Imaging Characteristics of Embedded Tooth-Associated Cemento-Osseous Dysplasia by Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Distribution of Type Based on the WHO Classification and Stages Based on Imaging Features in Patients with COD
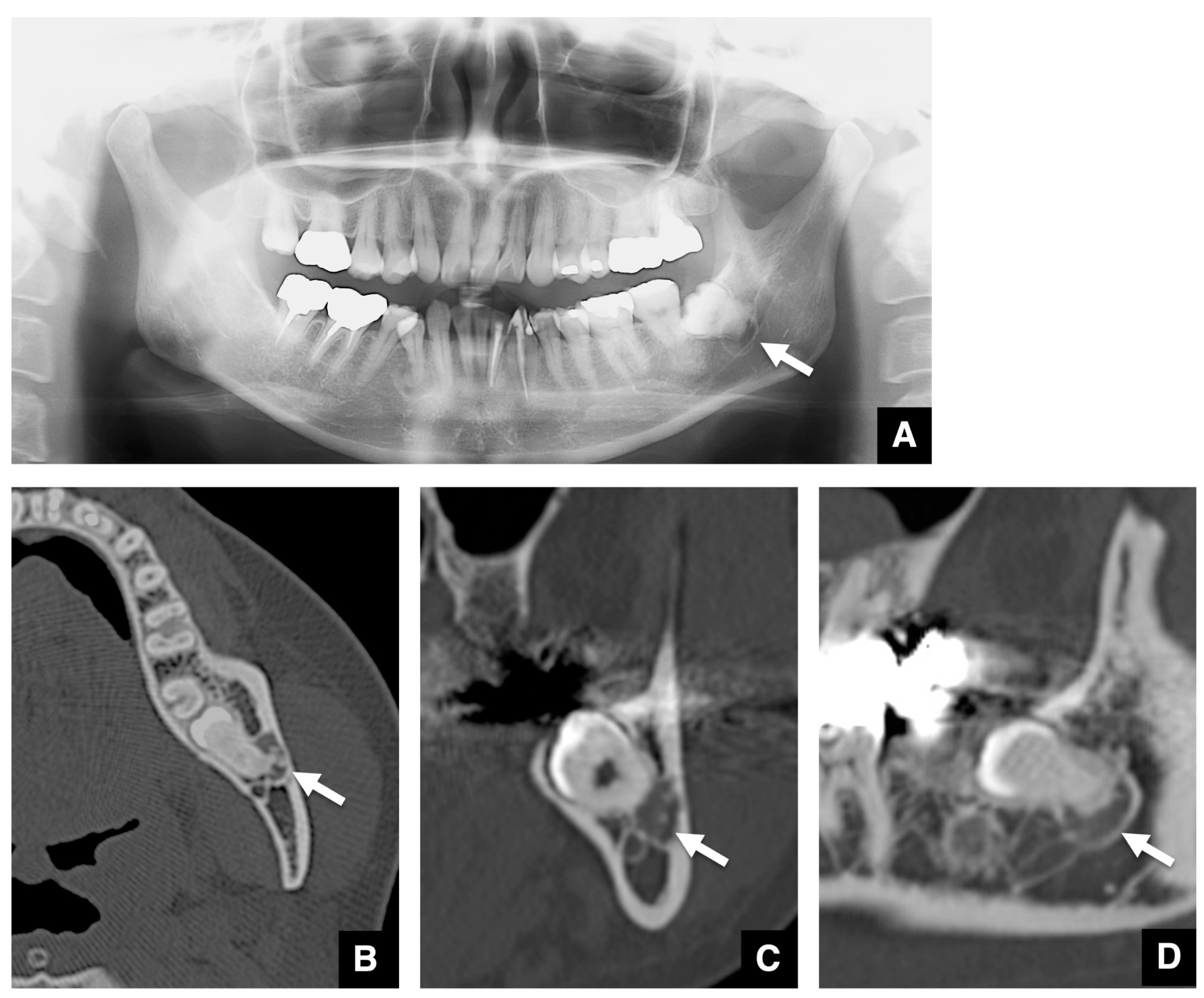
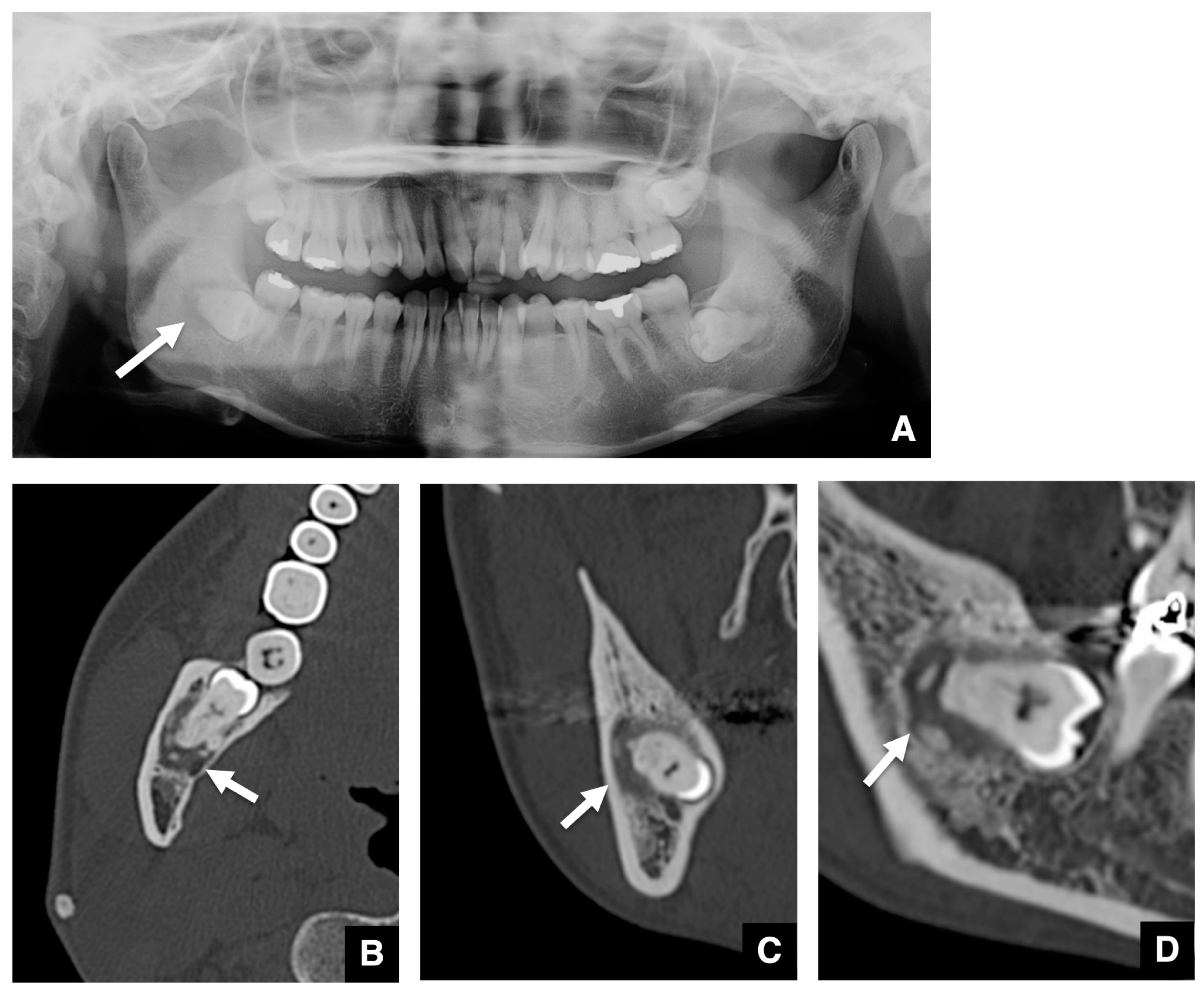
3.2. Imaging Characteristics of COD Associated with Embedded Teeth
4. Discussion
5. Conclusions
6. Clinical Significance
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aiuto, R.; Gucciardino, F.; Rapetti, R.; Siervo, S.; Bianch, A.E. Management of symptomatic florid cemento-osseous dysplasia: Literature review and a case report. J. Clin. Exp. Dent. 2018, 10, e291–e295. [Google Scholar] [CrossRef]
- Nel, C.; Yakoob, Z.; Schouwstra, C.M.; van Heerden, W.F. Familial florid cemento-osseous dysplasia: A report of three cases and review of the literature. Dentomaxillofac. Radiol. 2021, 50, 20190486. [Google Scholar] [CrossRef]
- Kato, C.N.A.O.; de Arruda, J.A.A.; Mendes, P.A.; Neiva, I.M.; Abreu, L.G.; Moreno, A.; Silva, T.A.; Souza, L.N.; Mesquita, R.A. Infected Cemento-Osseous Dysplasia: Analysis of 66 Cases and Literature Review. Head Neck Pathol. 2020, 14, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Langlais, R.P.; Langland, O.E.; Nortje, C.J. Diagnostic Imaging of the Jaws; Williams & Wilkins: Baltimore, MI, USA, 1995; pp. 540–547. [Google Scholar]
- El-Naggar, A.K.; Chan, J.K.C.; Grandis, J.R.; Takata, T.; Slootweg, P.J. World Health Organization Classification of Head and Neck Tumours; International Agency for Research on Cancer IARC Press: Lyon, France, 2017; pp. 254–255. [Google Scholar]
- Cavalcanti, P.H.P.; Nascimento, E.H.L.; Pontual, M.L.D.A.; Pontual, A.D.A.; Marcelos, P.G.C.L.; Perez, D.E.D.C.; Ramos-Perez, F.M.M. Cemento-Osseous Dysplasias: Imaging Features Based on Cone Beam Computed Tomography Scans. Braz. Dent. J. 2018, 29, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Brody, A.; Zalatnal, A.; Csomo, K.; Belik, A.; Dobo-Nagy, C. Difficulties in the diagnosis of periapical translucencies and in the classification of cemento-osseous dysplasia. BMC Oral. Health 2019, 19, 139. [Google Scholar] [CrossRef] [PubMed]
