Retrospective Evaluation of Nasopalatine Canal Anatomy, Dimensions, and Variations with Alveolar Bone in Patients Scheduled for Maxillary Anterior Dental Implant Surgery Using Cone Beam Computed Tomography
Abstract
1. Introduction
2. Methods
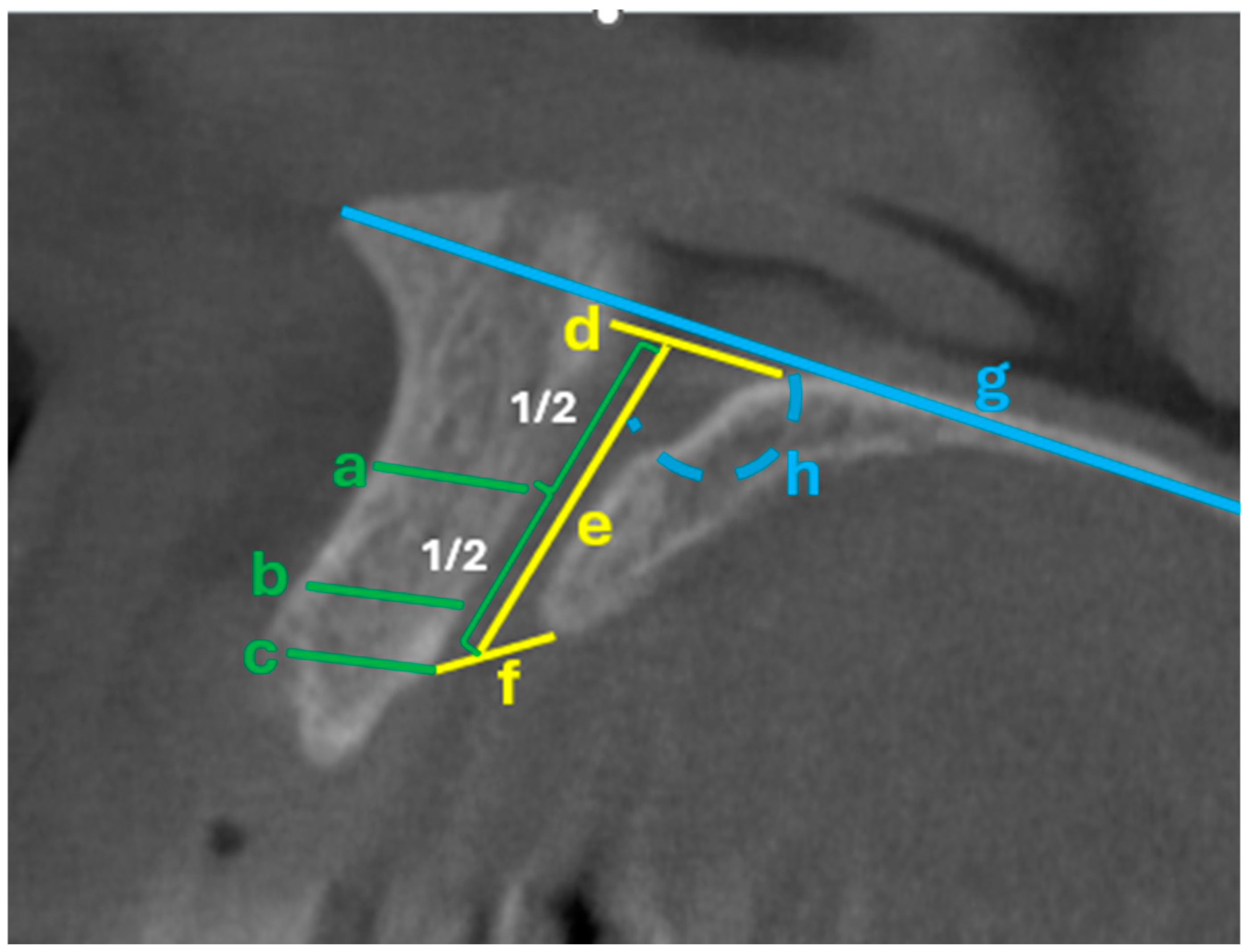
Operational Metrics for Pre-Operative Risk Appraisal
3. Statistical Analysis
4. Results
5. Discussion
Clinical Implications for Guided Surgery and Pre-Operative Assessment
- Screen morphology and multiplicity: Note cylindrical versus conical forms and the presence of accessory canals. In our cohort, the location of the accessory canal differed by sex (p = 0.040); therefore, clinicians should inspect nearer the midline in males and more laterally in females.
