Effect of Evolocumab on Lipoprotein(a) and PCSK9 in Healthy Individuals with Elevated Lipoprotein(a) Level
Abstract
1. Introduction
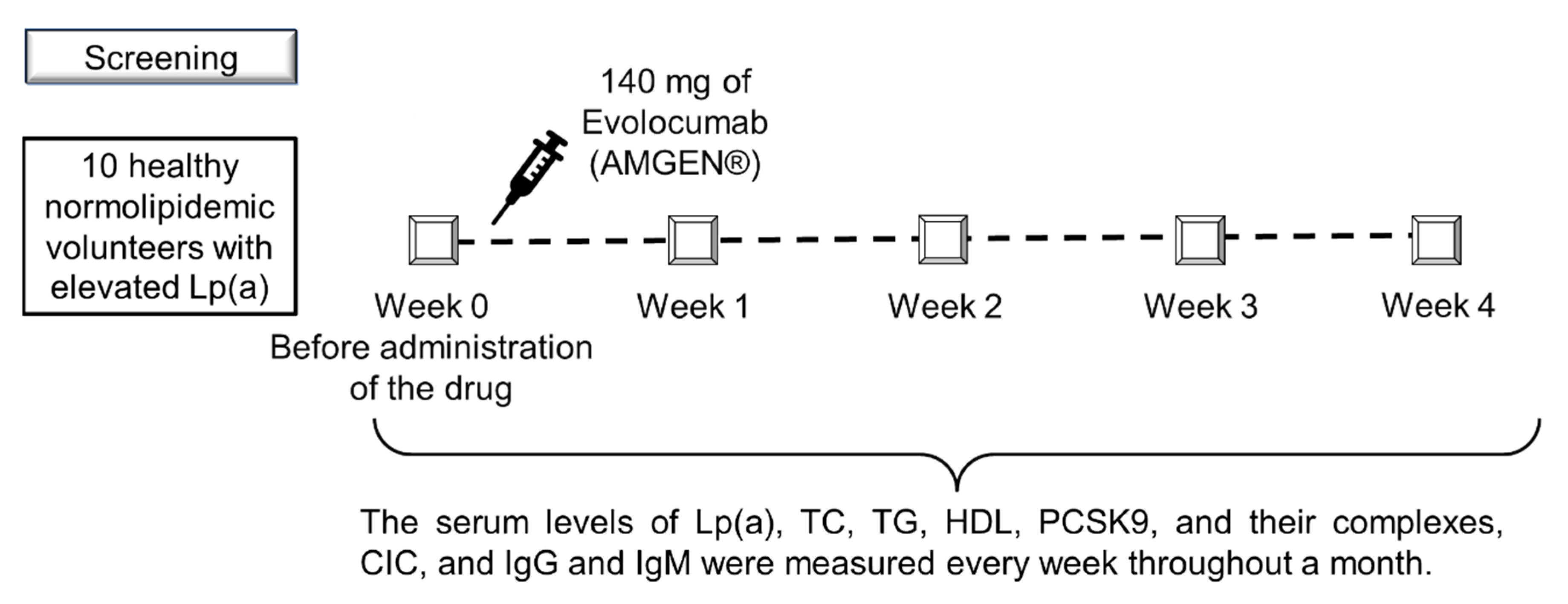
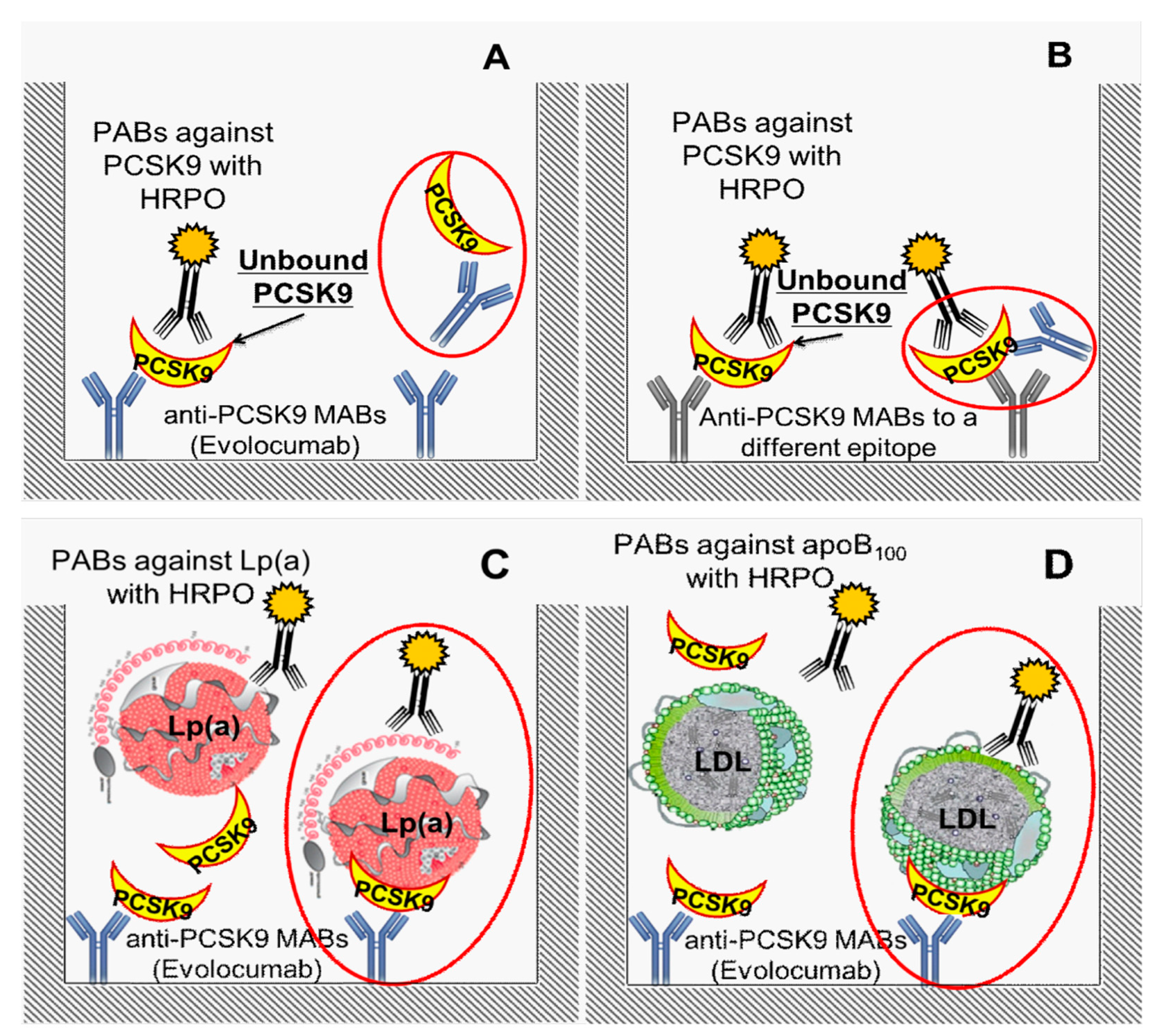
2. Materials and Methods
- Atherosclerotic cardiovascular disease (ischemic heart disease, stroke, peripheral arterial disease) requiring lipid-lowering therapy;
- Positive stress test;
- Chronic inflammatory diseases;
- Active liver disease;
- Renal failure (Cockcroft and Gault creatinine clearance of less than 60 mL/min);
- Type 2 diabetes mellitus;
- Uncontrolled hypothyroidism (TSH level of 1.5 UNL);
- Increased level of creatine kinase (CK) of 3 UNL;
- Immunodeficiency or autoimmune disorders;
- Administration of any lipid-lowering drugs or supplements affecting the lipid profile;
- Significant clinical or psychological condition that may interrupt the experiment, including alcohol abuse.