- White, S.C.; Pharoah, M.J. Other Bone Diseases. In Oral Radiology: Principles and Interpretation, 7th ed.; White, S.C., Pharoah, M.J., Eds.; Mosby Elsevier: St. Louis, MA, USA, 2013; pp. 408–413. [Google Scholar]
- Lima, L.B.; de Freitas Filho, S.A.; Barbosa de Paulo, L.F.; Servato, J.P.; Rosa, R.R.; Faria, P.R.; Loyola, A.M.; Cardoso, S.V. Simple bone cyst: Description of 60 cases seen at a Brazilian School of Dentistry and review of international literature. Med. Oral. Patol. Oral. Cir. Bucal. 2020, 25, e616–e625. [Google Scholar] [CrossRef] [PubMed]
- Gumru, B.; Akkitap, M.P.; Deveci, S.; Idman, E. A retrospective cone beam computed tomography analysis of cemento-osseous dysplasia. J. Dent. Sci. 2021, 16, 1154–1161. [Google Scholar] [CrossRef] [PubMed]
- Benaessa, M.M.; Mahomed, F.; Ngwenya, S.P. A retrospective clinico-pathologic analysis of cemento-osseous dysplasia in a South African patient population. Afr. Health Sci. 2019, 19, 3154–3159. [Google Scholar] [CrossRef] [PubMed]
- Barnts, K.; Feng, J.Q.; Qin, C.; Zhang, H.; Cheng, Y.L. Adenomatoid odontogenic tumor: Evidence for a mixed odontogenic tumor. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2022, 133, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Pawar, S.R.; Kshirsagar, R.A.; Purkayastha, R.S.; Joshi, S. Adenomatoid Odontogenic Tumor Mimicking a Dentigerous Cyst in Maxilla. Int. J. Clin. Pediatr. Dent. 2022, 15, 770–773. [Google Scholar] [PubMed]