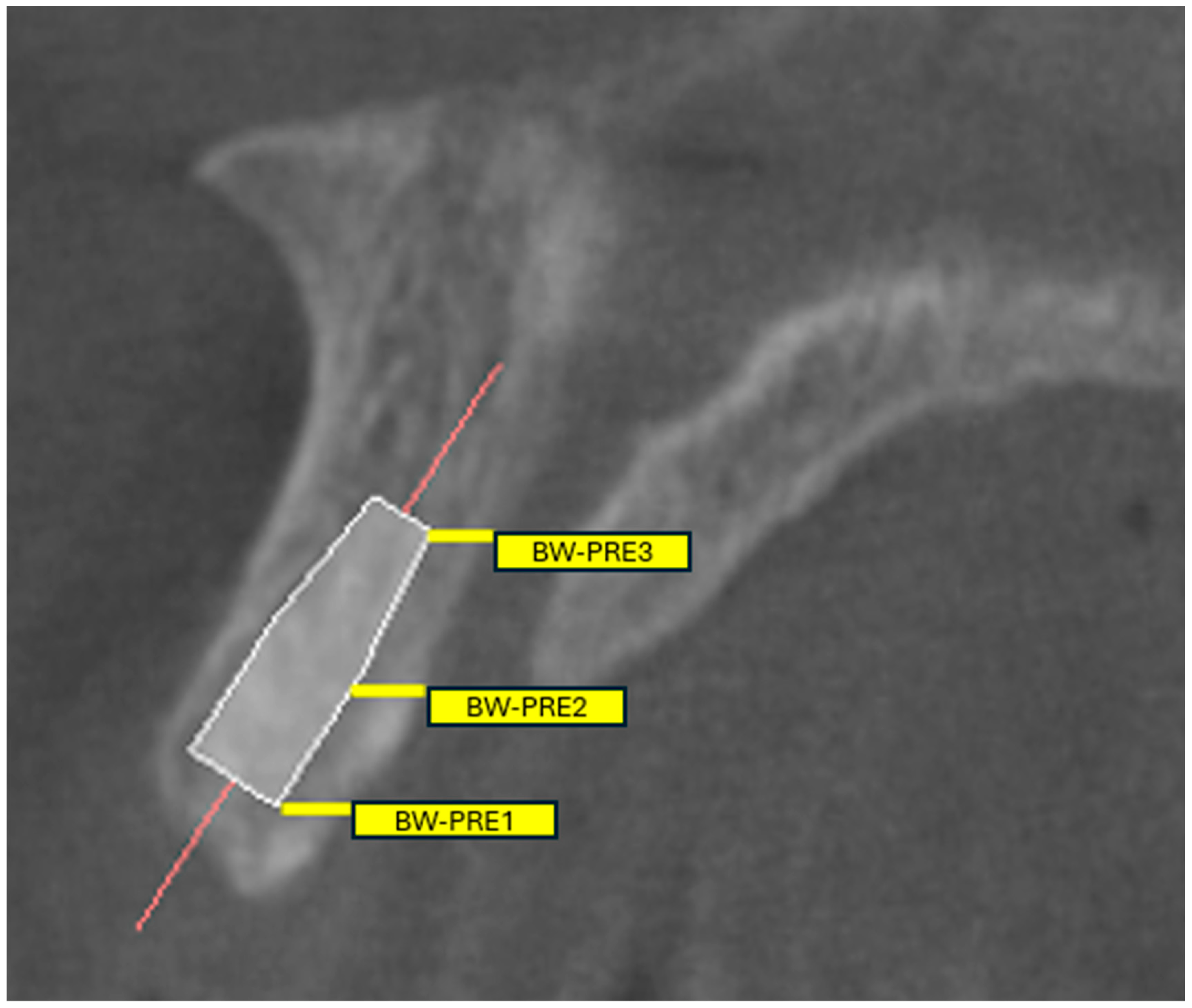
- Quantify proximity: Report Bw-pre 1/2/3 values and flag the lowest quartile—or a validated conservative threshold—as indicating heightened-risk proximity. Previous morphometric studies have demonstrated that the mean bone width between the central incisor root and the NPC ranges from approximately 1.4 mm at the coronal third to 3.2 mm at the apical third [9,10]. Accordingly, the risk of NPC perforation becomes clinically significant when the distance between the canal and the planned implant trajectory is less than 2 mm.