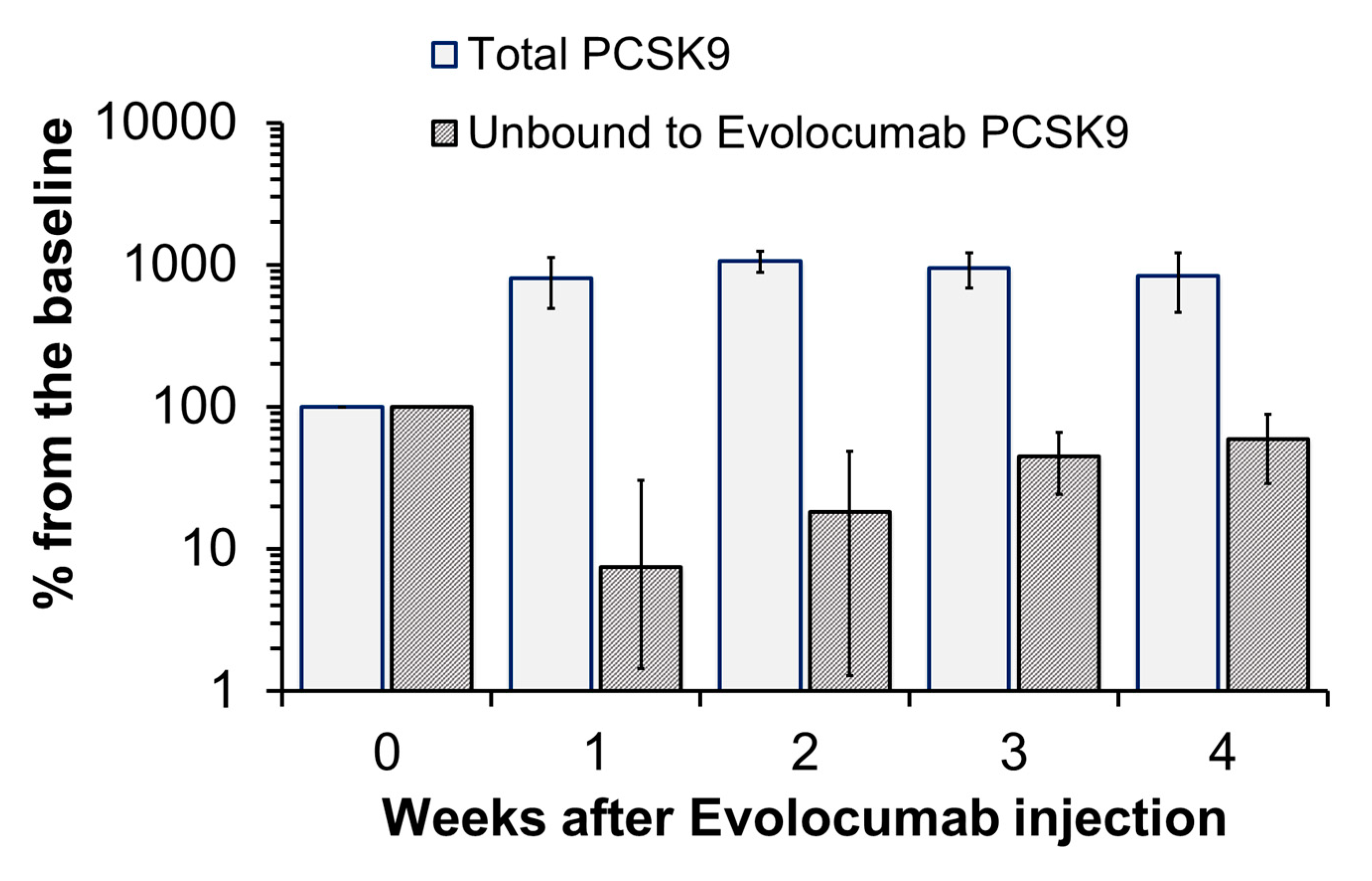
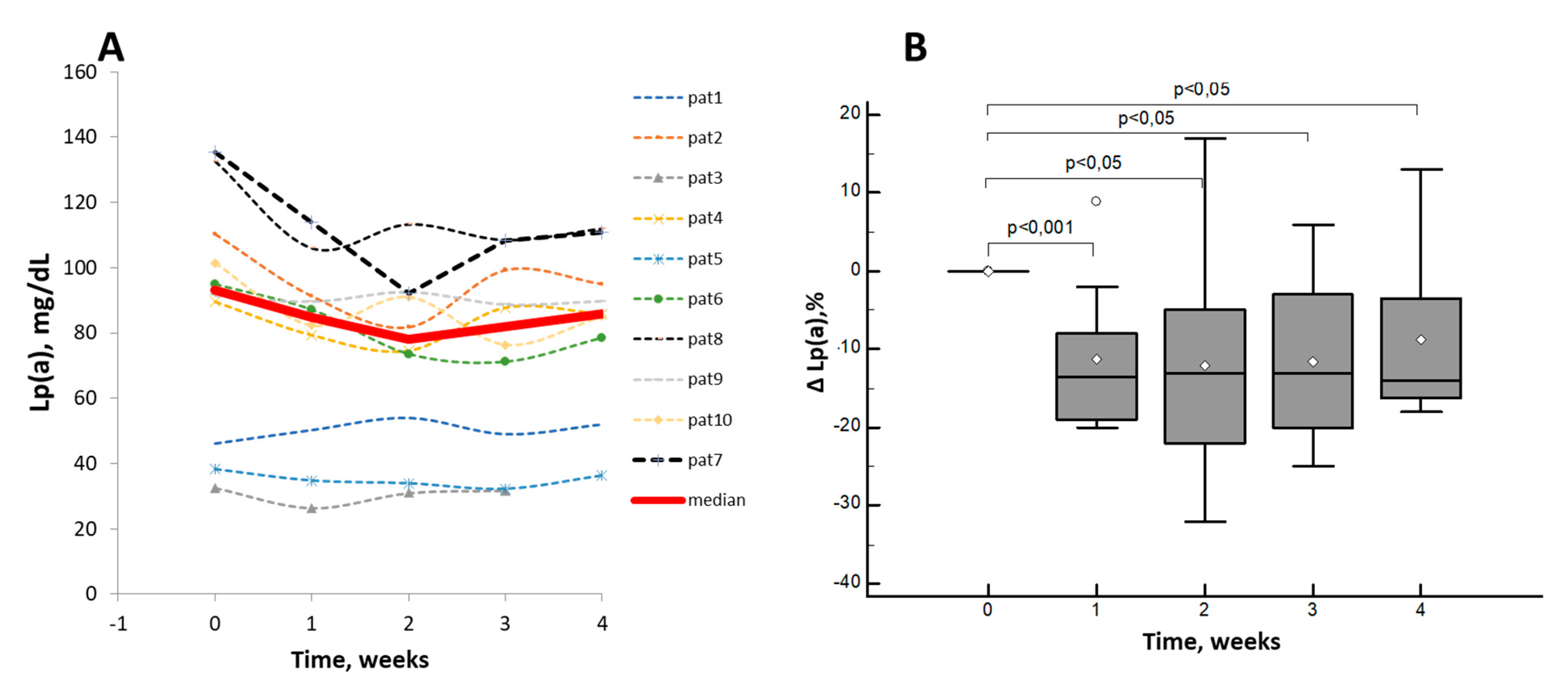
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kronenberg, F. Human Genetics and the Causal Role of Lipoprotein(a) for Various Diseases. Cardiovasc. Drugs Ther. 2016, 30, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Greco, M.F.; Sirtori, C.R.; Corsini, A.; Ezhov, M.V.; Sampietro, T.; Ruscica, M. Lipoprotein(a) Lowering—From Lipoprotein Apheresis to Antisense Oligonucleotide Approach. J. Clin. Med. 2020, 9, 2103. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.-X.; Liu, H.-H.; Sun, D.; Jin, J.-L.; Xu, R.-X.; Guo, Y.-L.; Wu, N.-Q.; Zhu, C.-G.; Li, S.; Zhang, Y.; et al. The different relations of PCSK9 and Lp(a) to the presence and severity of atherosclerotic lesions in patients with familial hypercholesterolemia. Atherosclerosis 2018, 277, 7–14. [Google Scholar] [CrossRef]
- Sabatine, M.S.; Giugliano, R.P. Low-Density Lipoprotein Cholesterol Treatment in the Proprotein Convertase Subtilisin/Kexin Type 9 Inhibitor Era. JAMA Cardiol. 2017, 2, 935–936. [Google Scholar] [CrossRef] [PubMed]
- Afanasieva, O.I.; Ezhov, M.V.; Pokrovsky, S.N. Antisense oligonucleotides and therapeutic monoclonal antibodies as a basement for novel biological lipid lowering drugs. Russ. J. Cardiol. 2018, 23, 99–109. (In Russian) [Google Scholar] [CrossRef]
- Sahebkar, A.; Watts, G.F. New Therapies Targeting apoB Metabolism for High-Risk Patients with Inherited Dyslipidaemias: What Can the Clinician Expect? Cardiovasc. Drugs Ther. 2013, 27, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Raal, F.J.; Giugliano, R.P.; Sabatine, M.S.; Koren, M.J.; Blom, D.; Seidah, N.G.; Honarpour, N.; Lira, A.; Xue, A.; Chiruvolu, P.; et al. PCSK9 inhibition-mediated reduction in Lp(a) with evolocumab: An analysis of 10 clinical trials and the LDL receptor’s role[S]. J. Lipid Res. 2016, 57, 1086–1096. [Google Scholar] [CrossRef]
