Application of Three-Dimensional Digital Technology in Orthodontics: The State of the Art
Abstract
1. Introduction
2. Diagnosis
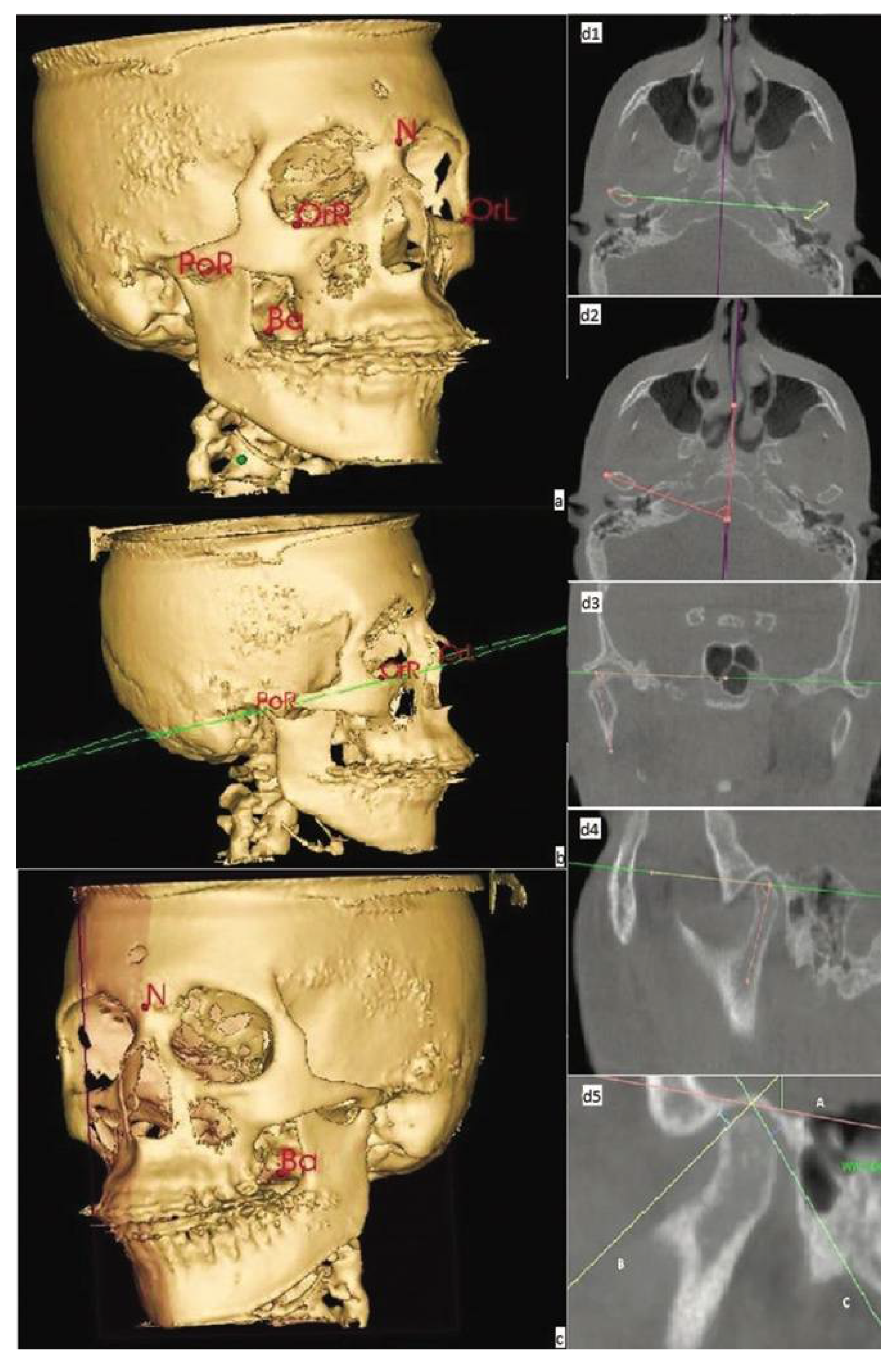
2.1. 3D Cephalometry
2.1.1. CBCT Assessment
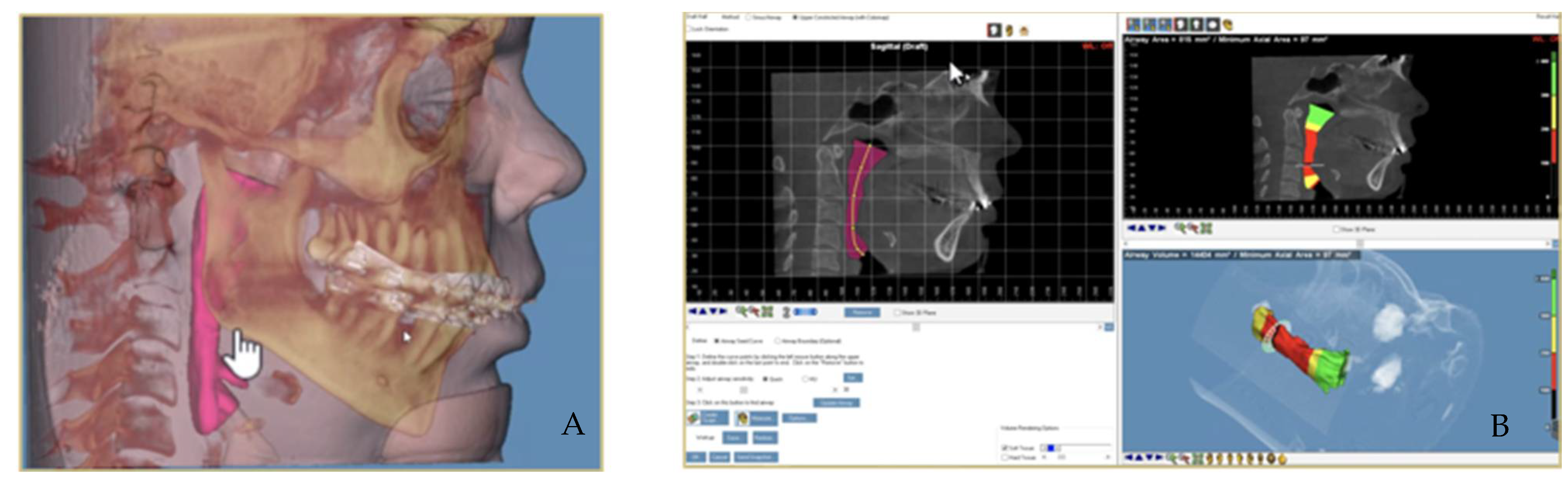
2.1.2. Airways Measuring Method with CBCT
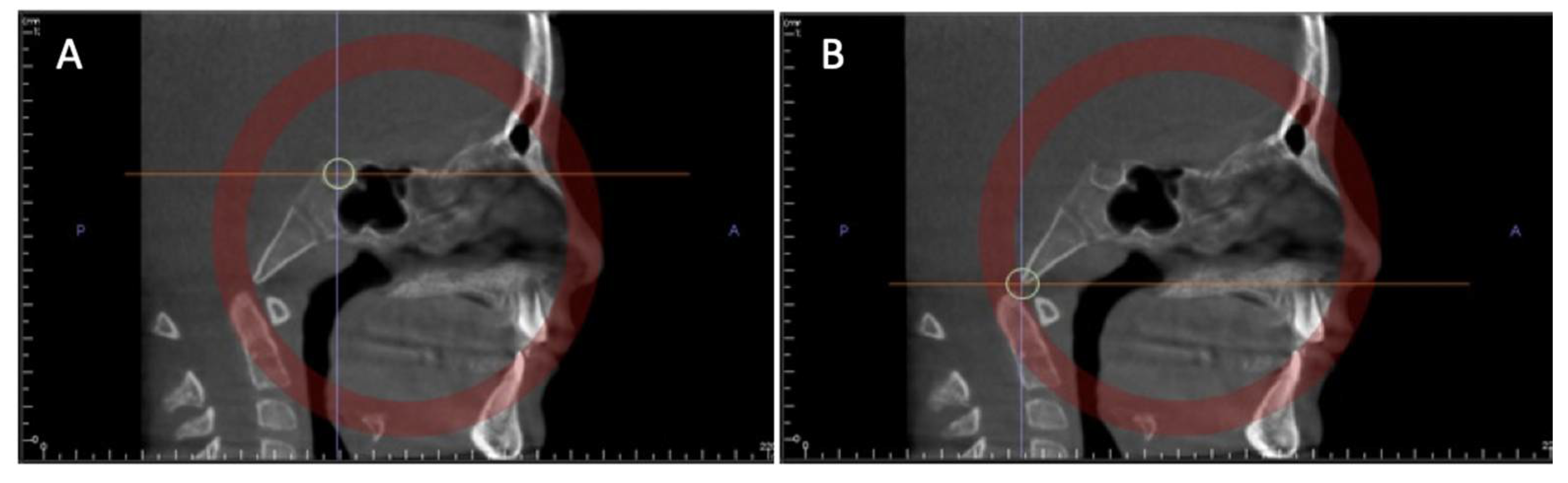
2.1.3. 3D Imaging and Spheno-Occipital Synchondrosis Ossification
2.2. Treatment Diagnosis Using a 3D Scanner
3. Treatment and Monitoring of Orthodontic Treatment
3.1. 3D Imaging for Indirect-Direct Bonding
3.2. Clear Aligner Manufacturing
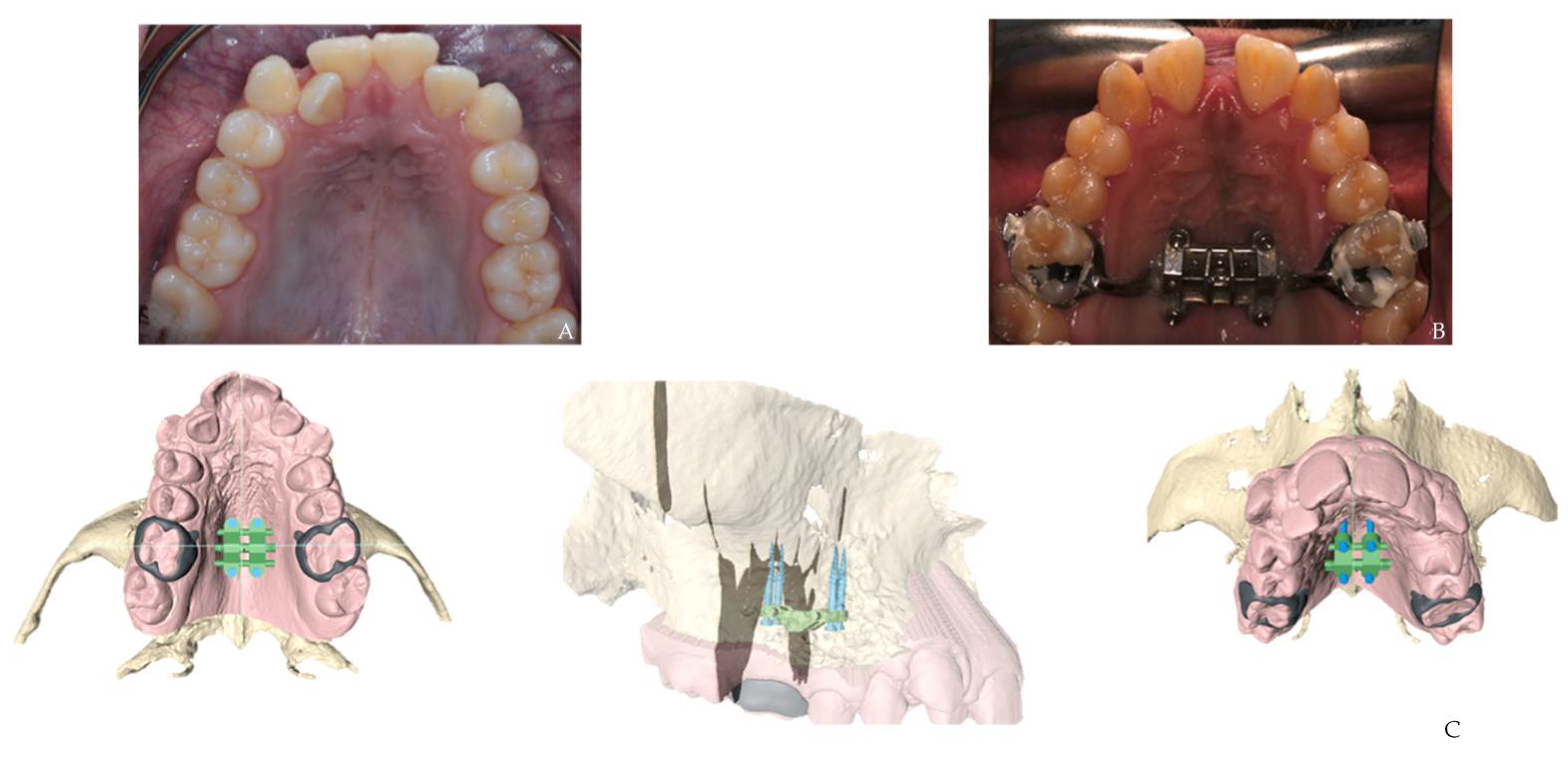
3.3. Surgical Guide Technique for Miniscrew Placement
3.4. Corticotomy Technique Using CAD/CAM 3D Printed Surgical Guides
3.5. Assessment of Tooth Movement in a Three-Dimensional Plane
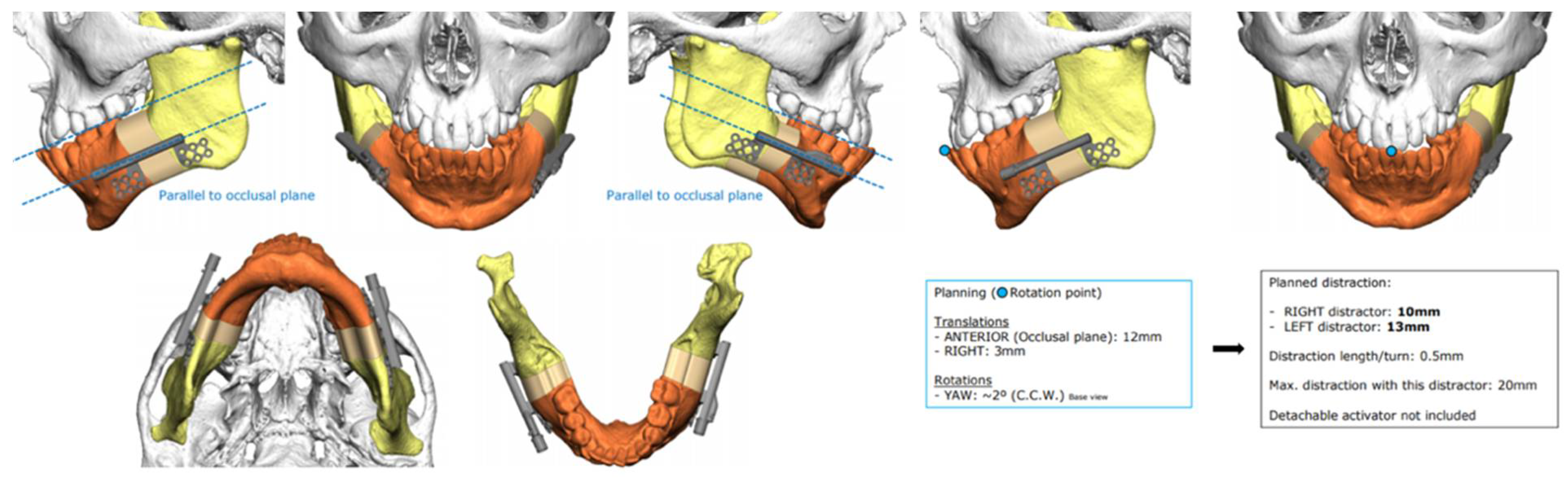
3.6. Distraction Osteogenesis
3.7. Orthognathic Surgery
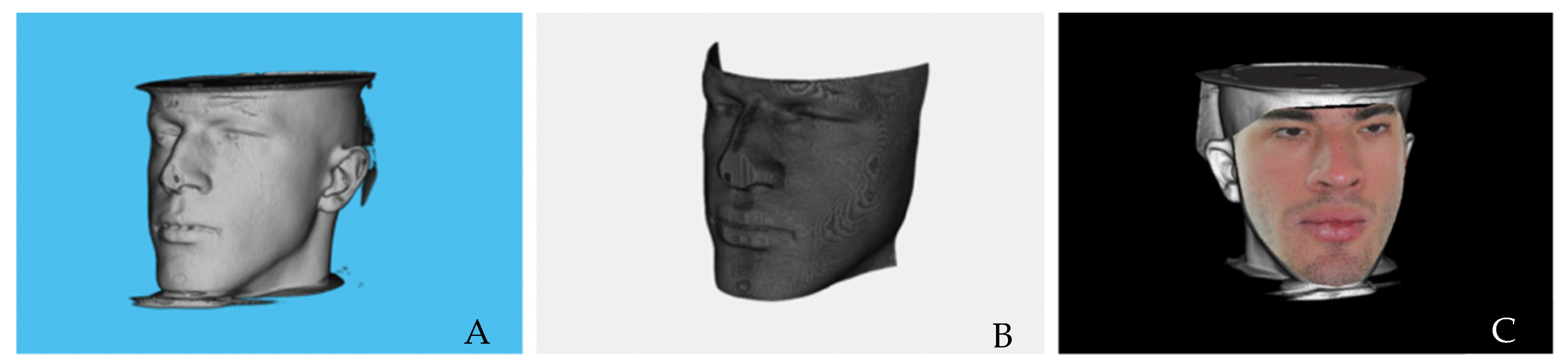
3.7.1. Photorealistic Visualization of Rendered CT Images
3.7.2. Orthognathic Surgery 3D Planning—Surgical Splint Manufacturing
4. Retention and Outcome Assessment
4.1. Retainer Manufacturing Technique Using CAD-CAM Technology
4.2. Three-Dimensional Prognosis of Dental Arch Shape after Orthodontic Treatment
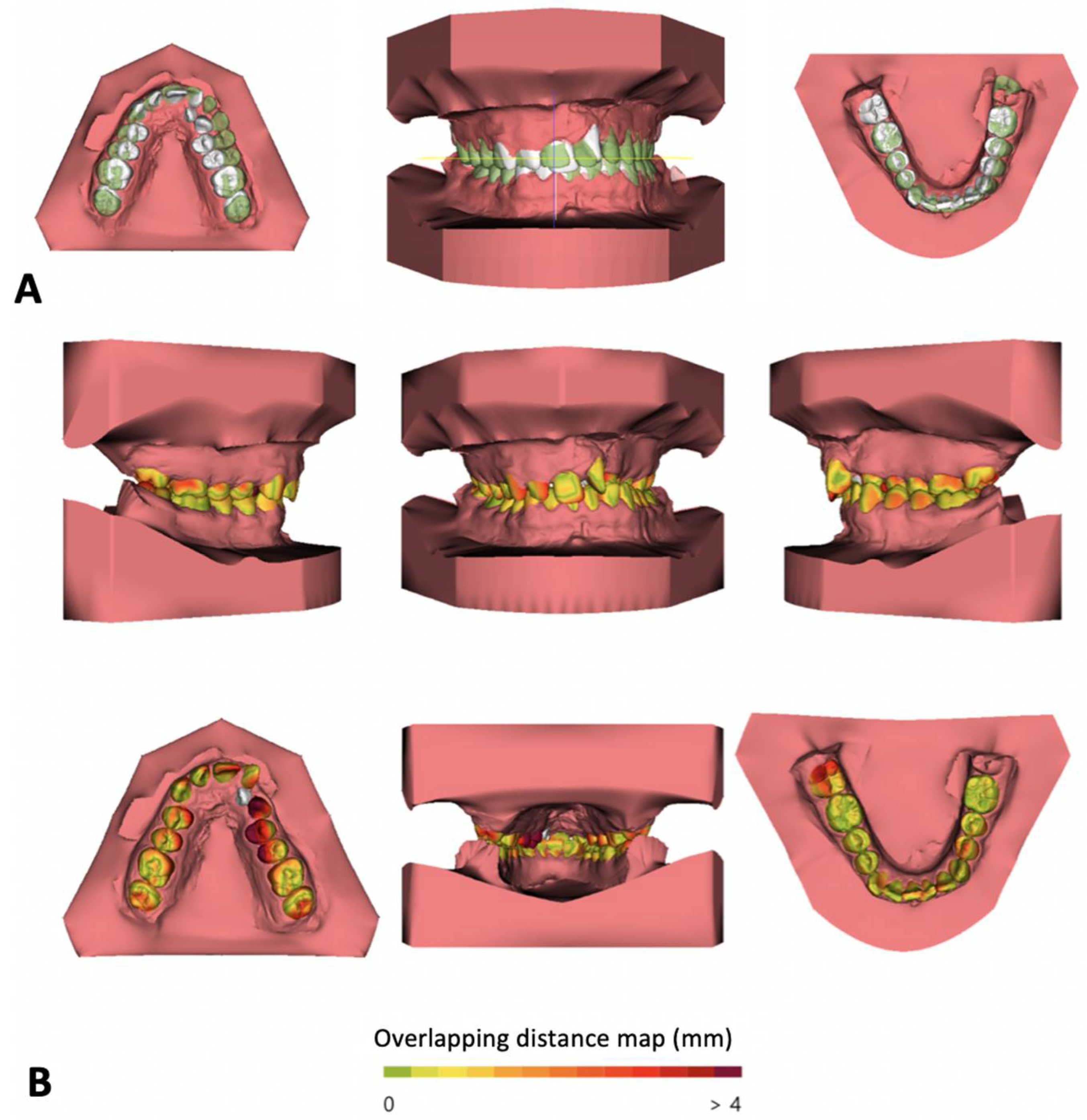
4.3. Superimposition on Outcome Analysis
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Martin, C.B.; Chalmers, E.V.; McIntyre, G.T.; Cochrane, H.; Mossey, P.A. Orthodontic Scanners: What’s Available? J. Orthod. 2015, 42, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, A.; Horodynski, M.; De Stefano, A.; Palaia, G.; Polimeni, A.; Romeo, U.; Guercio-Monaco, E.; Galluccio, G. CBCT and Intra-Oral Scanner: The Advantages of 3D Technologies in Orthodontic Treatment. Int. J. Environ. Res. Public Healthy 2020, 17, 9428. [Google Scholar] [CrossRef] [PubMed]
