Abstract
The therapeutic management decision-making process for breast cancer is complex, and is influenced by multiple factors including patient age, comorbidities, ethnicity, education, and availability of immediate or delayed reconstruction options. Our study analysed 276 patients diagnosed with breast cancer in the “Colțea” Clinical Hospital between 2014 and 2015. Mean patients age was 61.24, median 62, with a range of 31 to 89 years. Younger age was associated with a less advanced local disease and younger patients were more likely to choose and benefit from conservative surgery. Most patients (61.76%) came from rural areas. Place of origin had a significant influence on the tumor size at the time of diagnosis (3.9 cm vs. 1.8 cm) as well as on the choice of surgical procedure. Personalized treatment management plans that include aesthetic satisfaction coupled with oncological safety should be the objectives of contemporary breast surgery. Patient age is so important to the decision making process that it has been proposed as a determinant of educational and counselling strategies. From our experience, young patients from urban areas were more proactive patients. They were diagnosed earlier and more involved in treatment decisions compared with patients from rural areas, who generally did not question the surgeon’s opinion. Factors that influence the decision-making process likely include age, socioeconomic status, availability of radiotherapy, the necessity of periodic follow-up and the concern about recurrence.
Introduction
Breast cancer is the most frequent cancer in women and a common cause of death in women diagnosed with cancer, with over 500,000 deaths annually [1]. Chemoprophylaxis of atypical proliferative lesions may prevent cancer development for select cases and early detection and multimodality treatment improve survival and increase quality of life [2].
Breast cancer diagnosis, represented by the period between breast biopsy and histopathological result, is described as the most distressing moment for a woman across the entire cancer experience [3]. Anxiety increases over this time period and is quickly replaced by shock and doubt when the doctor communicates the diagnosis. After diagnosis, patients with breast cancer must face decisions about their available treatment options, with each having its own risks and benefits. The decision-making process is complex, and is influenced by multiple factors including patient age, comorbidities, ethnicity, education, and availability of immediate or delayed reconstruction options.
In the past ten years women have changed from the passive patient who accepted whatever treatment the doctor prescribed to an active and informed patient who wants to decide which option is best [4]. Personalized treatment management plans that include aesthetic satisfaction of breast cancer patients coupled with oncological safety should be the objectives of modern breast surgery. The treatment choice depends on patient characteristics and will, but is influenced by the doctor who presents and explains surgical options. In understanding these factors, practitioners can help patients make better informed and suitable decisions.
This study is a retrospective analysis over a 2 year-period of treatment selection by cancer patients in an attempt to reveal factors that influenced the decision.
Materials and methods
Our study analyzed 276 patients diagnosed with breast cancer in the “Colțea” Clinical Hospital between 2014 and 2015. This retrospective analysis used a timeframe sufficiently large to ensure enough patients for adequate statistical power. To generate patient groups we utilized queried databases used for reporting in the DRG system (Diagnosis Related Groups), a classification system based on diagnosis. This system is similar to the international disease classification system (International Classification of Diseases – ICD) in which diagnoses are classified into classes and subclasses. Repeated hospitalizations were queried regarding patient diagnoses, along with procedures performed on these occasions. These tools were useful for tracking and monitoring patients, though with the limitation that patients had to have been admitted to the same medical institution for inclusion.
Breast surgical procedures were divided into two classes: mastectomies and conservative procedures. Conservative surgery included all procedures that partially spared the breast, such as sectorectomy, quadranectomy, or atypical oncoplastic resections. Mastectomies included variations that preserve the skin or the nipple-areolar complex (skin sparing, nipple sparing), but with total excision of the mammary gland.
Patients were excluded if their data was incomplete and not sufficiently specific, or in cases where we could not register the result of the histopathologic examination, history of prior radiation to the breast area, cases of inflammatory breast cancer, local advanced breast cancer, particular histopathological types (lymphoma, sarcoma) which require a different therapeutic approach, multicentric tumors involving 2 or more breast quadrants, or diffuse malignant micro-calcifications and neoadjuvant chemotherapy.
