Intraoperative Assessment of Coronary Resistances: A New Quality Marker and Potential Tool to Predict Early Graft Failure after Coronary Artery Bypass Grafting?
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Inclusion Criteria
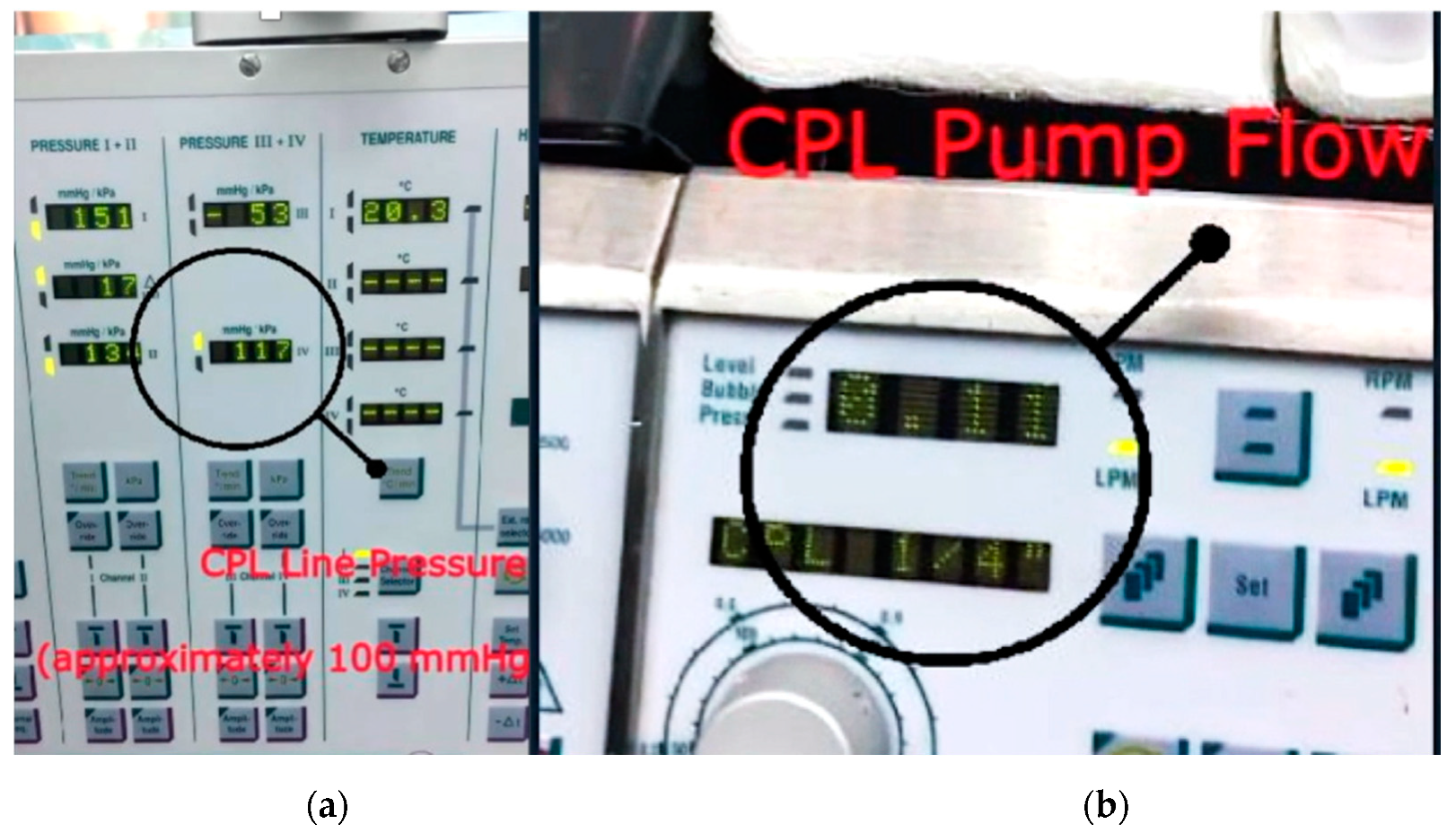
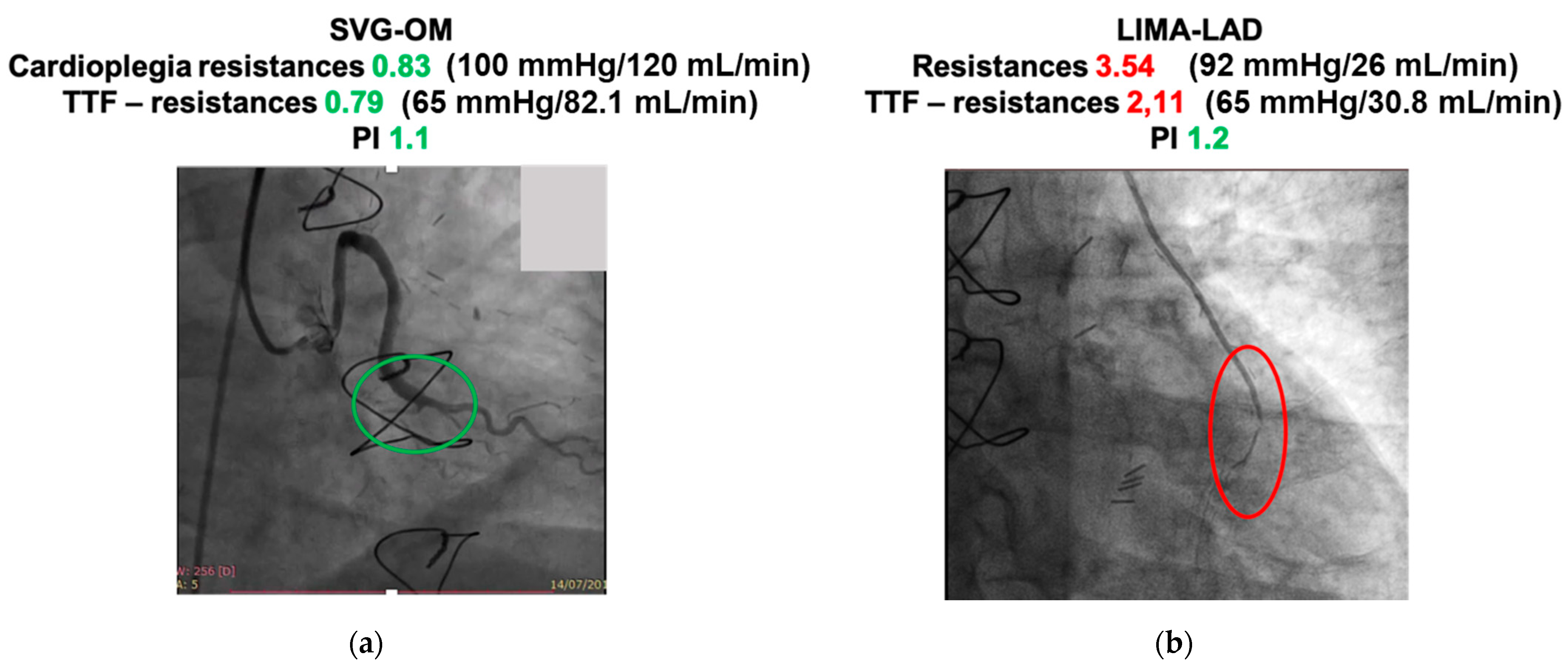
2.2. Graft Flowmetry and Coronary Resistances
2.3. Endpoints of the Study
2.4. Statistical Analyses
3. Results
3.1. Intraoperative Flow Measurements
3.2. Follow-Up Results
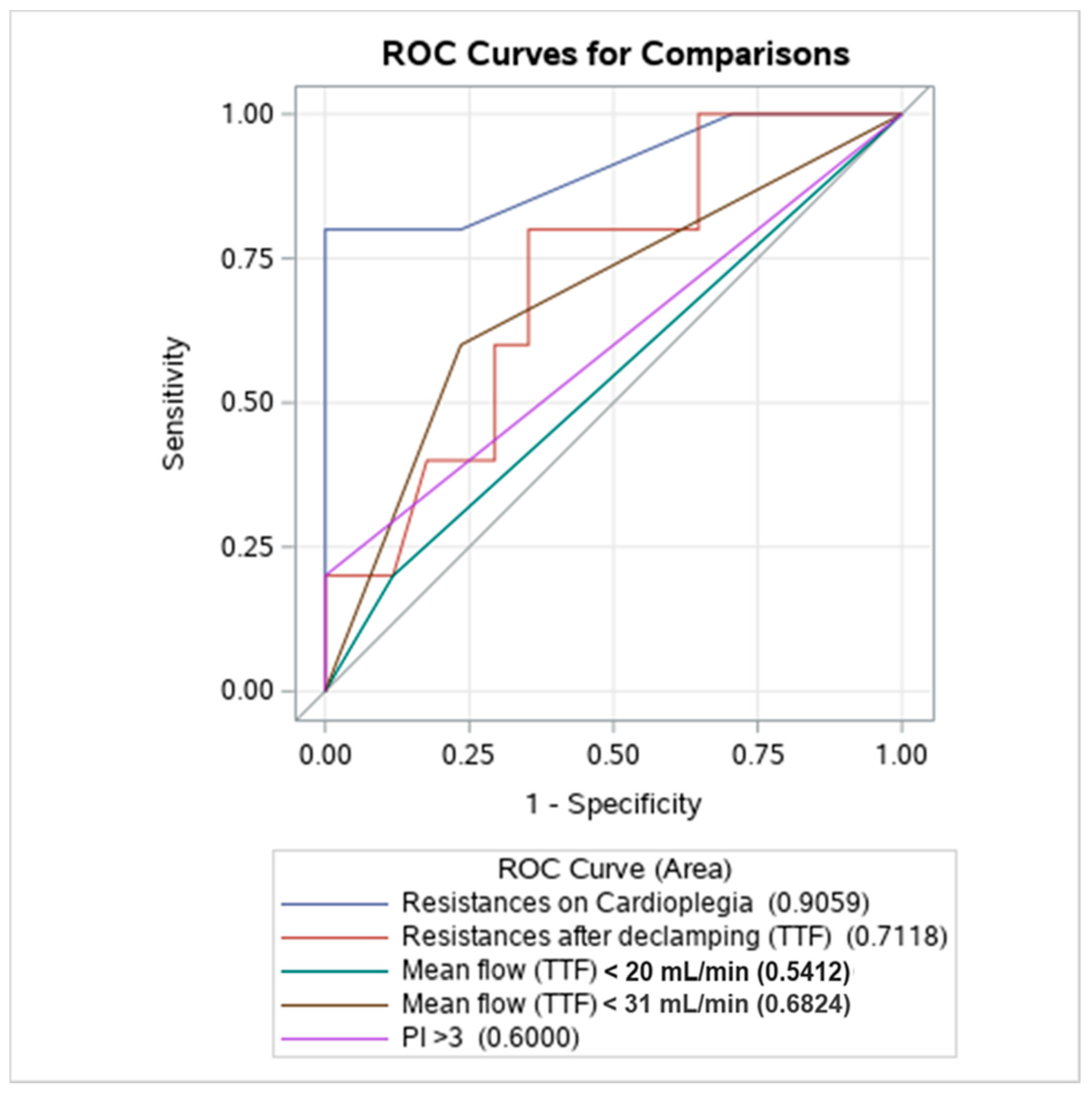
3.3. Discriminant Analysis
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Russ. J. Cardiol. 2019, 40, 87–165. [Google Scholar]
- Quin, J.; Lucke, J.; Hattler, B.; Gupta, S.; Baltz, J.; Bishawi, M.; Almassi, G.H.; Grover, F.L.; Collins, J.; Shroyer, A.L. Surgeon judgment and utility of transit time flow probes in coronary artery bypass grafting surgery. JAMA Surg. 2014, 149, 1182–1187. [Google Scholar] [CrossRef] [PubMed]
- Amin, S.; Pinho-Gomes, A.-C.; Taggart, D.P. Relationship of Intraoperative Transit Time Flowmetry Findings to Angiographic Graft Patency at Follow-Up. Ann. Thorac. Surg. 2016, 101, 1996–2006. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, H.; Takazawa, A.; Yoshitake, A.; Tochii, M.; Tokunaga, C.; Hayashi, J.; Izumida, H.; Kaneyuki, D.; Asakura, T.; Iguchi, A. Intraoperative transit-time flowmetry in patients undergoing coronary surgery to determine relationships between graft flow and patency and prior coronary interventions and flow demand: A retrospective study. J. Cardiothorac. Surg. 2018, 13, 121. [Google Scholar] [CrossRef] [PubMed]