- Verify buccal bone corridor: If mid-level buccal thickness is low, anticipate the need for angulation adjustment, narrower or shorter implants, or minor site development.
- Assess canal trajectory (Angle 1): Markedly oblique canals reduce the safe implant window; consider a more palatal entry point or a custom sleeve offset to prevent encroachment.
- Translate to guide design: Overlay the main and accessory canals, enforce a minimum clearance of ≥2 mm, and lock sleeves to maintain the planned prosthetically driven corridor.
- Plan alternatives: Predefine backup implant diameter, length, and angulation options—or staged augmentation protocols—when canal proximity is high.
- Inform consent and monitor: Document the elevated risk when below the safety threshold and monitor for early signs of nasopalatine bundle irritation, such as paresthesia or intraoperative bleeding.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- White, S.C.; Pharoah, M.J. The evolution and application of dental maxillofacial imaging modalities. Dent. Clin. N. Am. 2008, 52, 689–705. [Google Scholar] [CrossRef] [PubMed]
- Haiderali, Z. The role of CBCT in implant dentistry: Uses, benefits and limitations. Br. Dent. J. 2020, 228, 560–561. [Google Scholar] [CrossRef]
- Howerton, W.B., Jr.; Mora, M.A. Advancements in digital imaging: What is new and on the horizon? J. Am. Dent. Assoc. 2008, 139, 20s–24s. [Google Scholar] [CrossRef] [PubMed]
- Scarfe, W.C.; Farman, A.G.; Sukovic, P. Clinical applications of cone-beam computed tomography in dental practice. J. Can. Dent. Assoc. 2006, 72, 75–80. [Google Scholar] [PubMed]
- Rodella, L.F.; Buffoli, B.; Labanca, M.; Rezzani, R. A review of the mandibular and maxillary nerve supplies and their clinical relevance. Arch. Oral. Biol. 2012, 57, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Liang; Lambrichts, X.; Corpas, I.; Politis, L.; Vrielinck, C.; Ma, L.; Jacobs, G.; Jacobs, R. Neurovascular Disturbance Associated with Implant Placement in the Anterior Mandible and its Surgical Implications: Literature Review including Report of a Case. Chin. J. Dent. Res. 2008, 11, 56. [Google Scholar]