Using the aforementioned exclusion criteria, we selected a group of 102 patients who had been potential candidates for both conservative and radical surgical treatment.
Surgical treatment options consisted of breast conservative surgery (sectorectomy), oncoplastic technique (depending on localization and tumor/breast volume), skin sparring mastectomy, or classical mastectomy. At the time of surgery, immediate breast reconstruction was not possible. Delayed breast reconstruction was proposed along with an explanation of its advantages and disadvantages.
Results
Mean patients age was 61.24, median 62, with the youngest 31 and the oldest 88 years old. Younger age was associated with a less advanced local disease, and younger patients were more likely to benefit from conservative surgery (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 and Figure 6).
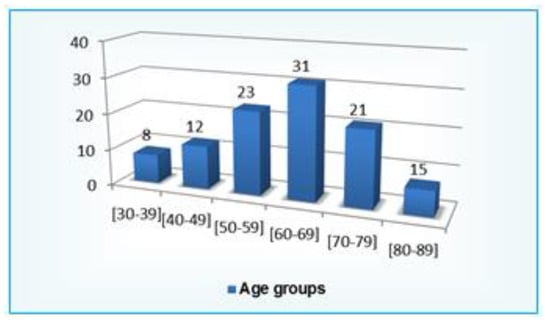
Figure 1.
Age distribution.
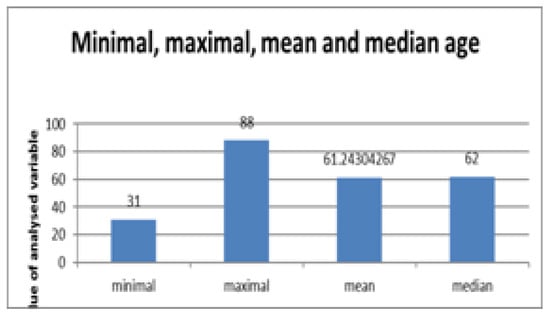
Figure 2.
Minimal, maximal, mean and median age.
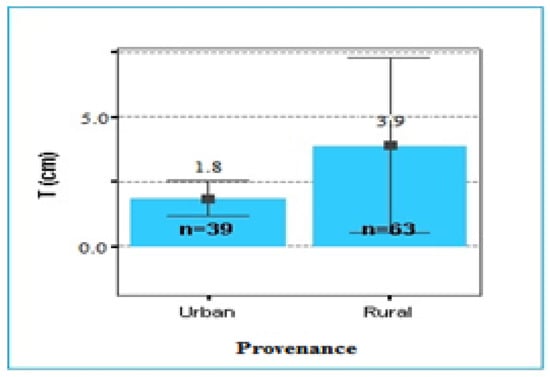
Figure 3.
Provenance.
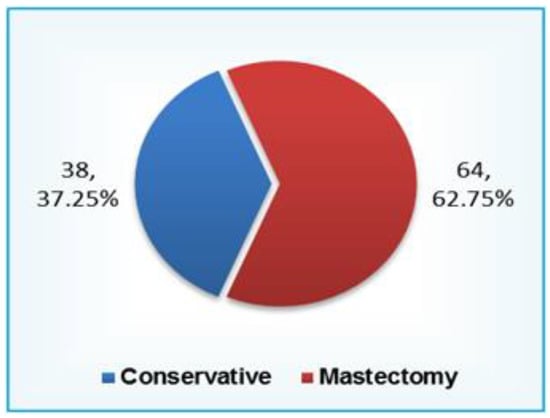
Figure 4.
Type of operations.
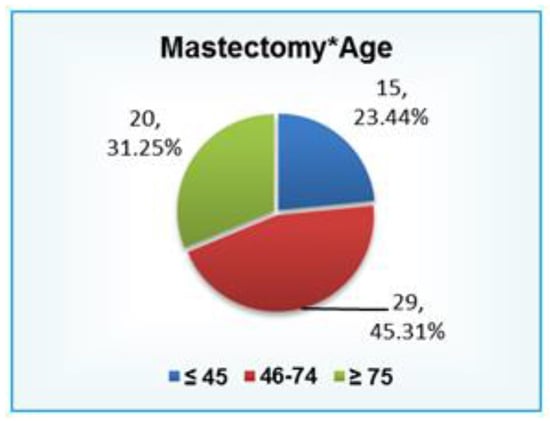
Figure 5.