- Keim, R.G.; Gottlieb, E.L.; Nelson, A.H.; Vogels, D.S. 2008 JCO study of orthodontic diagnosis and treatment procedures, part 1: Results and trends. J. Clin. Orthod. JCO 2008, 42, 625–640. [Google Scholar]
- Son, K.; Lee, W.-S.; Lee, K.-B. Prediction of the learning curves of 2 dental CAD software programs. J. Prosthet. Dent. 2019, 121, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Solem, R.C. Utilizing three-dimensional data in orthodontic practice and research. Orthod. Craniofacial Res. 2017, 20, 114–118. [Google Scholar] [CrossRef]
- Manosudprasit, A.; Haghi, A.; Allareddy, V.; Masoud, M.I. Diagnosis and treatment planning of orthodontic patients with 3-dimensional dentofacial records. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1083–1091. [Google Scholar] [CrossRef]
- Karatas, O.H.; Toy, E. Three-dimensional imaging techniques: A literature review. Eur. J. Dent. 2014, 8, 132–140. [Google Scholar] [CrossRef]
- De Grauwe, A.; Ayaz, I.; Shujaat, S.; Dimitrov, S.; Gbadegbegnon, L.; Vannet, B.V.; Jacobs, R. CBCT in orthodontics: A systematic review on justification of CBCT in a paediatric population prior to orthodontic treatment. Eur. J. Orthod. 2019, 41, 381–389. [Google Scholar] [CrossRef]
- Hippisley-Cox, J.; Pringle, M.; Cater, R.; Wynn, A.; Hammersley, V.; Coupland, C.; Hapgood, R.; Horsfield, P.; Teasdale, S.; Johnson, C. The electronic patient record in primary care--regression or progression? A cross sectional study. BMJ 2003, 326, 1439–1443. [Google Scholar] [CrossRef]