- Kostner, K.M.; Kostner, G.M.; Wierzbicki, A.S. Is Lp(a) ready for prime time use in the clinic? A pros-and-cons debate. Atherosclerosis 2018, 274, 16–22. [Google Scholar] [CrossRef]
- Reyes-Soffer, G.; Ginsberg, H.N.; Ramakrishnan, R. The metabolism of lipoprotein (a): An ever-evolving story. J. Lipid Res. 2017, 58, 1756–1764. [Google Scholar] [CrossRef]
- Hoover-Plow, J.; Huang, M. Lipoprotein(a) metabolism: Potential sites for therapeutic targets. Metabolism 2013, 62, 479–491. [Google Scholar] [CrossRef]
- I Afanas’Eva, O.; Adamova, I.I.; Benevolenskaia, G.F.; Pokrovskiĭ, S.N. [An immunoenzyme method for determining lipoprotein(a)]. Biulleten’ eksperimental’noi Boil. i meditsiny 1995, 120, 398–401. [Google Scholar]
- Dahlen, G.H. Incidence of Lp(a) among populations. In Lipoprotein(a); Scanu, A.M., Ed.; Academic Press: New York, NY, USA, 1990; pp. 151–173. [Google Scholar]
- Afanasieva, O.I.; Ezhov, M.V.; Razova, O.A.; Afanasieva, M.I.; Utkina, E.A.; Pokrovsky, S.N. Apolipoprotein(a) phenotype determines the correlations of lipoprotein(a) and proprotein convertase subtilisin/kexin type 9 levels in patients with potential familial hypercholesterolemia. Atherosclerosis 2018, 277, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Samarghandi, A.; Zhang, N.; Yao, Z.; Xiong, M.; Teng, B.-B. Proprotein Convertase Subtilisin/Kexin Type 9 Interacts With Apolipoprotein B and Prevents Its Intracellular Degradation, Irrespective of the Low-Density Lipoprotein Receptor. Arter. Thromb. Vasc. Biol. 2012, 32, 1585–1595. [Google Scholar] [CrossRef] [PubMed]
- Tavori, H.; Fan, D.; Blakemore, J.L.; Yancey, P.G.; Ding, L.; Linton, M.F.; Fazio, S. Serum Proprotein Convertase Subtilisin/Kexin Type 9 and Cell Surface Low-Density Lipoprotein Receptor. Circulation 2013, 127, 2403–2413. [Google Scholar] [CrossRef]
