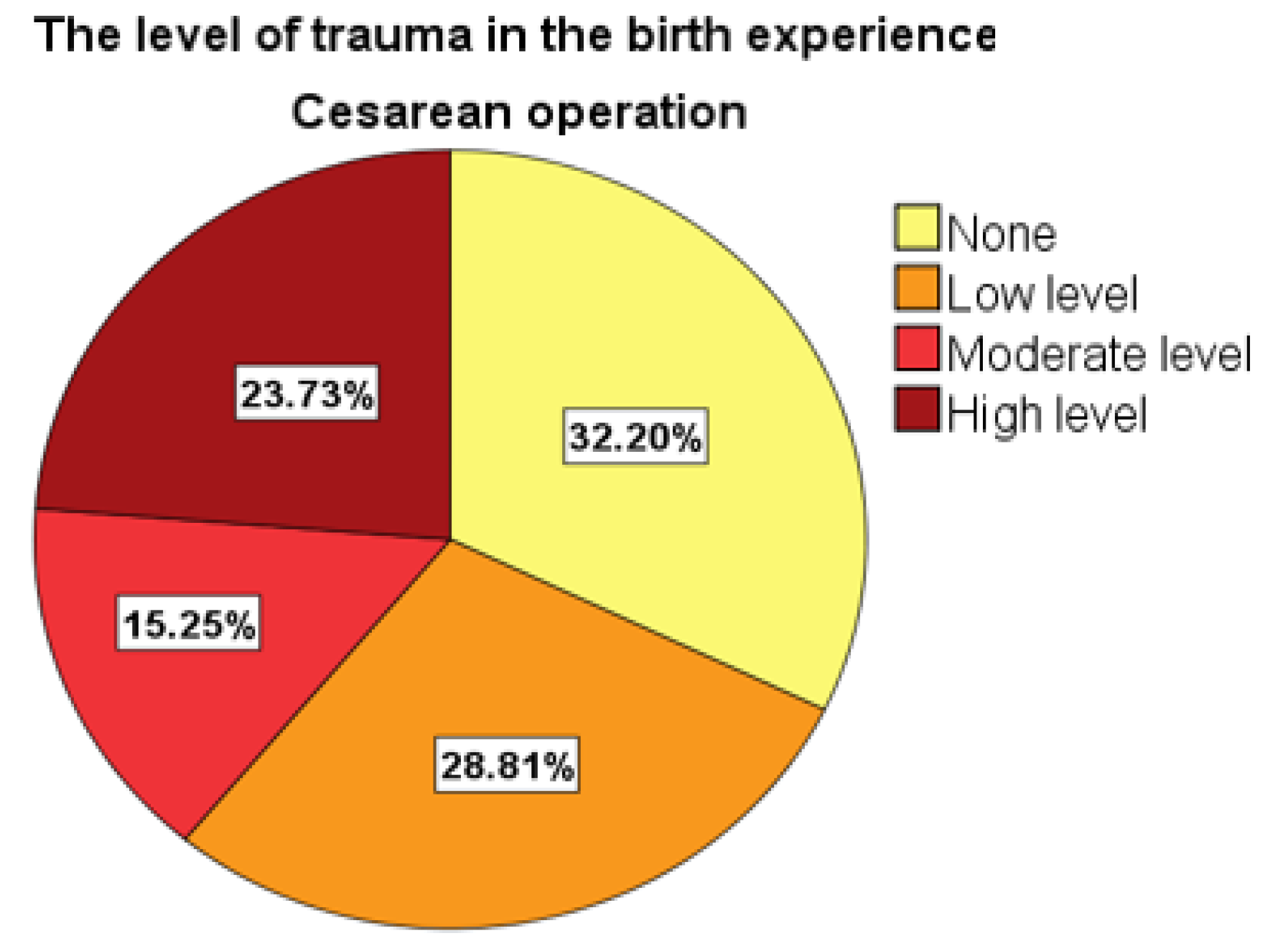
- Patients who gave birth vaginally assigned the maximum degree to the difficulty of birth, compared with patients who gave birth through cesarean section.