- Belboul, A.; Rådberg, G.; Roberts, D.; Dernevik, L. Intraoperative assessment of coronary flow and coronary vascular resistance during coronary bypass surgery. Scand. Cardiovasc. J. 1999, 33, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Rubino, A.S.; Onorati, F.; Scalas, C.; Serraino, G.F.; Marsico, R.; Gelsomino, S.; Lorusso, R.; Renzulli, A. Intra-aortic balloon pumping recruits graft flow reserve by lowering coronary resistances. Int. J. Cardiol. 2012, 154, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Onorati, F.; Santarpino, G.; Rubino, A.; Cristodoro, L.; Scalas, C.; Renzulli, A. Intraoperative bypass graft flow in intra-aortic balloon pump-supported patients: Differences in arterial and venous sequential conduits. J. Thorac. Cardiovasc. Surg. 2009, 138, 54–61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Une, D.; Deb, S.; Chikazawa, G.; Kommaraju, K.; Tsuneyoshi, H.; Karkhanis, R.; Singh, S.; Vincent, J.; Tsubota, H.; Sever, J.; et al. Cut-off values for transit time flowmetry: Are the revision criteria appropriate? J. Card. Surg. 2013, 28, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Di Giammarco, G.; Pano, M.; Cirmeni, S.; Pelini, P.; Vitolla, G.; Di Mauro, M. Predictive value of intraoperative transit-time flow measurement for short-term graft patency in coronary surgery. J. Thorac. Cardiovasc. Surg. 2006, 132, 468–474. [Google Scholar] [CrossRef] [PubMed]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A non- parametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Efron, B.; Tibshirani, R. Bootstrap Methods for Standard Errors, Confidence Intervals, and Other Measures of Statistical Accuracy. Stat. Sci. 1986, 1, 54–75. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 26 May 2021).