- European Commission. Radiation Protection No 172: Cone Beam CT for Dental and Maxillofacial Radiology. Evidence Based Guidelines. 2012. Available online: http://www.sedentexct.eu/files/radiation_protection_172.pdf (accessed on 10 November 2021).
- Juerchott, A.; Freudlsperger, C.; Weber, D.; Jende, J.M.E.; Saleem, M.A.; Zingler, S.; Lux, C.J.; Bendszus, M.; Heiland, S.; Hilgenfeld, T. In Vivo Comparison of MRI- and CBCT-Based 3D Cephalometric Analysis: Beginning of a Non-Ionizing Diagnostic Era in Craniomaxillofacial Imaging? Eur. Radiol. 2020, 30, 1488–1497. [Google Scholar] [CrossRef]
- Pinheiro, M.; Ma, X.; Fagan, M.J.; McIntyre, G.T.; Lin, P.; Sivamurthy, G.; Mossey, P.A. A 3D cephalometric protocol for the accurate quantification of the craniofacial symmetry and facial growth. J. Biol. Eng. 2019, 13, 42. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.; Chaushu, S.; Casap-Caspi, N. Cone-beam Computed Tomography and the Orthosurgical Management of Impacted Teeth. J. Am. Dent. Assoc. 2010, 141, 14S–18S. [Google Scholar] [CrossRef]
- Pittayapat, P.; Limchaichana-Bolstad, N.; Willems, G.; Jacobs, R. Three-dimensional cephalometric analysis in orthodontics: A systematic review. Orthod. Craniofacial Res. 2013, 17, 69–91. [Google Scholar] [CrossRef] [PubMed]
- Tanna, N.K.; AlMuzaini, A.A.; Mupparapu, M. Imaging in Orthodontics. Dent. Clin. North Am. 2021, 65, 623–641. [Google Scholar] [CrossRef] [PubMed]
- Cossellu, G.; Biagi, R.; Sarcina, M.; Mortellaro, C.; Farronato, G. Three-Dimensional Evaluation of Upper Airway in Patients with Obstructive Sleep Apnea Syndrome During Oral Appliance Therapy. J. Craniofacial Surg. 2015, 26, 745–748. [Google Scholar] [CrossRef]