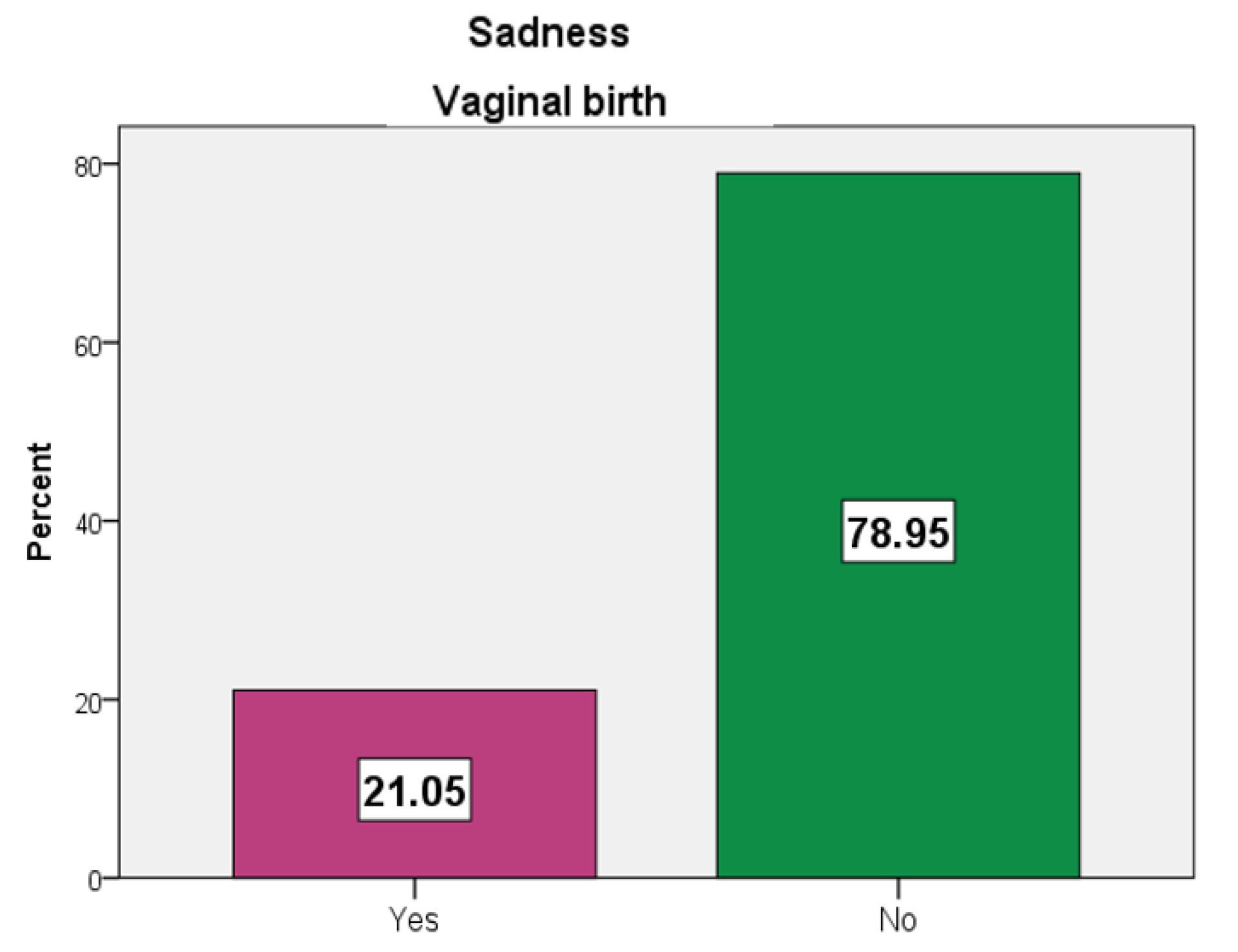
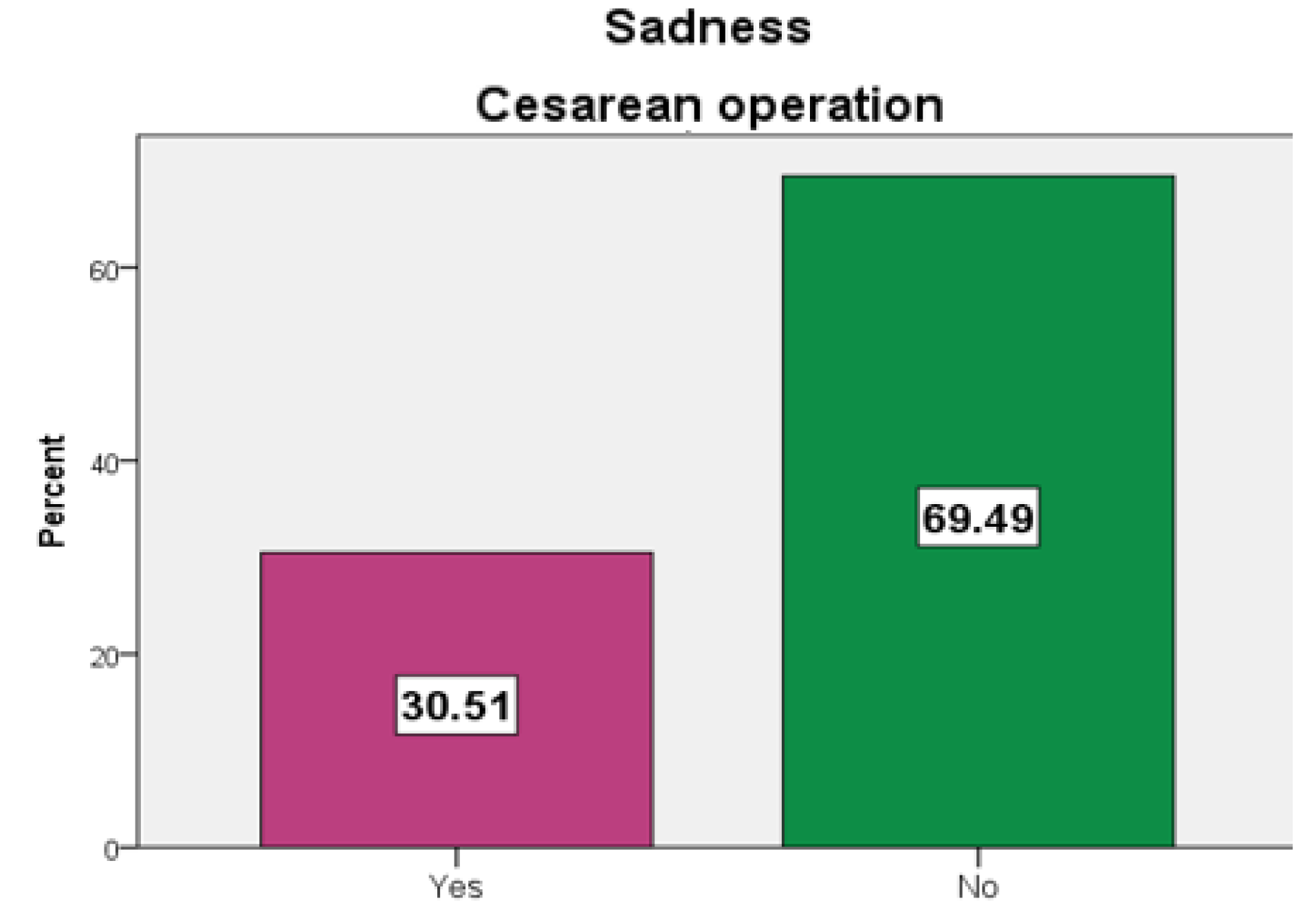
- Patients who gave birth through cesarean section experienced the feeling of sadness more than those who gave birth vaginally.
Abstract
:Highlights
- Patients who gave birth vaginally assigned the maximum degree to the difficulty of birth, compared with patients who gave birth through cesarean section.
- Patients who gave birth through cesarean section experienced the feeling of sadness more than those who gave birth vaginally.