- D’Ancona, G.; Karamanoukian, H.L.; Ricci, M.; Schmid, S.; Bergsland, J.; Salerno, T.A. Graft revision after transit time flow measurement in off-pump coronary artery bypass grafting. Eur. J. Cardiothorac. Surg. 2000, 17, 287–293. [Google Scholar] [CrossRef]
- Thuijs, D.J.; Bekker, M.W.; Taggart, D.P.; Kappetein, A.P.; Kieser, T.M.; Wendt, D.; Di Giammarco, G.; Trachiotis, G.D.; Puskas, J.D.; Head, S.J. Improving coronary artery bypass grafting: A systematic review and metaanalysis on the impact of adopting transit-time flow measurement. Eur. J. Cardio-Thorac. Surg. 2019, 56, 654–663. [Google Scholar] [CrossRef] [PubMed]
- Balacumaraswami, L.; Taggart, D.P. Digital tools to facilitate intraoperative coronary artery bypass graft assessment. Semin. Thorac. Cardiovasc. Surg. 2004, 16, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.K.; Desai, N.D.; Chikazawa, G.; Tsuneyoshi, H.; Vincent, J.; Zagorski, B.M.; Pen, V.; Moussa, F.; Cohen, G.N.; Christakis, G.T.; et al. The Graft Imaging to Improve Patency (GRIIP) clinical trial results. J. Thorac. Cardiovasc. Surg. 2010, 139, 294–301.e1. [Google Scholar] [CrossRef] [PubMed]
- Klocke, F.J. Coronary blood flow in man. Prog. Cardiovasc. Dis. 1976, 19, 117–166. [Google Scholar] [CrossRef]
- Quin, J.A.; Noubani, M.; Rove, J.Y.; Krstacic, J.E.; Hattler, B.; Collins, J.F.; Grover, F.L.; Almassi, G.H.; Shroyer, A.L.; Veterans Affairs Randomized On/Off Bypass Follow-up Study (ROOBY-FS) Group. Coronary Artery Bypass Grafting Transit Time Flow Measurement: Graft Patency and Clinical Outcomes. Ann. Thorac. Surg. 