Histopathology Report on Colon Cancer Specimens—Measuring Surgical Quality, an Increasing Stress for Surgeons
Highlights
- A single value of 12 lymph nodes should not be viewed as a benchmark for quality of colon surgery.
- The current standards on colon resections need to be reevaluated; a more flexible algorithm should be developed for assessment of surgical performance.
Abstract
Highlights
- A single value of 12 lymph nodes should not be viewed as a benchmark for quality of colon surgery.
- The current standards on colon resections need to be reevaluated; a more flexible algorithm should be developed for assessment of surgical performance.
Abstract
Introduction
Materials and Methods
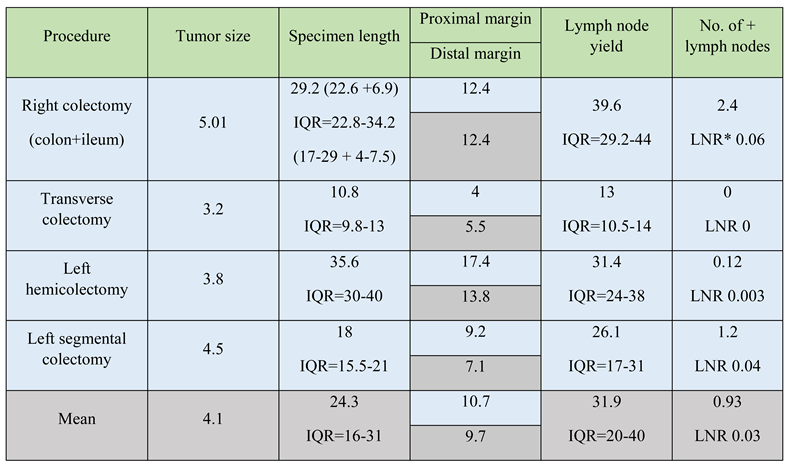
Results
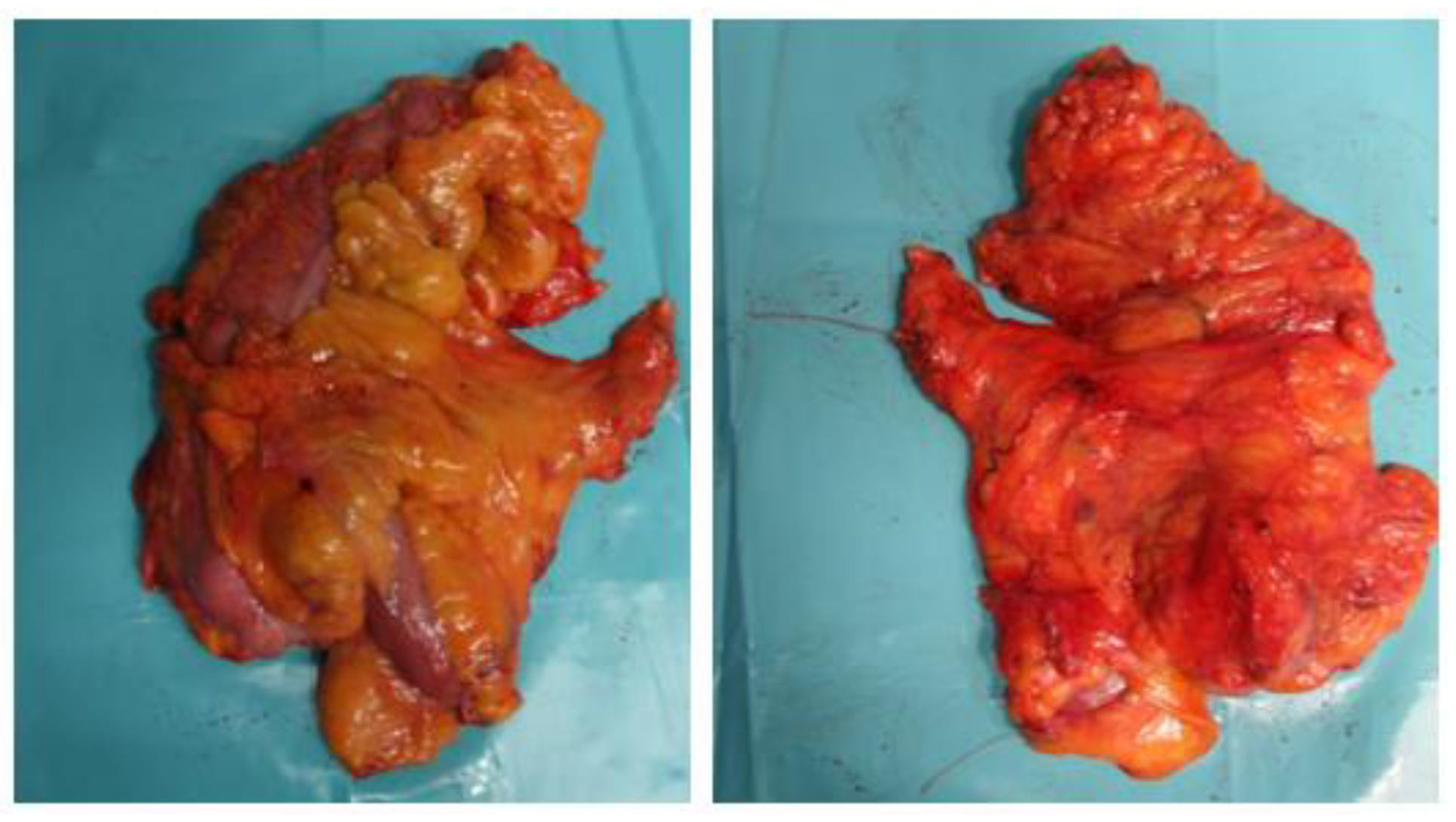
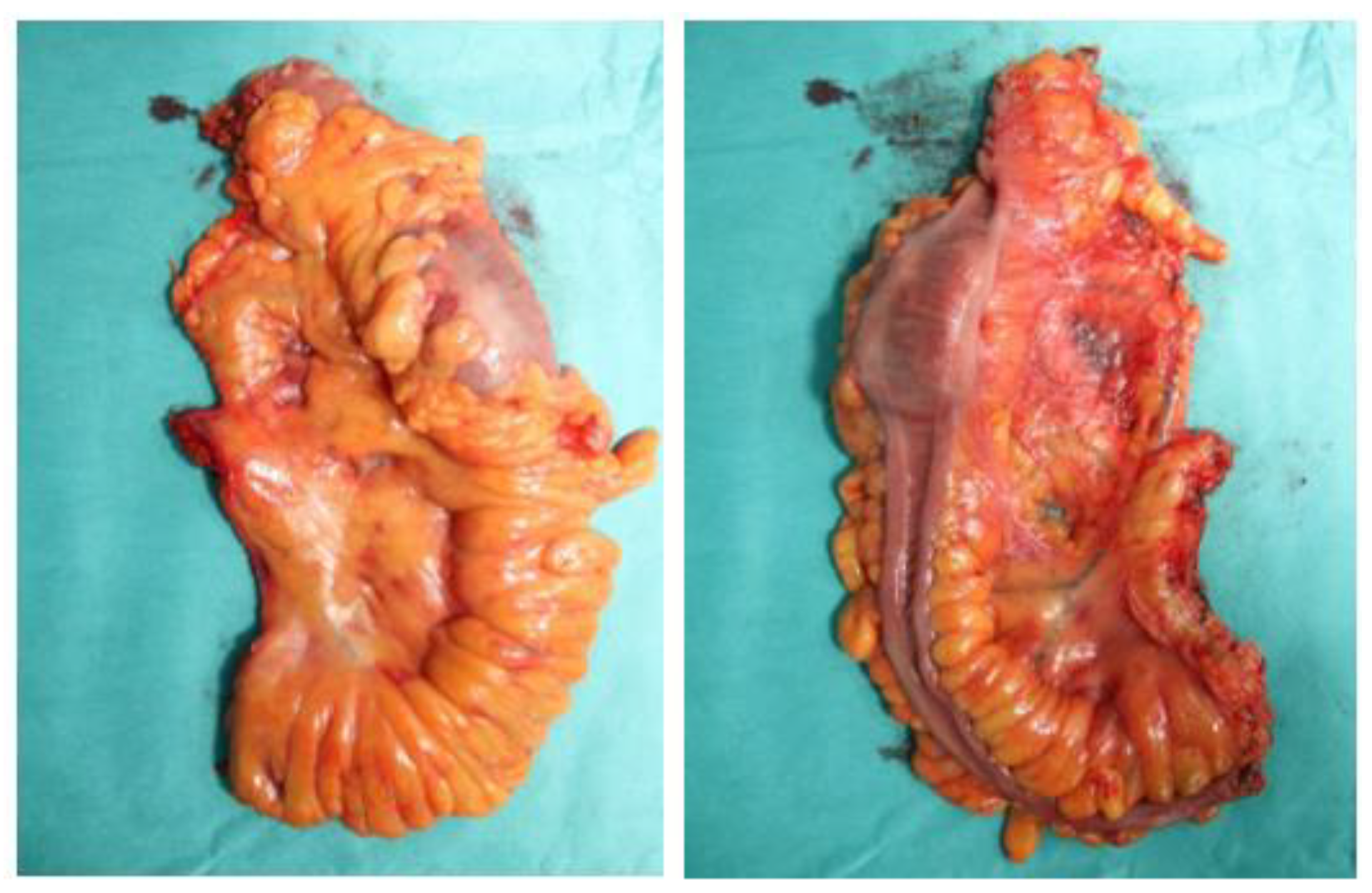
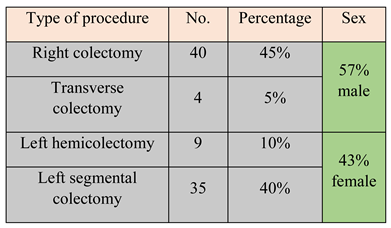
Surgical technique
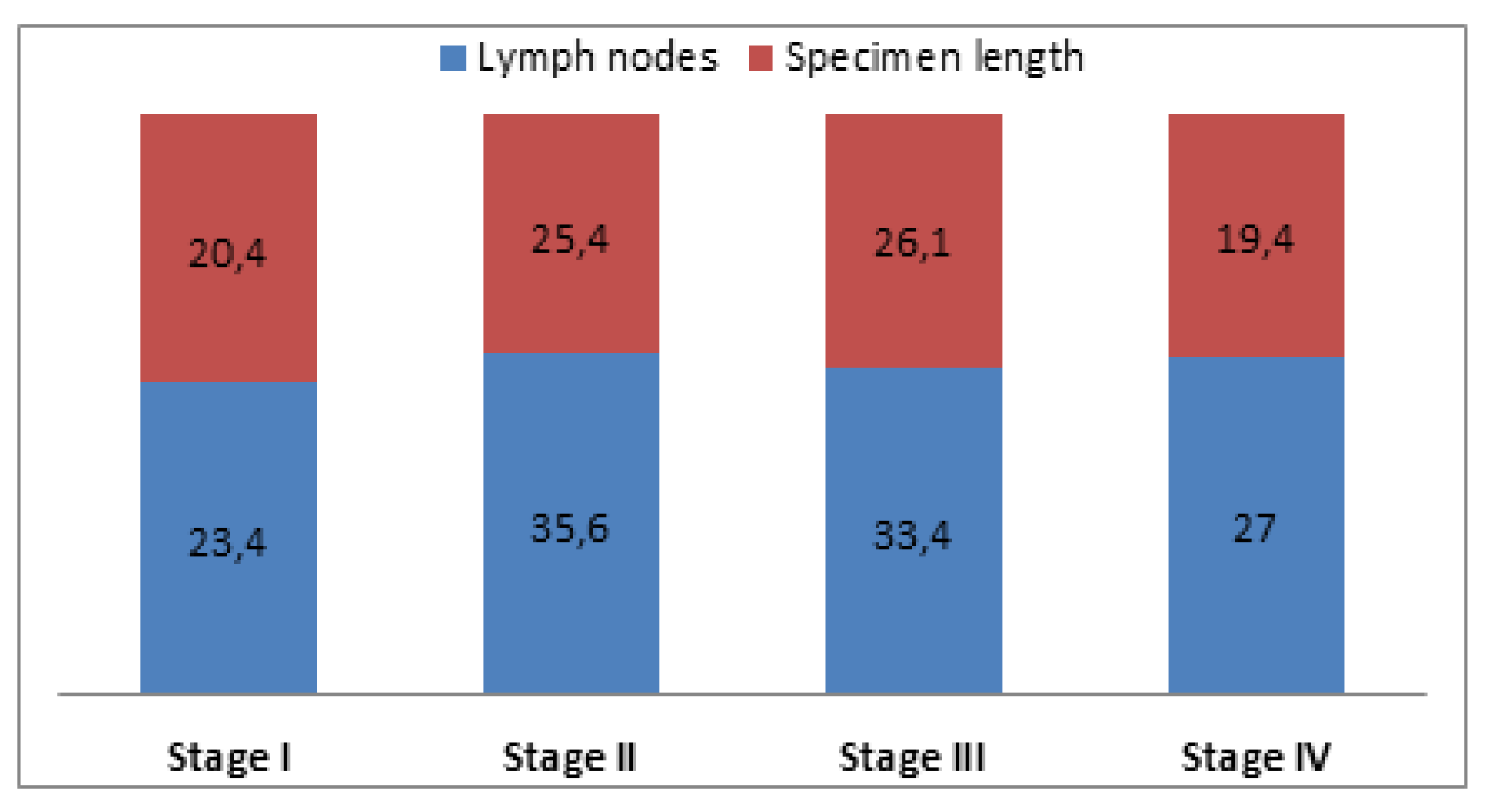
Clinicopathological outcomes
Discussion
Conclusions
References
- Ong, M.L.H.; Schofield, J.B. Assessment of lymph node involvement in colorectal cancer. World J Gastrointest Surg. 2016, 8, 179–192. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.L. Lymph Node Counts and Survival Rates After Resection for Colon and Rectal Cancer. Gastrointest Cancer Res. 2009, 3 (Suppl. 1), S33–S55. [Google Scholar] [PubMed]
- Dimofte, G.; Târcoveanu, E.; Taraşi, M.; Panait, C.; Lozneanu, G.; Nicolescu, S.; Porumb, V.; Grigoraş, O. Mean number of lymph nodes in colonic cancer specimen: possible quality control index for surgical performance. Chirurgia (Bucur). 2011, 106, 759–764. [Google Scholar] [PubMed]