- Só, B.B.; Carrard, V.C.; Hildebrand, L.C.; Martins, M.A.T.; Martins, M.D. Synchronous Calcifying Epithelial Odontogenic Tumor: Case Report and Analysis of the 5 Cases in the Literature. Head Neck Pathol. 2020, 14, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Yeh, T.H.; Chen, Y.C.; Lee, Y.P.; Chiang, C.P. Calcifying odontogenic cyst treated by marsupialization and subsequent total enucleation. J. Dent. Sci. 2022, 17, 1076–1078. [Google Scholar] [CrossRef] [PubMed]
- Alsufyani, N.A.; Lam, E.W. Osseous (cement-osseous) dysplasia of the jaws: Clinical and radiographic analysis. J. Can. Dent. Assoc. 2011, 77, b70. [Google Scholar] [PubMed]
- Toledano-Serrabone, J.; Nunez-Urrutia, S.; Vegas-Bustamante, E.; Sanchez-Torres, A.; Gay-Escoda, C. Florid cemento-osseous dysplasia: Repot of 2 cases. J. Clin. Exp. Dent. 2018, 10, e1145–e1148. [Google Scholar] [CrossRef] [PubMed]

| WHO Classification | Number of Patients | Number of Lesions Including the Mandibular Third Molar | Rate (%) |
|---|---|---|---|
| Periapical | 23 | - | - |
| Focal | 137 | 12 | 8.8 |
| Florid | 65 | 1 | 1.5 |
| Total | 225 | 13 | 5.8 |
| On Panoramic Tomography | On CT Imaging | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (y) | Sex | Side | WHO Classification | Stage | Shape | Size (mm) | Impaction of Associated Mandibular Third Molar | Margin | Sclerotic Rim | Internal Properties | Margin | Sclerotic Rim | Internal Properties | Contiguous between Root and Internal Properties | Thinning of Adjacent Cortical Bone | Expansion of Cortical Bone | Resorption of Mandibular Canal |
| 48 | F | Left | Focal | Second | Round | 7.0 × 4.3 × 7.1 | Horizontal | Well-defined | Thin | Undetectable | Smooth | Present | Radiopaque dots | Distinct | Present | Present | Absent |
| 33 | F | Right | Focal | Second | Round | 8.6 × 7.0 × 7.2 | Horizontal | Well-defined | Thick | Crescent | Not smooth | Present | Uniform calcification | Distinct | Present | Absent | Absent |
| Left | Focal | Second | Round | 7.9 × 7.3 × 7.1 | Horizontal | Well-defined | Undetectable | Undetectable | Smooth | Present | Radiopaque dots | Partial contact | Present | Absent | Present | ||