Abstract
Introduction
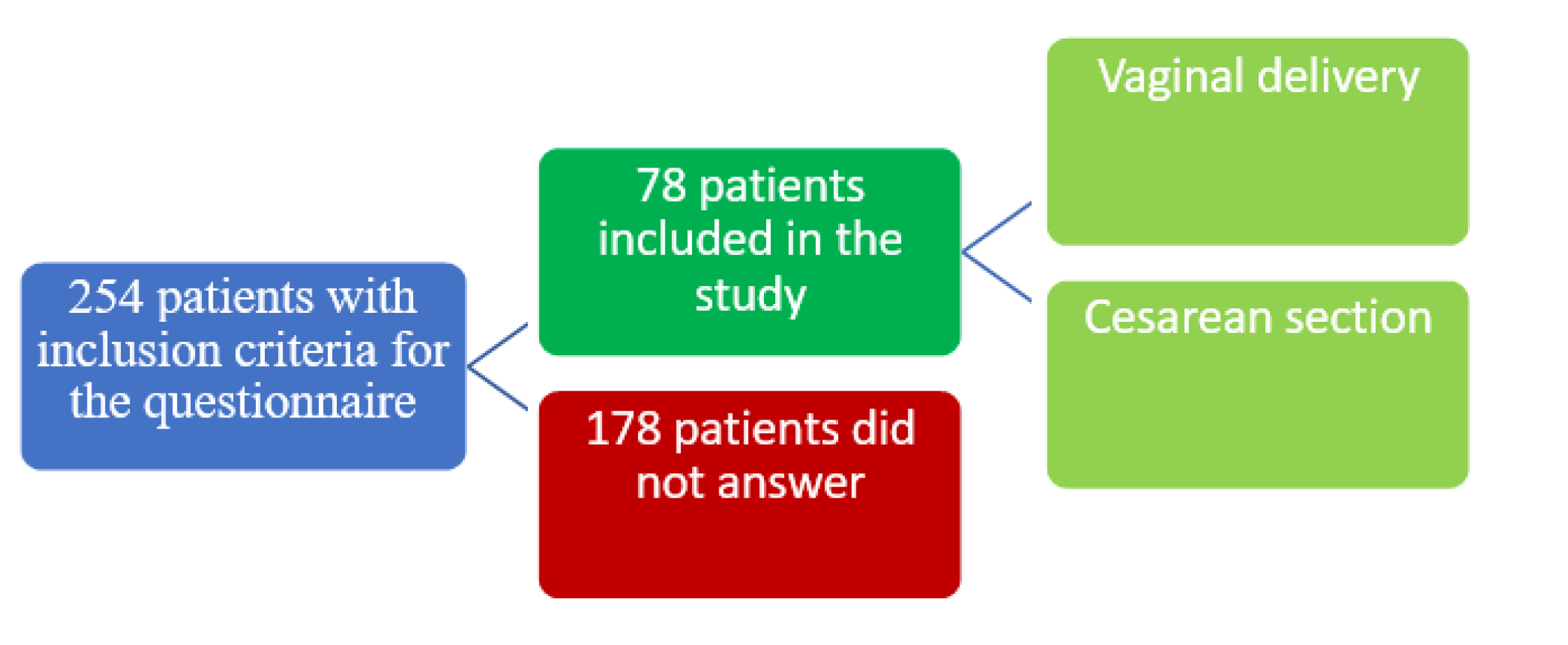
Materials and Methods
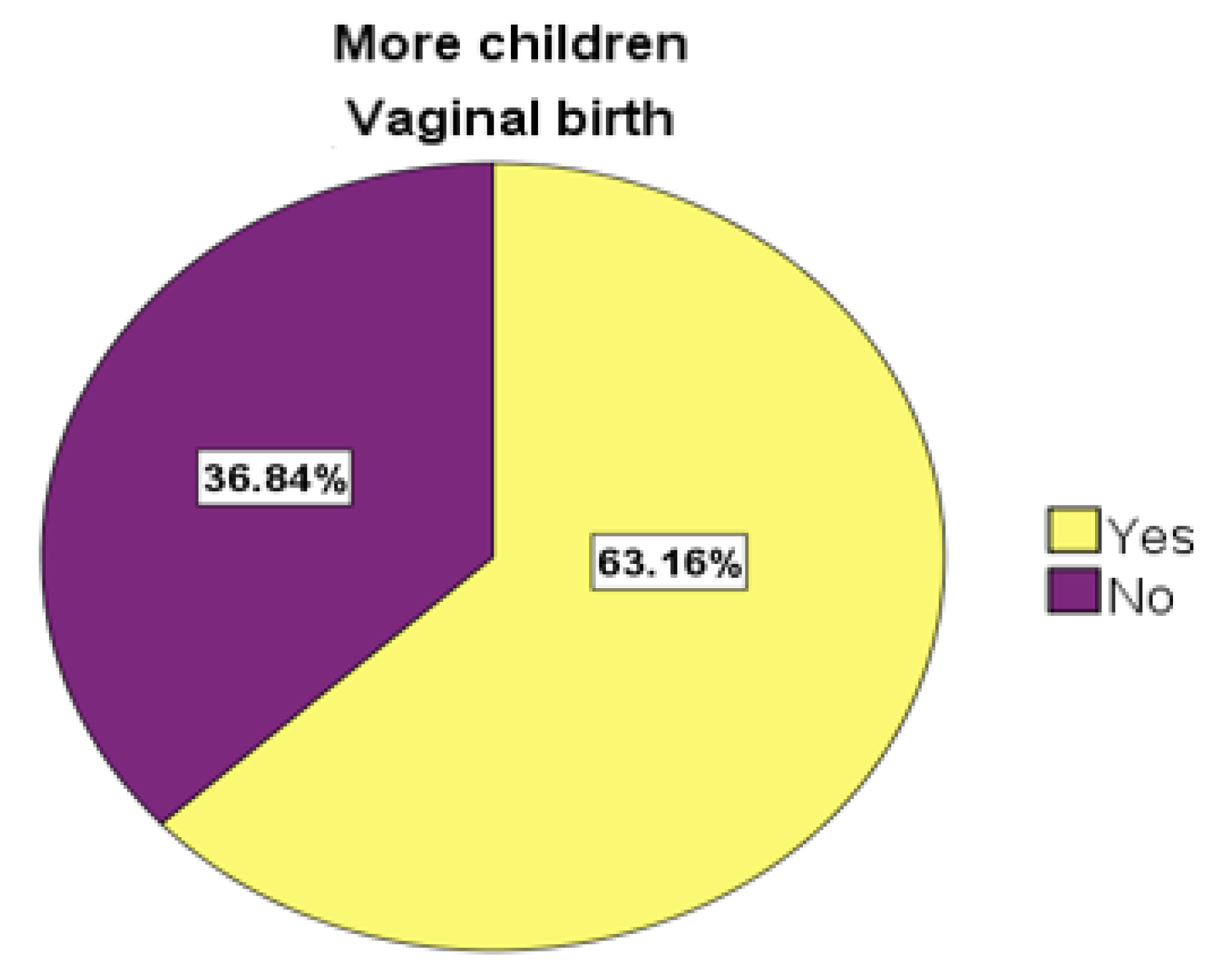
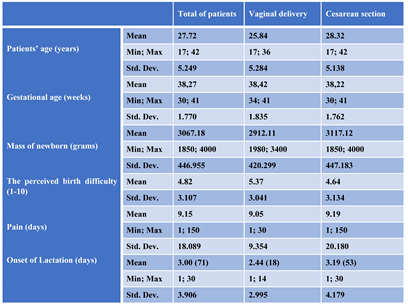
Results
Discussions
Conclusions
Conflict of interest disclosure
Compliance with ethical standards
References
- Skinner, E.M.; Barnett, B.; Dietz, H.P. Psychological consequences of pelvic floor trauma following vaginal birth: a qualitative study from two Australian tertiary maternity units. Arch Womens Ment Health. 2017, 21, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Nystedt, A.; Hildingsson, I. Women's and men's negative experience of child birth-A cross-sectional survey. Women Birth 2017, pii: S1871-5192(17)30056-2. [Google Scholar] [CrossRef]
- Boero, G.; Biggio, F.; Pisu, M.G.; Locci, V.; Porcu, P.; Serra, M. Combined effect of gestational stress and postpartum stress on maternal care in rats. Physiol Behav 2018, 184, 172–178. [Google Scholar] [CrossRef]
- Johnstone, S.J.; Boyce, P.M.; Hickey, A.R.; Morris-Yatees, A.D.; Harris, M.G. Obstetric risk factors for postnatal depression in urban and rural community samples. Aust N Z J Psychiatry. 2001, 35, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Nagle, U.; Farrelly, M. Women's views and experiences of having their mental health needs considered in the perinatal period. Midwifery 2018, 66, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Holden, L.; Hockey, R.; Ware, R.S.; Lee, C. Mental health- related quality of life and the timing of motherhood: a 16-year longitudinal study of a national cohort of young Australian women. Qual Life Res. 2018, 27, 923–935. [Google Scholar] [CrossRef]
- World Health Organization, Maternal and Newborn Health/Safe Motherhood Unit. Care in normal birth: a practical guide. Available online: http://www.who.int/maternal_child_adolescent/documents/who_frh_msm_9624/en/ (accessed on 1 May 2020).