- de Oliveira-Santos, C.; Rubira-Bullen, I.R.; Monteiro, S.A.; León, J.E.; Jacobs, R. Neurovascular anatomical variations in the anterior palate observed on CBCT images. Clin. Oral. Implant. Res. 2013, 24, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, M.M.; Balsiger, R.; Sendi, P.; von Arx, T. Morphology of the nasopalatine canal and dental implant surgery: A radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin. Oral. Implants Res. 2011, 22, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Alkanderi, A.; Al Sakka, Y.; Koticha, T.; Li, J.; Masood, F.; Suárez-López Del Amo, F. Incidence of nasopalatine canal perforation in relation to virtual implant placement: A cone beam computed tomography study. Clin. Implant. Dent. Relat. Res. 2020, 22, 77–83. [Google Scholar] [CrossRef] [PubMed]
- López Jornet, P.; Boix, P.; Sanchez Perez, A.; Boracchia, A. Morphological Characterization of the Anterior Palatine Region Using Cone Beam Computed Tomography. Clin. Implant. Dent. Relat. Res. 2015, 17 (Suppl. 2), e459–e464. [Google Scholar] [CrossRef] [PubMed]
- Alhumaidi, A.M.; Okshah, A.; Al Moaleem, M.M.; Alsabi, M.A.A.; Muharraq, I.H.A.; Asiri, A.Y.; Wasli, Y.A.M.; Alhijji, H.H.S.; Namazi, M.A.; Alfaqih, A.I.I.; et al. Sex and Population Variations in Nasopalatine Canal Dimensions: A CBCT-Based Systematic Review. Med. Sci. Monit. 2024, 30, e945949. [Google Scholar] [CrossRef] [PubMed]
- Soman, C. Assessment of the Nasopalatine Canal Length and Shape Using Cone-Beam Computed Tomography: A Retrospective Morphometric Study. Diagnostics 2024, 14, 973. [Google Scholar] [CrossRef] [PubMed]
- Couso-Queiruga, E.; Pedrinaci, I.; Avila-Ortiz, G.; Chappuis, V.; Barboza, E.P.; Petersen, R.L.; Raabe, C.; Rodrigues, D.M. Characterization of the anterior maxillary region for immediate implant placement: A radiographic cross-sectional study. J. Prosthet. Dent. 2025, in press. [Google Scholar] [CrossRef]
- Mardinger, O.; Namani-Sadan, N.; Chaushu, G.; Schwartz-Arad, D. Morphologic changes of the nasopalatine canal related to dental implantation: A radiologic study in different degrees of absorbed maxillae. J. Periodontol. 2008, 79, 1659–1662. [Google Scholar] [CrossRef] [PubMed]