Mastectomy Age.
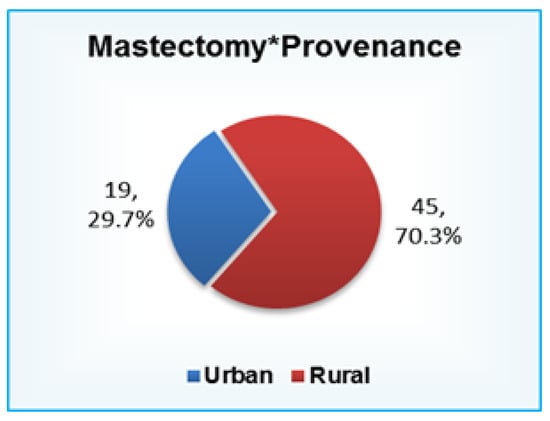
Figure 6.
Mastectomy Provenance.
Most patients (61,76%) came from rural areas. Place of origin had a significant influence on tumor size at the time of the diagnosis (3.9 cm vs. 1.8cm) and on the choice of surgical procedure.
A high percentage of women who underwent breast conservative surgery in our clinic were from urban areas.
Discussion
After the initial shock of a breast cancer diagnosis, women begin to turn their attention to treatment options. They typically seek information about the best physician and treatment as well as their reconstruction options. Personalized treatment management plans that include aesthetic satisfaction coupled with oncological safety should be the objectives of modern breast surgery [5].
Patient age is so important in the decision making process that it has been proposed as a primary determinant of educational and counseling strategies [3,5]. Depending on their age, women react differently when diagnosed with breast cancer, choosing also a distinct type of treatment. Young women under 30 may be considering a family and children, and how a cancer diagnosis might affect this future prospect. Women in the 30’s usually already have a family and are concerned about their future with their children and how their husband will support them. Women in their 40’s have greater family responsibilities, and a cancer diagnosis can upset the balance, considering that their appearance may affect their relationship with their husband and children. Women older than 50 might have had a similar experience with a relative or friend and are often more adapted. They are typically concerned about losing their independence and being obliged to ask for help.
Usually young women take an active role in understanding their condition, seeking information and becoming involved in treatment decisions, compared with older women who rely heavily on the surgeon’s recommendation [6]. Women that assume a more active role in their treatment suffer less from depression and are more satisfied with treatment outcome [7].
In the shared decision making model, the doctor informs the patient about the therapy modalities and incorporates the patient’s needs and desire into the treatment decision. This model is considered best when treatment decisions involve multiple options [8], especially in the management of primary breast cancer where several different surgical options may result in the same oncologic outcome.
From our experience, young patients from urban areas were the most active patients. Not only were they diagnosed earlier in the disease progression, but they were more involved in their treatment decision than patients from rural areas, who were more apt to accept the surgeon’s opinion without further questions.
Breast cancer treatment varies from breast conservation to oncoplastic surgery and mastectomy, radiotherapy of different regimens, chemotherapy, biological and hormonal therapy, depending on the immunohistochemical profile.
Socio-economic status might influence women’s decision-making, probably the result of greater information access, greater need for an aesthetically pleasing result, and greater access to medical services and expensive reconstruction procedures for those have greater resources [9].
The availability of a radiotherapy facility and a high density of radiotherapists have been shown to influence treatment decisions for choosing breast conserving surgery over mastectomy [10,11]. However, this was not an influencing factor in sample as a radiotherapy unit was available to our patients.
The risk of recurrence—related to tumor size, lymph node involvement, and stage—is an important factor influencing treatment decisions. Women are offered breast conserving surgery when faced with small tumor size and no detectable lymph nodes involvement [12].