2021, 112, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Hol, P.K.; Fosse, E.; Mork, B.E.; Lundblad, R.; Rein, K.A.; Lingaas, P.S.; Geiran, O.; Svennevig, J.L.; Tonnessen, T.I.; Nitter-Hauge, S.; et al. Graft control by transit time flow measurement and intraoperative angiography in coronary artery bypass surgery. Hear. Surg. Forum 2001, 4, 254–258. [Google Scholar]
| Baseline | n = 63 |
|---|---|
| Age, years | 65.1 ± 8.9 |
| Female | 20 (31.7) |
| Hypertension | 43 (68.3) |
| Dyslipidemia | 23 (36.5) |
| Diabetes | 29 (46.0) |
| Peripheral vascular disease | 11 (17.5) |
| COPD | 10 (15.9) |
| Creatinine >200 mmol/L | 4 (6.3) |
| Dialysis | 1 (1.6) |
| Prior myocardial infarction | 21 (33.3) |
| Left main stem | 39 (61.9) |
| LVEF | |
| >50% | 29 (46.0) |
| 30–50% | 31 (50.8) |
| <30% | 2 (3.2) |
| Intraoperative Details | |
| Cardiopulmonary bypass time, min | 104.4 ± 42.2 |
| Aortic cross-clamping time, min | 88.5 ± 33.0 |
| Flowmetry | Graft Type |
|---|---|
| Parameter | SVG-Right coronary artery (n = 6) |
| Flow during cardioplegia | 120.0 ± 31.6 |
| CR cardioplegia | 0.84 ± 0.19 |
| Mean TTF flow | 47.5 ± 24.0 |
| CR TTF | 1.41 ± 0.53 |
| PI | 1.4 ± 0.6 |
| Parameter | SVG-Posterior descending artery (n = 8) |
| Flow during cardioplegia | 98.8 ± 14.6 |
| CR cardioplegia | 1.00 ± 0.20 |
| Mean TTF flow | 35.5 ± 19.7 |
| CR TTF | 2.83 ± 4.26 |
| PI | 1.9 ± 0.9 |
| Parameter | SVG-Obtuse Marginal (n = 38) |
| Flow during cardioplegia | 104.5 ± 32.4 |
| CR cardioplegia | 1.03 ± 0.30 |
| Mean TTF flow | 39.2 ± 21.4 |
| CR TTF | 1.94 ± 1.43 |
| PI | 1.5 ± 0.5 |
| Parameter | SVG-Ramus intermedius (n = 17) |