- Güncü, G.N.; Yıldırım, Y.D.; Yılmaz, H.G.; Galindo-Moreno, P.; Velasco-Torres, M.; Al-Hezaimi, K.; Al-Shawaf, R.; Karabulut, E.; Wang, H.L.; Tözüm, T.F. Is there a gender difference in anatomic features of incisive canal and maxillary environmental bone? Clin. Oral. Implant. Res. 2013, 24, 1023–1026. [Google Scholar] [CrossRef]
- Öçbe, M.; Medişoğlu, M.S. Multimodal Imaging of the Nasopalatine Canal: Morphometric Characteristics and Signal Intensity Assessment. J. Craniofac. Surg. 2025, 36, 2564–2569. [Google Scholar] [CrossRef]
- Firincioglulari, M.; Orhan, K. Morphological Variations of the Nasopalatine Canal in the North Cyprus Population: A Cone Beam Computed Tomography Study. Med. Sci. Monit. 2024, 30, e944868. [Google Scholar] [CrossRef]
- Etoz, M.; Sisman, Y. Evaluation of the nasopalatine canal and variations with cone-beam computed tomography. Surg. Radiol. Anat. 2014, 36, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Milanovic, P.; Selakovic, D.; Vasiljevic, M.; Jovicic, N.U.; Milovanović, D.; Vasovic, M.; Rosic, G. Morphological Characteristics of the Nasopalatine Canal and the Relationship with the Anterior Maxillary Bone-A Cone Beam Computed Tomography Study. Diagnostics 2021, 11, 915. [Google Scholar] [CrossRef]
| N | % | ||
|---|---|---|---|
| Age | 20–39 age | 62 | 33.5% |
| 40–59 age | 75 | 40.5% | |
| 60–75 age | 48 | 25.9% | |
| Gender | Man | 93 | 50.3% |
| Female | 92 | 49.7% | |
| Number of nasopalatine canal (NPC) | 1 | 162 | 87.6% |
| 2 | 23 | 12.4% | |
| The region where the nasopalatine canal is located | Central incisor region | 101 | 54.6% |
| Between central and lateral | 64 | 34.6% | |
| Lateral incisor region | 18 | 9.7% | |
| Canine region | 2 | 1.1% | |
| Additional foramina observed in the palate according to their location | Between central and lateral | 11 | 47.8% |
| Lateral incisor region | 10 | 43.5% | |
| Canine region | 2 | 8.7% | |
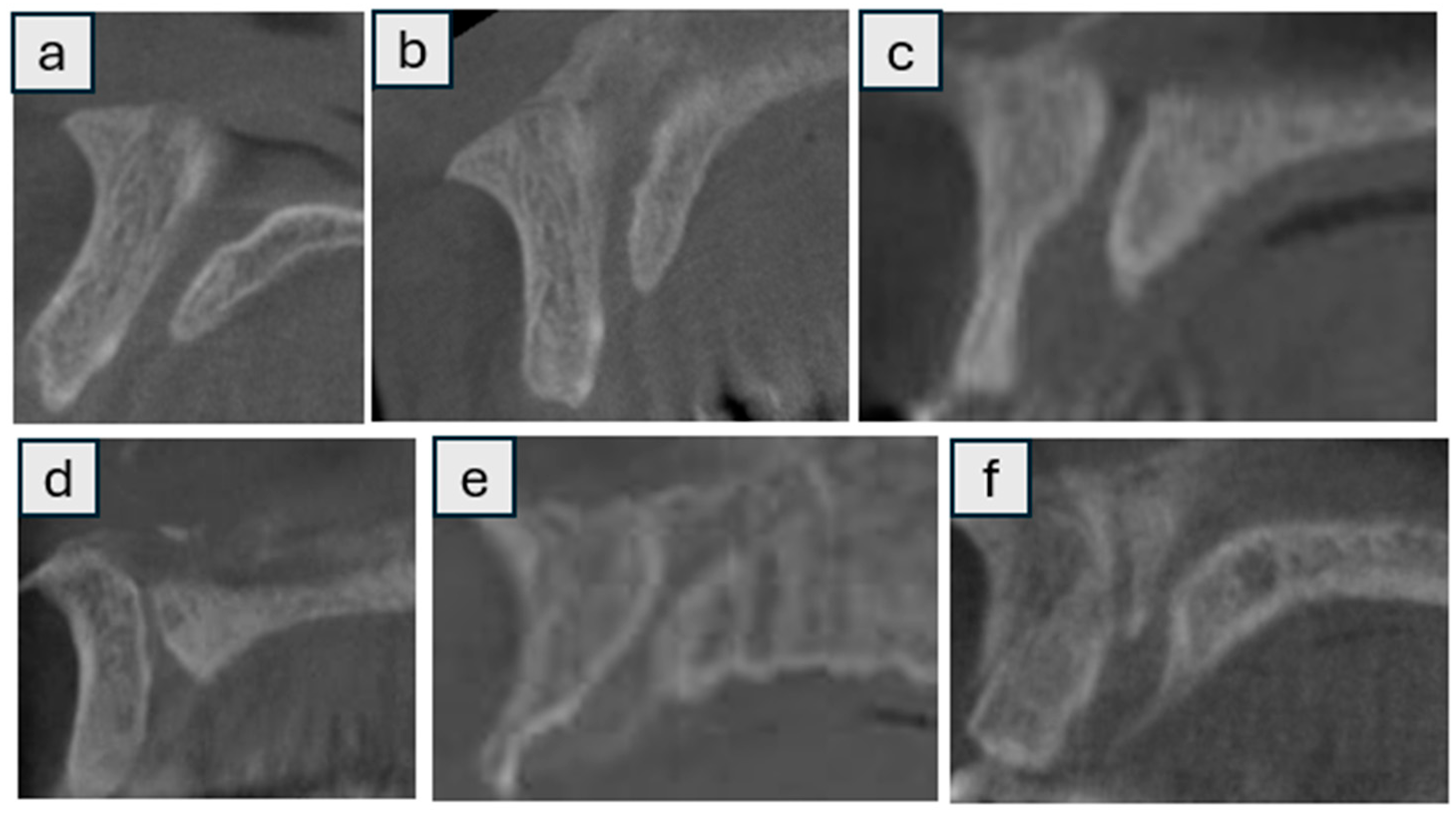
| Morphology of the nasopalatine canal (Sagittal) | Cylindrical | 83 | 44.9% |
| Cone | 47 | 25.4% | |
| Funnel | 41 | 22.1% | |
| Banana-shaped | 3 | 1.6% | |
| Hourglass-shaped | 8 | 4.3% | |
| Tree branch | 3 | 1.6% | |
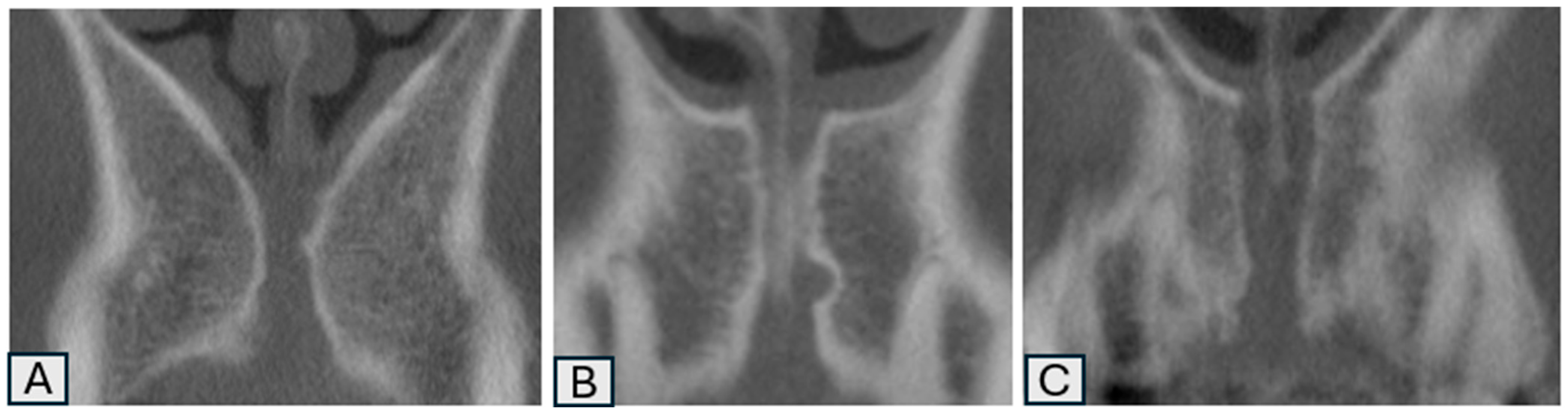
| Morphology of the nasopalatine canal (Coronal) | Single | 97 | 52.4% |
| 2 parallel | 23 | 12.4% | |
| Y-shaped | 65 | 35.1% | |
| Mean | Std. Dev. | ||
|---|---|---|---|
| Age | 47.94 | 13.61 | |