- Schendel, S.A.; Broujerdi, J.A.; Jacobson, R.L. Three-dimensional upper-airway changes with maxillomandibular advancement for obstructive sleep apnea treatment. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 385–393. [Google Scholar] [CrossRef]
- Brunetto, D.P.; Velasco, L.; Koerich, L.; Araújo, M.T.D.S. Prediction of 3-dimensional pharyngeal airway changes after orthognathic surgery: A preliminary study. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 299–309. [Google Scholar] [CrossRef]
- Görgülü, S.; Gokce, S.M.; Olmez, H.; Sagdic, D.; Ors, F. Nasal cavity volume changes after rapid maxillary expansion in adolescents evaluated with 3-dimensional simulation and modeling programs. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 633–640. [Google Scholar] [CrossRef]
- Vale, F.; Francisco, I.; Lucas, A.; Roseiro, A.; Caramelo, F.; Sobral, A. Timing of Spheno-Occipital Synchondrosis Ossification in Children and Adolescents with Cleft Lip and Palate: A Retrospective Case-Control Study. Int. J. Environ. Res. Public Heal. 2020, 17, 8889. [Google Scholar] [CrossRef]
- Rheude, B.; Sadowsky, P.L.; Ferriera, A.; Jacobson, A. An evaluation of the use of digital study models in orthodontic diagnosis and treatment planning. Angle Orthod. 2005, 75, 300–304. [Google Scholar]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 161–170. [Google Scholar] [CrossRef] [PubMed]
- El-Timamy, A.M.; El-Sharaby, F.A.; Eid, F.H.; Mostafa, Y.A. Three-dimensional imaging for indirect-direct bonding. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 928–931. [Google Scholar] [CrossRef] [PubMed]