| Flow during cardioplegia | 118.2 ± 32.6 |
| CR cardioplegia | 0.89 ± 0.23 |
| Mean TTF flow | 32.7 ± 19.2 |
| CR TTF | 2.05 ± 1.38 |
| PI | 1.6 ± 0.6 |
| Parameter | SVG-Diagonal (n = 17) |
| Flow during cardioplegia | 110.0 ± 26.7 |
| CR cardioplegia | 0.92 ± 0.18 |
| Mean TTF flow | 29.4 ± 17.8 |
| CR TTF | 2.96 ± 2.53 |
| PI | 1.8 ± 0.5 |
| Parameter | LIMA-Left anterior descending (20) |
| Flow during cardioplegia | 68.9 ± 33.0 |
| CR cardioplegia | 1.33 ± 0.72 |
| Mean TTF flow | 49.1 ± 33.4 |
| CR TTF | 1.49 ± 0.86 |
| PI | 1.6 ± 0.7 |
| Parameter | SVG- Left anterior descending (n = 7) |
| Flow during cardioplegia | 110.0 ± 29.4 |
| CR cardioplegia | 0.98 ± 0.33 |
| Mean TTF flow | 39.5 ± 25.6 |
| CR TTF | 1.74 ± 0.88 |
| PI | 1.5 ± 0.4 |
| Parameter | Patent Grafts (n = 17) | Occluded Grafts (n = 5) | p |
|---|---|---|---|
| Flow during cardioplegia | 100.2 ± 27.7 | 49.2 ± 31.5 | 0.0022 |
| CR cardioplegia | 1.03 ± 0.33 | 2.70 ± 1.57 | 0.0029 |
| Mean TTF flow | 54.2 ± 25.5 | 30.2 ± 17.1 | 0.06 |
| CR TTF | 1.74 ± 0.22 | 6.38 ± 9.92 | 0.09 |
| PI | 1.7 ± 0.6 | 2.3 ± 1.6 | 0.44 |
| Parameter | OR | 95% CI | p |
| CR cardioplegia | 25.1 | 2.1–>999 | 0.0420 |
| CR TTF | 1.28 | 0.74–2.20 | 0.37 |
| TTF < 20 mL/min | 1.88 | 0.13–26.2 | 0.64 |
| TTF < 31 mL/min | 4.88 | 0.59–40.3 | 0.14 |
| PI | 1.96 | 0.68–5.64 | 0.21 |
| PI > 3 | 11.78 | 0.11–>999 | 0.23 |
| Variables | Cut-Off | Sensitivity | Specificity |
|---|---|---|---|
| CR cardioplegia | ≥2.0 (2.0–3.5) | 80.0% (50.0–100) | 100% (100–100) |
| CR TTF | ≥2.03 (1.16–24.1) | 80.0% (50.0–100) | 64.7% (16.7–100) |