- Glazener, C.M.; Abdalla, M.; Stroud, P.; Naji, S.; Templeton, A.; Russell, I.T. Postnatal maternal morbidity: extent, causes, prevention and treatment. Br J Obstet Gynaecol. 1995, 102, 282–7. [Google Scholar] [CrossRef]
- Fisher, J.; Astbury, J.; Smith, A. Adverse psychological impact of operative obstetric interventions: a prospective longitudinal study. Aust N Z J Psychiatry. 1997, 31, 728–38. [Google Scholar] [CrossRef]
- Boyce, P.M.; Todd, A.L. Increased risk of postnatal depression after emergency caesarean section. Med J Aust. 1992, 157, 172–4. [Google Scholar] [CrossRef]
- Culp, R.E.; Osofsky, H.J. Effects of cesarean delivery on parental depression, marital adjustment, and mother- infant interaction. Birth. 1989, 16, 53–7. [Google Scholar] [CrossRef]
- Saisto, T.; Salmela-Aro, K.; Nurmi, J.E.; Halmesmaki, E. Psychosocial predictors of disappointment with delivery and puerperal depression. A longitudinal study. Acta Obstet Gynecol Scand. 2001, 80, 39–45. [Google Scholar] [CrossRef]
- Ranjit, A.; Jiang, W.; Little, S.; Witkop, C.; Haider, A.; Robinson, J. Outcomes of Mothers and Children at Five Years After Cesarean Versus Vaginal Delivery. Obstetrics/Gynecology 2018, 131, 58s. [Google Scholar] [CrossRef]
- Gulden, A.; Top, E.D. Maternal attachment and breastfeeding behaviors according to type of delivery in the immediate postpartum period. Rev Assoc Med Bras (1992). 2018, 64, 164–169. [Google Scholar] [CrossRef]
- Strunck, M.; Bachmann, G. Teaching Optimism During Pregnancy: A Possible Protective Practice Against Postpartum Depression. Obstetrics & Gynecology 2018, 131, 133s. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. (2018, June). Retrieved , 2018. Available online: https://www.cdc.gov/reproductivehealth/depression/in dex (accessed on 29 July 2018).
- Rowland, D.L.; Motofei, I.G.; Popa, F.; Constantin, V.D.; Vasilache, A.; Păunică, I.; Bălălău, C.; Păunică, P.G.; Banu, P.; Păunică, S. The postfinasteride syndrome; an overview. J Mind Med Sci. 2016, 3, 99–107. [Google Scholar] [CrossRef]
- Saisto, T.; Salmela-Aro, K.; Nurmi, J.E.; Halmesmaki, E. Psychosocial predictors of disappointment with delivery and puerperal depression. A longitudinal study. Acta Obstet Gynecol Scand. 2001, 80, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.E.; Wiltsey-Stirman, S.; Sikorskii, A.; Miller, T.; King, A.; Blume, J.L.; Pham, X.; Moore Simas, T.A.; Poleshuck, E.; Weinberg, R.; Zlotnick, C. Protocol for the ROSE sustainment (ROSES) study, a sequential multiple assignment randomized trial to determine the minimum necessary intervention to maintain a postpartum depression prevention program in prenatal clinics serving low-income women. Implement Sci. 2018, 13, 115. [Google Scholar] [CrossRef]
- Stanescu, A.D.; Balalau, D.O.; Ples, L.; Paunica, S.; Balalau, C. Postpartum depression: Prevention and multimodal therapy. Journal of Mind and Medical Sciences. 2018, 5, 163–168. [Google Scholar] [CrossRef]