| 35 | F | Right | Focal | First | Round | 9.1 × 8.6 × 10.4 | Horizontal | Ill-defined | Thin | Undetectable | Smooth | Absent | Undetectable | Distinct | Present | Absent | Present |
| 39 | F | Right | Focal | Second | Round | 14.8 × 8.5 × 9.9 | Horizontal | Well-defined | Undetectable | Crescent | Smooth | Present | Uniform calcification | Distinct | Absent | Absent | Present |
| 47 | F | Right | Focal | Second | Irregular | 8.4 × 6.0 × 9.7 | Vertical | Well-defined | Undetectable | Pearls | Not smooth | Absent | Massive calcification | Partial contact | Present | Absent | Present |
| 42 | F | Left | Focal | Second | Irregular | 10.2 × 5.6 × 13.0 | Horizontal | Well-defined | Undetectable | Multiple dots | Smooth | Present | Radiopaque dots | Distinct | Present | Absent | Present |
| 51 | F | Right | Focal | Second | Round | 9.8 × 6.2 × 5.8 | Horizontal | Ill-defined | Undetectable | Crescent | Smooth | Present | Uniform calcification | Partial contact | Absent | Absent | Present |
| 33 | F | Left | Focal | Second | Round | 10.3 × 8.7 × 11.5 | Vertical | Ill-defined | Undetectable | Multiple dots | Smooth | Present | Massive calcification | Contiguous | Present | Absent | Present |
| 62 | M | Right | Focal | First | Round | 6.0 × 2.9 × 5.7 | Horizontal | Well-defined | Undetectable | Undetectable | Smooth | Present | Undetectable | Distinct | Absent | Absent | Absent |
| 44 | M | Left | Focal | First | Round | 8.7 × 5.7 × 5.8 | Horizontal | Ill-defined | Undetectable | Undetectable | Smooth | Absent | Undetectable | Distinct | Absent | Absent | Absent |
| 45 | F | Right | Florid | Second | Round | 11.9 × 8.6 × 11.7 | Horizontal | Ill-defined | Undetectable | Undetectable | Smooth | Present | Multiple radiopaque dots | Partially contact | Absent | Absent | Present |
| Left | Florid | Second | Round | 10.2 × 5.6 × 11.9 | Horizontal | Ill-defined | Thin | Multiple dots | Not smooth | Present | Multiple radiopaque dots | Partially contact | Present | Absent | Present | ||