- Levy, E.; Ouadda, A.B.D.; Spahis, S.; Sané, A.T.; Garofalo, C.; Grenier, E.; Emonnot, L.; Yara, S.; Couture, P.; Beaulieu, J.-F.; et al. PCSK9 plays a significant role in cholesterol homeostasis and lipid transport in intestinal epithelial cells. Atherosclerosis 2013, 227, 297–306. [Google Scholar] [CrossRef]
- Sun, H.; Krauss, R.M.; Chang, J.T.; Teng, B.-B. PCSK9 deficiency reduces atherosclerosis, apolipoprotein B secretion, and endothelial dysfunction. J. Lipid Res. 2018, 59, 207–223. [Google Scholar] [CrossRef]
- Raal, F.J.; Honarpour, N.; Blom, D.J.; Hovingh, G.K.; Xu, F.; Scott, R.; Wasserman, S.M.; Stein, E.A. Inhibition of PCSK9 with evolocumab in homozygous familial hypercholesterolaemia (TESLA Part B): A randomised, double-blind, placebo-controlled trial. Lancet 2015, 385, 341–350. [Google Scholar] [CrossRef]
- Cain, W.J.; Millar, J.S.; Himebauch, A.S.; Tietge, U.J.F.; Maugeais, C.; Usher, D.; Rader, D.J. Lipoprotein [a] is cleared from the plasma primarily by the liver in a process mediated by apolipoprotein [a]. J. Lipid Res. 2005, 46, 2681–2691. [Google Scholar] [CrossRef]
- Sharma, M.; Redpath, G.M.; Williams, M.J.; McCormick, S.P. Recycling of Apolipoprotein(a) After PlgRKT-Mediated Endocytosis of Lipoprotein(a). Circ. Res. 2017, 120, 1091–1102. [Google Scholar] [CrossRef]
- Rader, D.J.; A Mann, W.; Cain, W.; Kraft, H.G.; Usher, D.; A Zech, L.; Hoeg, J.M.; Davignon, J.; Lupien, P.; Grossman, M. The low density lipoprotein receptor is not required for normal catabolism of Lp(a) in humans. J. Clin. Investig. 1995, 95, 1403–1408. [Google Scholar] [CrossRef]
- Krempler, F.; Kostner, G.M.; Roscher, A.; Haslauer, F.; Bolzano, K.; Sandhofer, F. Studies on the role of specific cell surface receptors in the removal of lipoprotein (a) in man. J. Clin. Investig. 1983, 71, 1431–1441. [Google Scholar] [CrossRef] [PubMed]