- Ritto, A. Construção Dos Alinhadores Transparentes No Consultório. Dentistry 2011, 6, 26–36. [Google Scholar]
- Möhlhenrich, S.C.; Brandt, M.; Kniha, K.; Bock, A.; Prescher, A.; Hölzle, F.; Modabber, A.; Danesh, G. Suitability of virtual plaster models superimposed with the lateral cephalogram for guided paramedian orthodontic mini-implant placement with regard to the bone support. J. Orofac. Orthop. Fortschr. Der Kieferorthopädie 2020, 81, 340–349. [Google Scholar] [CrossRef]
- Cassetta, M.; Giansanti, M. Accelerating orthodontic tooth movement: A new, minimally-invasive corticotomy technique using a 3D-printed surgical template. Med. Oral Patol. Oral Y Cir. Bucal 2016, 21, e483–e487. [Google Scholar] [CrossRef]
- Maino, B.G.; Paoletto, E.; Lombardo, L.; Siciliani, G. A Three-Dimensional Digital Insertion Guide for Palatal Miniscrew Placement. J. Clin. Orthod. JCO 2016, 50, 12–22. [Google Scholar]
- Lee, R.J.; Weissheimer, A.; Pham, J.; Go, L.; Menezes, L.; Redmond, W.R.; Loos, J.F.; Sameshima, G.T.; Tong, H. Three-dimensional monitoring of root movement during orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 132–142. [Google Scholar] [CrossRef]
- Cha, B.K.; Lee, J.Y.; Jost-Brinkmann, P.-G.; Yoshida, N. Analysis of tooth movement in extraction cases using three-dimensional reverse engineering technology. Eur. J. Orthod. 2007, 29, 325–331. [Google Scholar] [CrossRef]
- Talaat, S.; Kaboudan, A.; Breuning, H.; Ragy, N.; Elshebiny, T.; Kula, K.; Ghoneima, A. Reliability of linear and angular dental measurements with the OrthoMechanics Sequential Analyzer. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 264–269. [Google Scholar] [CrossRef]