| Canal diameter (mm) | Nasal | 3.15 | 0.66 |
| Palatal | 3.42 | 0.62 | |
| Mean | 3.29 | 0.45 | |
| Canal length (mm) | 11.39 | 1.98 | |
| Buccal anterior to the canal (mm) | Coronal | 9.70 | 1.58 |
| Buccal anterior to the canal (mm) | Middle | 7.10 | 1.04 |
| Buccal anterior to the canal (mm) | Apical | 9.61 | 0.54 |
| Angle 1 (with horizontal plate) | 107.50 | 4.43 | |
| Angle 2 (with palatal bone margin) | 6.35 | 1.81 | |
| Angle 3 (with incisor) | 9.26 | 3.48 | |
| Bw-pre 1 (mm) | 1.66 | 0.45 | |
| Bw-pre 2 (mm) | 2.53 | 0.58 | |
| Bw-pre 3 (mm) | 3.59 | 0.82 |
| Age | ||||||||
|---|---|---|---|---|---|---|---|---|
| 20–39 Age | 40–59 Age | 60–75 Age | ||||||
| Mean | SD | Mean | SD | Mean | SD | * p. | ||
| Canal diameter (mm) | Nasal | 3.26 | 0.61 | 3.02 | 0.68 | 3.22 | 0.66 | 0.071 |
| Palatal | 3.43 | 0.66 | 3.40 | 0.61 | 3.43 | 0.61 | 0.940 | |
| Mean | 3.35 | 0.49 | 3.21 | 0.43 | 3.33 | 0.43 | 0.162 | |
| Canal length (mm) | 11.51 | 2.16 | 11.44 | 1.79 | 11.17 | 2.03 | 0.645 | |
| Buccal anterior to the canal (mm) | Coronal | 9.87 | 1.58 | 9.45 | 1.60 | 9.87 | 1.55 | 0.218 |
| Buccal anterior to the canal (mm) | Middle | 7.14 | 1.05 | 7.09 | 1.02 | 7.08 | 1.10 | 0.942 |
| Buccal anterior to the canal (mm) | Apical | 9.51 | 0.51 | 9.70 | 0.52 | 9.61 | 0.58 | 0.115 |
| Angle 1 (with horizontal plate) | 107.53 | 3.89 | 108.10 | 4.45 | 106.53 | 4.95 | 0.160 | |
| Angle 2 (with palatal bone margin) | 6.22 | 1.88 | 6.43 | 1.73 | 6.38 | 1.87 | 0.795 | |
| Angle 3 (with incisor) | 9.00 | 3.84 | 9.26 | 3.10 | 9.59 | 3.57 | 0.680 | |
| Bw-pre 1 (mm) | 1.71 | 0.47 | 1.65 | 0.45 | 1.59 | 0.44 | 0.391 | |
| Bw-pre 2 (mm) | 2.52 | 0.55 | 2.51 | 0.59 | 2.57 | 0.58 | 0.863 | |
| Bw-pre 3 (mm) | 3.63 | 0.83 | 3.63 | 0.81 | 3.49 | 0.82 | 0.614 | |
| Gender | ||||||
|---|---|---|---|---|---|---|
| Male | Female | |||||
| Mean | SD | Mean | SD | * p. | ||
| Canal diameter (mm) | Nasal | 3.09 | 0.69 | 3.22 | 0.62 | 0.197 |
| Palatal | 3.44 | 0.62 | 3.39 | 0.63 | 0.598 | |
| Mean | 3.27 | 0.43 | 3.31 | 0.47 | 0.566 | |
| Canal length (mm) | 11.41 | 1.99 | 11.38 | 1.97 | 0.943 | |
| Buccal anterior to the canal (mm) | Cornal | 9.78 | 1.61 | 9.62 | 1.57 | 0.496 |
| Buccal anterior to the canal (mm) | Middle | 7.10 | 1.08 | 7.10 | 1.02 | 0.978 |