- Romagnuolo, R.; Scipione, C.; Marcovina, S.M.; Gemin, M.; Seidah, N.G.; Boffa, M.B.; Koschinsky, M.L. Roles of the low density lipoprotein receptor and related receptors in inhibition of lipoprotein(a) internalization by proprotein convertase subtilisin/kexin type 9. PLoS ONE 2017, 12, e0180869. [Google Scholar] [CrossRef]
- McCormick, S.P.; Schneider, W.J. Lipoprotein(a) catabolism: A case of multiple receptors. Pathology 2019, 51, 155–164. [Google Scholar] [CrossRef]
- Canuel, M.; Sun, X.; Asselin, M.-C.; Paramithiotis, E.; Prat, A.; Seidah, N.G. Proprotein Convertase Subtilisin/Kexin Type 9 (PCSK9) Can Mediate Degradation of the Low Density Lipoprotein Receptor-Related Protein 1 (LRP-1). PLoS ONE 2013, 8, e64145. [Google Scholar] [CrossRef]
- Villard, E.F.; Thedrez, A.; Blankenstein, J.; Croyal, M.; Tran, T.-T.-T.; Poirier, B.; Le Bail, J.-C.; Illiano, S.; Nobécourt, E.; Krempf, M.; et al. PCSK9 Modulates the Secretion But Not the Cellular Uptake of Lipoprotein(a) Ex Vivo. JACC: Basic Transl. Sci. 2016, 1, 419–427. [Google Scholar] [CrossRef]
- Croyal, M.; Tran, T.-T.-T.; Blanchard, R.H.; Le Bail, J.-C.; Villard, E.F.; Poirier, B.; Aguesse, A.; Billon-Crossouard, S.; Ramin-Mangata, S.; Blanchard, V.; et al. PCSK9 inhibition with alirocumab reduces lipoprotein(a) levels in nonhuman primates by lowering apolipoprotein(a) production rate. Clin. Sci. 2018, 132, 1075–1083. [Google Scholar] [CrossRef]
- Shapiro, M.D.; Fazio, S. From Lipids to Inflammation. Circ. Res. 2016, 118, 732–749. [Google Scholar] [CrossRef] [PubMed]
- Tavori, H.; Christian, D.C.; Minnier, J.; Plubell, D.L.; Shapiro, M.D.; Yeang, C.; Giunzioni, I.; Croyal, M.; Duell, P.B.; Lambert, G.; et al. PCSK9 Association with Lipoprotein(a). Circ. Res. 2016, 119, 29–35. [Google Scholar] [CrossRef]
- Razova, O.A.; Afanas’eva, O.I.; Egiazaryan, M.G.; Sherstyuk, E.E.; Klesareva, E.A.; Pokrovskii, S.N. Circulating Complex of Lipoprotein(a) and Proprotein Convertase Subtilisin/Kexin Type 9 in the Serum Measured by ELISA. Bull. Exp. Biol. Med. 2020, 169, 639–643. [Google Scholar] [CrossRef] [PubMed]