- Burgio, K.L.; Zyczynski, H.; Locher, J.L.; Richter, H.E.; Redden, D.T.; Wright, K.C. Urinary incontinence in the 12-month postpartum period. Obstetrics & Gynecology. 2003, 102, 1291–1298. [Google Scholar] [CrossRef]
- Declercq, E.R.; Sakala, C.; Corry, M.P.; Applebaum, S.; Herrlich, A. Major survey findings of Listening to Mothers III: New Mothers Speak Out: Report of National Surveys of Women’s Childbearing Experiences. J Perinat Educ. 2014, 23, 17–24. [Google Scholar] [CrossRef]
- Haran, C.; van Driel, M.; Mitchell, B.L.; Brobdribb, W.E. Clinical guidelines for postpartum women and infants in primary care—a systematic review. BMC Pregnancy Childbirth 2014, 14, 51. [Google Scholar] [CrossRef] [PubMed]
- Practice, A.C. Optimizing Postpartum Care. Obstet Gynecol. 2016, 127, 187–192. [Google Scholar] [CrossRef]
- Laudenbach, V.; Mercier, F.J.; Rozé, J.C.; et al. Anaesthesia mode for caesarean section and mortality in very preterm infants: an epidemiologic study in the EPIPAGE cohort. Int J Obstet Anesth. 2009, 18, 142–9. [Google Scholar] [CrossRef]
- Balalau, D.O.; Sima, R.M.; Bacalbașa, N.; Pleș, L.; Stănescu, A.D. Emergency peripartum hysterectomy, physical and mental consequences: a 6-year study. J Mind Med Sci. 2016, 3, 65–70. [Google Scholar]
- Rhoades, D.A.; Latza, U.; Mueller, B.A. Risk factors and outcomes associated with nuchal cord. A population- based study. J Reprod Med. 1999, 44, 39–45. [Google Scholar] [PubMed]
- Pleș, L.; Beliș, V.; Rîcu, A.; Sima, R.M. Medico-legal issues of the nuchal cord at birth. Journal of Romanian Legal Medicine. 2016, 24, 289–293. [Google Scholar]
- Ionescu, C.A.; Ples, L.; Banacu, M.; Poenaru, E.; Panaitescu, E.; Traian Dimitriu, M.C. Present tendencies of elective caesarean delivery in Romania: Geographic, social and economic factors. J Pak Med Assoc. 2017, 67, 1248–1253. [Google Scholar]
 |
© 2019 by the authors. 2019 Camelia Alexandroaia, Romina-Marina Sima, Oana-Denisa Bălălău, Gabriel-Octavian Olaru, Liana Pleş
Share and Cite
Alexandroaia, C.; Sima, R.-M.; Bălălău, O.-D.; Olaru, G.-O.; Pleş, L. Patients’ Perception of Childbirth According to the Delivery Method: The Experience in Our Clinic. J. Mind Med. Sci. 2019, 6, 311-318. https://doi.org/10.22543/7674.62.P311318
Alexandroaia C, Sima R-M, Bălălău O-D, Olaru G-O, Pleş L. Patients’ Perception of Childbirth According to the Delivery Method: The Experience in Our Clinic. Journal of Mind and Medical Sciences. 2019; 6(2):311-318. https://doi.org/10.22543/7674.62.P311318
Chicago/Turabian StyleAlexandroaia, Camelia, Romina-Marina Sima, Oana-Denisa Bălălău, Gabriel-Octavian Olaru, and Liana Pleş. 2019. "Patients’ Perception of Childbirth According to the Delivery Method: The Experience in Our Clinic" Journal of Mind and Medical Sciences 6, no. 2: 311-318. https://doi.org/10.22543/7674.62.P311318
APA StyleAlexandroaia, C., Sima, R.-M., Bălălău, O.-D., Olaru, G.-O., & Pleş, L. (2019). Patients’ Perception of Childbirth According to the Delivery Method: The Experience in Our Clinic. Journal of Mind and Medical Sciences, 6(2), 311-318. https://doi.org/10.22543/7674.62.P311318