| Buccal anterior to the canal (mm) | Apical | 9.63 | 0.54 | 9.60 | 0.54 | 0.732 |
| Angle 1 (with horizontal plate) | 108.11 | 4.10 | 106.89 | 4.69 | 0.061 | |
| Angle 2 (with palatal bone margin) | 6.37 | 1.93 | 6.33 | 1.68 | 0.881 | |
| Angle 3 (with incisor) | 9.22 | 3.51 | 9.29 | 3.46 | 0.887 | |
| Bw-pre 1 (mm) | 1.63 | 0.46 | 1.68 | 0.45 | 0.419 | |
| Bw-pre 2 (mm) | 2.48 | 0.57 | 2.58 | 0.58 | 0.262 | |
| Bw-pre 3 (mm) | 3.59 | 0.82 | 3.60 | 0.81 | 0.915 | |
| Variable | Subcategory | 20–39 Age N | 20–39 Age % | 40–59 Age N | 40–59 Age % | 60–75 Age N | 60–75 Age % | p_Value |
|---|---|---|---|---|---|---|---|---|
| Number of nasopalatine canal (NPC) | 1 | 55 | 21.6 | 63 | 20.2 | 44 | 22.4 | 0.429 |
| 2 | 7 | 2.7 | 12 | 3.8 | 4 | 2.0 | ||
| The region where the nasopalatine canal is located | Central incisor region | 37 | 14.5 | 43 | 13.8 | 21 | 10.7 | 0.288 |
| Between central and lateral | 18 | 7.1 | 25 | 8.0 | 21 | 10.7 | ||
| Lateral incisor region | 7 | 2.7 | 5 | 1.6 | 6 | 3.1 | ||
| Canine region | 0 | 0.0 | 2 | 0.6 | 0 | 0.0 | ||
| Additional foramina observed in the palate according to their location. | Between central and lateral | 1 | 0.4 | 6 | 1.9 | 4 | 2.0 | 0.110 |
| Lateral incisor region | 5 | 2.0 | 5 | 1.6 | 0 | 0.0 | ||
| Canine region | 1 | 0.4 | 1 | 0.3 | 0 | 0.0 | ||
| Morphology of the nasopalatine canal (Sagittal) | Cylindrical | 26 | 10.2 | 34 | 10.9 | 23 | 11.7 | 0.632 |
| Cone | 15 | 5.9 | 23 | 7.4 | 9 | 4.6 | ||
| Funnel | 15 | 5.9 | 16 | 5.1 | 10 | 5.1 | ||
| Banana-shaped | 1 | 0.4 | 1 | 0.3 | 1 | 0.5 | ||
| Hourglass-shaped | 4 | 1.6 | 0 | 0.0 | 4 | 2.0 | ||
| Tree branch | 1 | 0.4 | 1 | 0.3 | 1 | 0.5 | ||
| Morphology of the nasopalatine canal (Coronal) | Single | 33 | 12.9 | 36 | 11.5 | 28 | 14.3 | 0.708 |
| 2 parallel | 7 | 2.7 | 12 | 3.8 | 4 | 2.0 | ||
| Y-shaped | 22 | 8.6 | 27 | 8.7 | 16 | 8.2 |
| Variable | Subcategory | Male_N | Female_N | Male_% (Column) | Female_% (Column) | p_Value |
|---|---|---|---|---|---|---|
| Number of nasopalatine canal (NPC) | 1 | 84 | 78 | 90.3 | 84.8 | 0.254 |
| 2 | 9 | 14 | 9.7 | 15.2 | ||
| The region where the nasopalatine canal is located | Central incisor region | 48 | 53 | 51.6 | 57.6 | 0.477 |