- Kotake, K.; Honjo, S.; Sugihara, K.; Hashiguchi, Y.; Kato, T.; Kodaira, S.; Muto, T.; Koyama, Y. Number of lymph nodes retrieved is an important determinant of survival of patients with stage II and stage III colorectal cancer. Jpn J Clin Oncol. 2012, 42, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Stracci, F.; Bianconi, F.; Leite, S.; Liso, A.; La Rosa, F.; Lancellotta, V.; van de Velde, C.J.; Aristei, C. Linking surgical specimen and examined lymph nodes in colorectal patients. Eur J Surg Oncol. 2016, 42, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Lavy, R.; Hershkovitz, Y.; Muhamad, A.; Sandbank, J.; Halevy, A. Re-examining Distal Resections in Colon Cancer. Isr Med Assoc J. 2017, 19, 696–699. [Google Scholar] [PubMed]
- Hardt, J.; Buhr, H.J.; Klinger, C.; Benz, S.; Ludwig, K.; Kalff, J.; Post, S. Quality indicators for colon cancer surgery: Evidence-based development of a set of indicators for the outcome quality. Chirurg. 2018, 89, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Betge, J.; Harbaum, L.; Pollheimer, M.J.; Lindtner, R.A.; Kornprat, P.; Ebert, M.P.; Langner, C. Lymph node retrieval in colorectal cancer: determining factors and prognostic significance. Int J Colorectal Dis. 2017, 32, 991–998. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.R.; Renehan, A.G.; O’Dwyer, S.T.; Haboubi, N.Y. Lymph node harvest in colon and rectal cancer: Current Considerations. World J Gastrointest Surg. 2012, 4, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Cisz, K.C.; Moreira, A.Z.; Fialho, L.O.; Aguero, H.J.V.; Paiva, D.D.; Oliveira, A.V.; Paulo, F.L. Lymph nodes identification after colorectal cancer resections. Arq Bras Cir Dig. 2011, 24, 103–106. [Google Scholar] [CrossRef]