| Mean TTF flow | ≤51.8 (30–51.8) | 100% (0–100) | 58.8% (33.3–100) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rubino, A.S.; Ceresa, F.; Mammana, L.; Vite, G.; Cullurà, G.; Palermo, A.; Leonardi, A.; De Donno, B.F.; Patanè, F. Intraoperative Assessment of Coronary Resistances: A New Quality Marker and Potential Tool to Predict Early Graft Failure after Coronary Artery Bypass Grafting? J. Cardiovasc. Dev. Dis. 2021, 8, 163. https://doi.org/10.3390/jcdd8120163
Rubino AS, Ceresa F, Mammana L, Vite G, Cullurà G, Palermo A, Leonardi A, De Donno BF, Patanè F. Intraoperative Assessment of Coronary Resistances: A New Quality Marker and Potential Tool to Predict Early Graft Failure after Coronary Artery Bypass Grafting? Journal of Cardiovascular Development and Disease. 2021; 8(12):163. https://doi.org/10.3390/jcdd8120163
Chicago/Turabian StyleRubino, Antonino Salvatore, Fabrizio Ceresa, Liborio Mammana, Giuseppe Vite, Gianluca Cullurà, Augusto Palermo, Aurora Leonardi, Bruna Filomena De Donno, and Francesco Patanè. 2021. "Intraoperative Assessment of Coronary Resistances: A New Quality Marker and Potential Tool to Predict Early Graft Failure after Coronary Artery Bypass Grafting?" Journal of Cardiovascular Development and Disease 8, no. 12: 163. https://doi.org/10.3390/jcdd8120163
APA StyleRubino, A. S., Ceresa, F., Mammana, L., Vite, G., Cullurà, G., Palermo, A., Leonardi, A., De Donno, B. F., & Patanè, F. (2021). Intraoperative Assessment of Coronary Resistances: A New Quality Marker and Potential Tool to Predict Early Graft Failure after Coronary Artery Bypass Grafting? Journal of Cardiovascular Development and Disease, 8(12), 163. https://doi.org/10.3390/jcdd8120163