| Between central and lateral | 34 | 30 | 36.6 | 32.6 | ||
| Lateral incisor region | 9 | 9 | 9.7 | 9.8 | ||
| Canine region | 2 | 0 | 2.2 | 0.0 | ||
| Additional foramina observed in the palate according to their location | Between central and lateral | 7 | 4 | 77.8 | 28.6 | 0.040 |
| Lateral incisor region | 1 | 9 | 11.1 | 64.3 | ||
| Canine region | 1 | 1 | 11.1 | 7.1 | ||
| Morphology of the nasopalatine canal (Sagittal) | Cylindrical | 45.0 | 38 | 48.4 | 41.3 | 0.299 |
| Cone | 9.0 | 27 | 9.7 | 29.3 | ||
| Funnel | 32.0 | 23 | 34.4 | 25.0 | ||
| Banana | 2.0 | 1 | 2.2 | 1.1 | ||
| Hourglass | 5.0 | 3 | 5.4 | 3.3 | ||
| Tree branch | 3 | 0 | 100 | 0.0 | ||
| Morphology of the nasopalatine canal (Coronal) | Single | 53 | 44 | 57 | 47.8 | 0.358 |
| 2 parallel | 9 | 14 | 9.7 | 15.2 | ||
| Y-shaped | 31 | 34 | 33.3 | 37.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Özarslantürk, S.; Ceylan Şen, S.; Saraç Atagün, Ö. Retrospective Evaluation of Nasopalatine Canal Anatomy, Dimensions, and Variations with Alveolar Bone in Patients Scheduled for Maxillary Anterior Dental Implant Surgery Using Cone Beam Computed Tomography. Tomography 2025, 11, 114. https://doi.org/10.3390/tomography11100114
Özarslantürk S, Ceylan Şen S, Saraç Atagün Ö. Retrospective Evaluation of Nasopalatine Canal Anatomy, Dimensions, and Variations with Alveolar Bone in Patients Scheduled for Maxillary Anterior Dental Implant Surgery Using Cone Beam Computed Tomography. Tomography. 2025; 11(10):114. https://doi.org/10.3390/tomography11100114
Chicago/Turabian StyleÖzarslantürk, Savaş, Seval Ceylan Şen, and Özlem Saraç Atagün. 2025. "Retrospective Evaluation of Nasopalatine Canal Anatomy, Dimensions, and Variations with Alveolar Bone in Patients Scheduled for Maxillary Anterior Dental Implant Surgery Using Cone Beam Computed Tomography" Tomography 11, no. 10: 114. https://doi.org/10.3390/tomography11100114
APA StyleÖzarslantürk, S., Ceylan Şen, S., & Saraç Atagün, Ö. (2025). Retrospective Evaluation of Nasopalatine Canal Anatomy, Dimensions, and Variations with Alveolar Bone in Patients Scheduled for Maxillary Anterior Dental Implant Surgery Using Cone Beam Computed Tomography. Tomography, 11(10), 114. https://doi.org/10.3390/tomography11100114