Conclusions
Regarding surgical management, the most difficult decision a woman faces is breast conserving surgery vs. mastectomy. Conservative techniques, especially those that preserve the nipple areola complex, are followed by improved patient’s perception of the body image, confidence, and sexuality, with the only drawback being increased anxiety linked to recurrence risk [5].
Even though studies have shown that, when feasible, breast conserving surgery associated with radiotherapy has a similar overall survival rate as mastectomy, numerous women choose mastectomy. Factors that influence this decision are likely age, socioeconomic status, the availability of radiotherapy, the necessity of periodic follow-up, and the concern about recurrence.
References
- Ghoncheh, M.; Pournamdar, Z.; Salehiniya, H. Incidence and Mortality and Epidemiology of Breast Cancer in the World. Asian Pac J Cancer Prev. 2016, 17, 43–6. [Google Scholar] [CrossRef] [PubMed]
- Bălălău C, Voiculescu Ș, Motofei I, Scăunașu RV, Negrei C. Low dose tamoxifen as treatment of benign breast proliferative lesions. Farmacia. 2015, 63, 371–75.
- Waring, A.N. Breast Cancer: Reactions, Choices, Decisions. The Ochsner Journal. 2000, 2, 40–6. [Google Scholar] [PubMed]
- Sio, T.T.; Chang, K.; Jayakrishnan, R.; Wu, D.; Politi, M.; Malacarne, D.; Saletnik, J.; Chung, M. Patient age is related to decision-making, treatment selection, and perceived quality of life in breast cancer survivors. World J Surg Oncol. 2014, 12, 230. [Google Scholar] [CrossRef] [PubMed]
- Scaunasu RV, Burcoș T, Voiculescu Ș, Popescu BA, Bertesteanu ȘV, Bălălău OD, Bacalbasa N, Bălălău C. Conservative surgery of breast cancer in women; psychological benefits. J Mind Med Sci. 2016, 3, 13–18. [CrossRef]
- Bleicher, R.J.; Abrahamse, P.; Hawley, S.T.; Katz, S.J.; Morrow, M. The influence of age on the breast surgery decision-making process. Ann Surg Oncol. 2008, 15, 854–62. [Google Scholar] [CrossRef] [PubMed]
- Vogel, B.A.; Leonhart, R.; Helmes, A.W. Communication matters: the impact of communication and participation in decision making on breast cancer patients' depression and quality of life. Patient Educ Couns. 2009, 77, 391–7. [Google Scholar] [CrossRef] [PubMed]
- Pope, T.M.; Hexum, M. Legal briefing: Shared decision making and patient decision aids. J Clin Ethics. 2013, 24, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Moagar-Poladian, S.; Folea, V.; Paunica, M. Competitiveness of EU member states in attracting EU funding for research and innovation. Romanian Journal of Economic Forecasting. 2017, 20, 150–167. [Google Scholar]
- Nattinger, A.B.; Kneusel, R.T.; Hoffmann, R.G.; Gilligan, M.A. Relationship of distance from a radiotherapy facility and initial breast cancer treatment. J Natl Cancer Inst. 2001, 93, 1344–6. [Google Scholar] [CrossRef] [PubMed]
- Voti, L.; Richardson, L.C.; Reis, I.M.; Fleming, L.E.; Mackinnon, J.; Coebergh, J.W. Treatment of local breast carcinoma in Florida: the role of the distance to radiation therapy facilities. Cancer. 2006, 106, 201–7. [Google Scholar] [CrossRef] [PubMed]
- Chagpar AB, Studts JL, Scoggins CR, Martin RC 2nd, Carlson DJ, Laidley AL, El-Eid SE, McGlothin TQ, Noyes RD, McMasters KM. Factors associated with surgical options for breast carcinoma. Cancer. 2006, 106, 1462–6. [CrossRef] [PubMed]
© 2017 by the author. 2017 Răzvan V. Scăunaşu, Ștefan Voiculescu, Bogdan Popescu, Cristina Cozma, Radu Jecan, Cristian Bălălău.