- Viney, N.J.; Yeang, C.; Yang, X.; Xia, S.; Witztum, J.L.; Tsimikas, S. Relationship between “LDL-C”, estimated true LDL-C, apolipoprotein B-100, and PCSK9 levels following lipoprotein(a) lowering with an antisense oligonucleotide. J. Clin. Lipidol. 2018, 12, 702–710. [Google Scholar] [CrossRef]
- O’Donoghue, M.L.; Fazio, S.; Giugliano, R.P.; Stroes, E.S.; Kanevsky, E.; Gouni-Berthold, I.; Im, K.; Pineda, A.L.; Wasserman, S.M.; Češka, R.; et al. Lipoprotein(a), PCSK9 Inhibition, and Cardiovascular Risk. Circulation 2019, 139, 1483–1492. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Time (Week) | ||||
|---|---|---|---|---|---|
| Baseline 0 Week | 1st | 2nd | 3rd | 4th | |
| TC, mmol/L | 4.54 [3.70;4.98] | 3.30 [2.89;4.54] | 3.77 [3.01;4,28] a | 3.92 [3.57;4.40] | 4.45 [3.90;4.81] |
| LDL-C, mmol/L | 3.47 [2,70;3,79] | 2.47 [1.66;3.17] a | 2.27 [2.10;2.70] a | 2.23 [2.07;2.87] a | 2.75 [2.57;3.22] |
| LDL-Ccorr, mmol/L | 2.60 [2,0;3,2] | 1.95 [1.30;2.50] a | 1.70 [1.50;2.00] a | 1.90 [1.25;2.07] | 2.30 [1.65; 2.48] |
| TG, mmol/L | 0.84 [0.58;0.98] | 0.72 [0.63;0.89] | 0.78 [0.69;1.05] | 0.73 [0.67;80.93] | 0.90 [0.54;1.30] |
| HDL, mmol/L | 0.99 [0.73;1.25] | 1.03 [0.94; 1.45] | 1.14 [0.91;1.19] | 1.22 [1.10;1.29] | 1.35 [0.79;1.93] |
| Lp(a), mg/dL | 93.14 [46.10;110.40] | 84.70 [50.20;91.30] a | 78.15 [54.00;92.10] a | 82.05 [49.00;99.30] a | 85.80 [71.78;99.00] a |
| PCSK9, unbound, ng/mL | 710 [520;1062] | 0 [0;0] a | 0 [0;13] b | 450 [190;503] a | 341 [142;504] a |
| Total pool of PCSK9, ng/mL | 496 [369;719] | 3944 [3132;4629] a | 5916 [3694;7332] a | 5175 [3621;5832] a | 3895 [3442;3964] a |
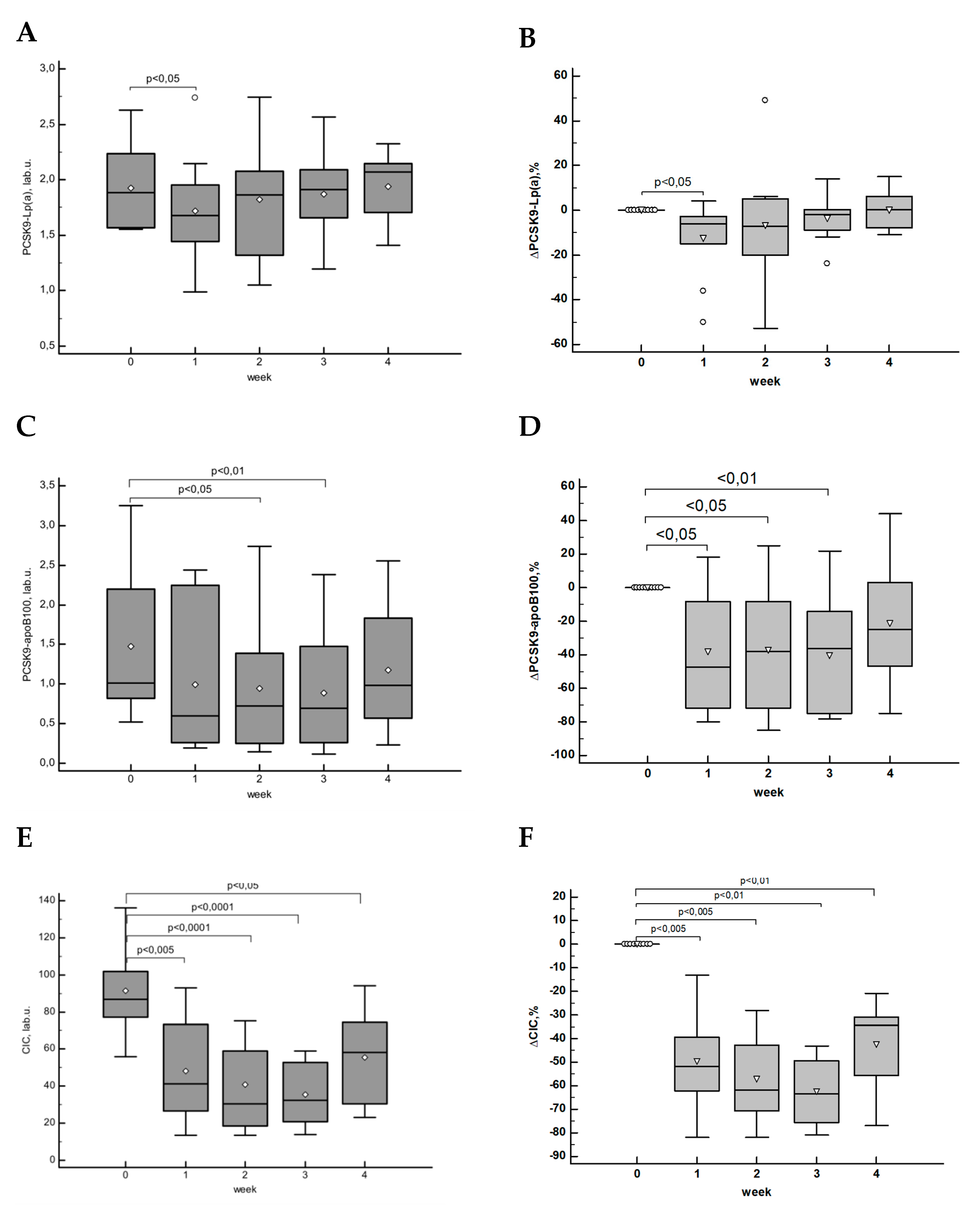
| [PCSK9-apoB], lab.u. | 1.01 [0.82;2.20] | 0.60 [0.25;2.24] | 0.73 [0.25;1.39] a | 0.69 [0.26;1.48] a | 0.98 [0.57;1.83] |
| [PCSK9-Lp(a)], lab.u. | 1.89 [1.57;2.23] | 1.68 [1.44;1.95] a | 1.86 [1.32;2.08] | 1.91 [1.66;2.09] | 2.07 [1.70;2.14] |