- Li, B.; Sun, H.; Zeng, F.; Zhang, T.; Wang, X. Accuracy of a CAD/CAM surgical template for mandibular distraction: A preliminary study. Br. J. Oral Maxillofac. Surg. 2018, 56, 814–819. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Hsung, T.-C.; Khambay, B. Reducing cone beam CT scan height as a method of radiation reduction for photorealistic three-dimensional orthognathic planning. J. Cranio-Maxillofacial Surg. 2015, 43, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Plooij, J.M.; Maal, T.J.; Haers, P.; Borstlap, W.A.; Kuijpers-Jagtman, A.M.; Bergé, S.J. Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery. A systematic review. Int. J. Oral Maxillofac. Surg. 2011, 40, 341–352. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, M. Realistic 3D Reconstruction from CT Images. Master’s Thesis, Faculty of Sciences and Technology, University of Coimbra, Coimbra, Portugal, 2022. [Google Scholar]
- Ayoub, A.; Xiao, Y.; Khambay, B.; Siebert, J.; Hadley, D. Towards building a photo-realistic virtual human face for craniomaxillofacial diagnosis and treatment planning. Int. J. Oral Maxillofac. Surg. 2007, 36, 423–428. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, C.D.; Manisali, M.; Naini, F.B. Three-dimensional virtual surgical planning (3D-VSP) in orthognathic surgery: Advantages, disadvantages and pitfalls. J. Orthod. 2021, 48, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Aristizábal, J.F.; Martínez-Smit, R.; Díaz, C.; Filho, V.A.P.; Pereira, V.A. Surgery-first approach with 3D customized passive self-ligating brackets and 3D surgical planning: Case report. Dent. Press J. Orthod. 2018, 23, 47–57. [Google Scholar] [CrossRef]