- Dedavid e Silva, T.L.; Damin, D.C. Lymph node ratio predicts tumor recurrence in stage III colon cancer. Rev Col Bras Cir. 2013, 40, 463–470. [Google Scholar] [PubMed]
- Heald, R.J. The ‘Holy Plane’ of rectal surgery. J R Soc Med. 1988, 81, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Heald, R.J.; Moran, B.J.; Ryall, R.D.; Sexton, R.; MacFarlane, J.K. Rectal Cancer. The basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998, 133, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Hohenberger, W.; Weber, K.; Matzel, K.; Papadopoulos, T.; Merkel, S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation – tehnical notes and outcome. Colorectal Dis. 2009, 11, 354–364. [Google Scholar] [CrossRef] [PubMed]
- West, N.P.; Hohenberger, W.; Weber, K.; Perrakis, A.; Finan, P.J.; Quirke, P. Complete Mesocolic Excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol. 2010, 28, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wang, J.; Lin, L.; Li, J.; Chen, G.; Wang, K.; Zhao, X.; Guocong, W.; Zhang, Z. Surgical and pathological outcomes of complete mesocolic excision compared with conventional surgery in right colon cancers. Int J Clin Exp Med. 2017, 10, 11616–11625. [Google Scholar]
- West, N.P.; Kobayashi, H.; Takahashi, K.; Perrakis, A.; Weber, K.; Hohenberger, W.; Sugihara, K.; Quirke, P. Understanding optimal colon cancer surgery: comparison of japanese D3 resection and european complete mesocolic excision with central vascular ligation. J Clin Oncol. 2012, 30, 1763–1769. [Google Scholar] [CrossRef] [PubMed]