| IgG, g/L | 10.83 [9.24;12.03] | 9.93 [8.30;12.04] | 9.71 [8.56;13.12] | 10.36 [9.41;12.04] | 9.62 [8.51;11.62] |
| IgM, g/L | 0.83 [0.67;1.12] | 0.76 [0.58;1.07] | 0.64 [0.58;1.25] | 0.68 [0.54;0.93] | 0.59 [0.52;1.13] |
| CIC, lab.u | 86.80 [77.05;102.00] | 41.30 [26.45;73.22] b | 30.40 [18.37;59.03] b | 32.25 [20.70;52.75] a | 58.10 [30.50;74.60] a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afanasieva, O.; Ezhov, M.V.; Klesareva, E.; Razova, O.; Chubykina, U.; Egiazaryan, M.; Sherstyuk, E.; Afanasieva, M.; Utkina, E.; Pokrovsky, S. Effect of Evolocumab on Lipoprotein(a) and PCSK9 in Healthy Individuals with Elevated Lipoprotein(a) Level. J. Cardiovasc. Dev. Dis. 2020, 7, 45. https://doi.org/10.3390/jcdd7040045
Afanasieva O, Ezhov MV, Klesareva E, Razova O, Chubykina U, Egiazaryan M, Sherstyuk E, Afanasieva M, Utkina E, Pokrovsky S. Effect of Evolocumab on Lipoprotein(a) and PCSK9 in Healthy Individuals with Elevated Lipoprotein(a) Level. Journal of Cardiovascular Development and Disease. 2020; 7(4):45. https://doi.org/10.3390/jcdd7040045
Chicago/Turabian StyleAfanasieva, Olga, Marat V. Ezhov, Elena Klesareva, Oksana Razova, Uliana Chubykina, Mane Egiazaryan, Ekaterina Sherstyuk, Marina Afanasieva, Elena Utkina, and Sergei Pokrovsky. 2020. "Effect of Evolocumab on Lipoprotein(a) and PCSK9 in Healthy Individuals with Elevated Lipoprotein(a) Level" Journal of Cardiovascular Development and Disease 7, no. 4: 45. https://doi.org/10.3390/jcdd7040045
APA StyleAfanasieva, O., Ezhov, M. V., Klesareva, E., Razova, O., Chubykina, U., Egiazaryan, M., Sherstyuk, E., Afanasieva, M., Utkina, E., & Pokrovsky, S. (2020). Effect of Evolocumab on Lipoprotein(a) and PCSK9 in Healthy Individuals with Elevated Lipoprotein(a) Level. Journal of Cardiovascular Development and Disease, 7(4), 45. https://doi.org/10.3390/jcdd7040045