- Vale, F.D.; Scherzberg, J.; Cavaleiro, J.; Sanz, D.; Caramelo, F.; Maló, L.; Marcelino, J.P. 3D virtual planning in orthognathic surgery and CAD/CAM surgical splints generation in one patient with craniofacial microsomia: A case report. Dent. Press J. Orthod. 2016, 21, 89–100. [Google Scholar] [CrossRef]
- Elnagar, M.H.; Aronovich, S.; Kusnoto, B. Digital Workflow for Combined Orthodontics and Orthognathic Surgery. Oral Maxillofac. Surg. Clin. North Am. 2020, 32, 1–14. [Google Scholar] [CrossRef]
- Teixeira, A.O.D.B.; Almeida, M.A.D.O.; Almeida, R.C.D.C.; Maués, C.P.; Pimentel, T.; Ribeiro, D.P.B.; de Medeiros, P.J.; Quintão, C.C.A.; Carvalho, F.D.A.R. Three-dimensional accuracy of virtual planning in orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 674–683. [Google Scholar] [CrossRef]
- Tonin, R.H.; Filho, L.I.; Yamashita, A.L.; Ferraz, F.W.D.S.; Tolentino, E.D.S.; Previdelli, I.T.D.S.; Brum, B.; Iwaki, L.C.V. Accuracy of 3D virtual surgical planning for maxillary positioning and orientation in orthognathic surgery. Orthod. Craniofacial Res. 2020, 23, 229–236. [Google Scholar] [CrossRef]
- Nasef, A.A.; El-Beialy, A.R.; Mostafa, Y.A. Virtual techniques for designing and fabricating a retainer. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 394–398. [Google Scholar] [CrossRef]
- Wolf, M.; Schumacher, P.; Jäger, F.; Wego, J.; Fritz, U.; Korbmacher-Steiner, H.; Jäger, A.; Schauseil, M. Novel Lingual Retainer Created Using CAD/CAM Technology: Evaluation of Its Positioning Accuracy. J. Orofac. Orthop. 2015, 76, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Asquith, J.; McIntyre, G. Dental Arch Relationships on Three-Dimensional Digital Study Models and Conventional Plaster Study Models for Patients with Unilateral Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2012, 49, 530–534. [Google Scholar] [CrossRef] [PubMed]