| 38 | F | Left | Focal | Final | Round | 13.2 × 9.8 × 10.2 | Horizontal | Well-defined | Thick | Pearls | Not smooth | Absent | Uniform calcification | Contiguous | Present | Absent | Absent |
| 35 | F | Left | Focal | Second | Round | 11.7 × 7.1 × 10.0 | Horizontal | Well-defined | Thin | Multiple dots | Smooth | Present | Radiopaque dots | Partial contact | Present | Absent | Present |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishimura, S.; Oda, M.; Habu, M.; Takahashi, O.; Tsurushima, H.; Otani, T.; Yoshiga, D.; Wakasugi-Sato, N.; Matsumoto-Takeda, S.; Nishina, S.; et al. Imaging Characteristics of Embedded Tooth-Associated Cemento-Osseous Dysplasia by Retrospective Study. Tomography 2024, 10, 231-242. https://doi.org/10.3390/tomography10020018
Nishimura S, Oda M, Habu M, Takahashi O, Tsurushima H, Otani T, Yoshiga D, Wakasugi-Sato N, Matsumoto-Takeda S, Nishina S, et al. Imaging Characteristics of Embedded Tooth-Associated Cemento-Osseous Dysplasia by Retrospective Study. Tomography. 2024; 10(2):231-242. https://doi.org/10.3390/tomography10020018
Chicago/Turabian StyleNishimura, Shun, Masafumi Oda, Manabu Habu, Osamu Takahashi, Hiroki Tsurushima, Taishi Otani, Daigo Yoshiga, Nao Wakasugi-Sato, Shinobu Matsumoto-Takeda, Susumu Nishina, and et al. 2024. "Imaging Characteristics of Embedded Tooth-Associated Cemento-Osseous Dysplasia by Retrospective Study" Tomography 10, no. 2: 231-242. https://doi.org/10.3390/tomography10020018
APA StyleNishimura, S., Oda, M., Habu, M., Takahashi, O., Tsurushima, H., Otani, T., Yoshiga, D., Wakasugi-Sato, N., Matsumoto-Takeda, S., Nishina, S., Yoshii, S., Sasaguri, M., Yoshioka, I., & Morimoto, Y. (2024). Imaging Characteristics of Embedded Tooth-Associated Cemento-Osseous Dysplasia by Retrospective Study. Tomography, 10(2), 231-242. https://doi.org/10.3390/tomography10020018