- Sondenaa, K.; Quirke, P.; Hohenberger, W.; Sugihara, K.; Kobayashi, H.; Kessler, H.; Brown, G.; Tudyka, V.; D’Hoore, A.; Kennedy, R.H.; West, N.P.; Kim, S.H.; Heald, R.; Storli, K.E.; Nesbakken, A.; Moran, B. The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery. Int J Colorectal Dis. 2014, 29, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Culligan, K.; Remzi, F.H.; Soop, M.; Coffey, J.C. Review of nomenclature in colonic surgery – proposal of a standardized nomenclature based on mesocolic anatomy. Surgeon. 2013, 11, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.K.; Kim, Y.W.; Han, Y.D.; Cho, M.S.; Hur, H.; Min, B.S.; Lee, K.Y. Complete mesocolic excision and central vascular ligation for colon cancer: principle, anatomy surgical technique and outcomes. Surg Oncol. 2016, 25, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Dimitriou, N.; Griniatsos, J. Complete mesocolic excision: techniques and outcomes. World J Gastrointest Oncol. 2015, 7, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Iancu, C.; Osian, G.; Mocan, L.; Mocan, T.; Zaharie, F.; Todea-Iancu, D.; Bala, O.; Bodea, R.; Al-Hajjar, N.; Pop, F.; Puia, I.C.; Graur, F.; Muteanu, D.; Vlad, L. Management of colorectal resections for treatment of neoplastic intestinal occlusions. Experience of surgery clinic No III, Cluj-Napoca. Chirurgia (Bucur). 2008, 103, 45–51. [Google Scholar] [PubMed]
- Păunică, M.; Pitulice, I.C.; Ștefănescu, A. International migration from public health systems. Case of Romania. Amfiteatru Economic. 2017, 19, 742–756. [Google Scholar]