- Farronato, G.; Salvadori, S.; Nolet, F.; Zoia, A.; Farronato, D. Assessment of inter- and intra-operator cephalometric tracings on cone beam CT radiographs: Comparison of the precision of the cone beam CT versus the latero-lateral radiograph tracing. Prog. Orthod. 2014, 15, 1–7. [Google Scholar] [CrossRef] [PubMed][Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Francisco, I.; Ribeiro, M.P.; Marques, F.; Travassos, R.; Nunes, C.; Pereira, F.; Caramelo, F.; Paula, A.B.; Vale, F. Application of Three-Dimensional Digital Technology in Orthodontics: The State of the Art. Biomimetics 2022, 7, 23. https://doi.org/10.3390/biomimetics7010023
Francisco I, Ribeiro MP, Marques F, Travassos R, Nunes C, Pereira F, Caramelo F, Paula AB, Vale F. Application of Three-Dimensional Digital Technology in Orthodontics: The State of the Art. Biomimetics. 2022; 7(1):23. https://doi.org/10.3390/biomimetics7010023
Chicago/Turabian StyleFrancisco, Inês, Madalena Prata Ribeiro, Filipa Marques, Raquel Travassos, Catarina Nunes, Flávia Pereira, Francisco Caramelo, Anabela Baptista Paula, and Francisco Vale. 2022. "Application of Three-Dimensional Digital Technology in Orthodontics: The State of the Art" Biomimetics 7, no. 1: 23. https://doi.org/10.3390/biomimetics7010023
APA StyleFrancisco, I., Ribeiro, M. P., Marques, F., Travassos, R., Nunes, C., Pereira, F., Caramelo, F., Paula, A. B., & Vale, F. (2022). Application of Three-Dimensional Digital Technology in Orthodontics: The State of the Art. Biomimetics, 7(1), 23. https://doi.org/10.3390/biomimetics7010023