- Aslan, D.; Bordea, A.; Burcoș, T. Anastomotic leakage after sphincter-sparing surgery in a young woman diagnosed with low rectal cancer – case report. J Clin Invest Surg. 2017, 2, 45–53. [Google Scholar] [CrossRef]


 |
 |
 |
 |
© 2018 by the author. 2018 Stefan Morarasu, Tudor Frunza, Karina Bilavschi, Ana Maria Patrascu, Sorinel Lunca, Gabriel Dimofte
Share and Cite
Morarasu, S.; Frunza, T.; Bilavschi, K.; Patrascu, A.M.; Lunca, S.; Dimofte, G. Histopathology Report on Colon Cancer Specimens—Measuring Surgical Quality, an Increasing Stress for Surgeons. J. Mind Med. Sci. 2018, 5, 75-81. https://doi.org/10.22543/7674.51.P7581
Morarasu S, Frunza T, Bilavschi K, Patrascu AM, Lunca S, Dimofte G. Histopathology Report on Colon Cancer Specimens—Measuring Surgical Quality, an Increasing Stress for Surgeons. Journal of Mind and Medical Sciences. 2018; 5(1):75-81. https://doi.org/10.22543/7674.51.P7581
Chicago/Turabian StyleMorarasu, Stefan, Tudor Frunza, Karina Bilavschi, Ana Maria Patrascu, Sorinel Lunca, and Gabriel Dimofte. 2018. "Histopathology Report on Colon Cancer Specimens—Measuring Surgical Quality, an Increasing Stress for Surgeons" Journal of Mind and Medical Sciences 5, no. 1: 75-81. https://doi.org/10.22543/7674.51.P7581
APA StyleMorarasu, S., Frunza, T., Bilavschi, K., Patrascu, A. M., Lunca, S., & Dimofte, G. (2018). Histopathology Report on Colon Cancer Specimens—Measuring Surgical Quality, an Increasing Stress for Surgeons. Journal of Mind and Medical Sciences, 5(1), 75-81. https://doi.org/10.22543/7674.51.P7581



