Impact of the 2019 European Guidelines on Diabetes in Clinical Practice: Real and Simulated Analyses of Lipid Goals
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cholesterol Treatment Trialists’ (CTT) Collaborators; Mihaylova, B.; Emberson, J.; Blackwell, L.; Keech, A.; Simes, J.; Barnes, E.H.; Voysey, M.; Gray, A.; Collins, R.; et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: Meta-analysis of individual data from 27 randomised trials. Lancet 2012, 380, 581–590. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/AphA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2018, 139, 1082–1143. [Google Scholar]
- de Cardiología, S.A.; Normas, Á.D.C.Y.; Sociedad Argentina de Cardiología. Uso apropiado de estatinas en Argentina. Documento de Posición. Rev. Arg. Cardiol. 2018, 86, 1–13. [Google Scholar]
- Breuker, C.; Clement, F.; Mura, T.; Macioce, V.; Castet-Nicolas, A.; Audurier, Y.; Boegner, C.; Morcrette, E.; Jalabert, A.; Villiet, M.; et al. Non-achievement of LDL-cholesterol targets in patients with diabetes at very-high cardiovascular risk receiving statin treatment: Incidence and risk factors. Int. J. Cardiol. 2018, 268, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Gyberg, V.; De Bacquer, D.; De Backer, G.; Jennings, C.; Kotseva, K.; Mellbin, L.; Schnell, O.; Tuomilehto, J.; Wood, D.; Rydén, L.; et al. Patients with coronary artery disease and diabetes need improved management: A report from the EUROASPIRE IV survey: A registry from the EuroObservational Research Programme of the European Society of Cardiology. Cardiovasc. Diabetol. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giugliano, R.P.; Cannon, C.P.; Blazing, M.A.; Nicolau, J.C.; Corbalán, R.; Špinar, J.; Park, J.-G.; White, J.A.; Bohula, E.A.; Braunwald, E. Benefit of Adding Ezetimibe to Statin Therapy on Cardiovascular Outcomes and Safety in Patients With Versus Without Diabetes Mellitus. Circulation 2018, 137, 1571–1582. [Google Scholar] [CrossRef] [PubMed]
- Sabatine, M.S.; Leiter, L.A.; Wiviott, S.D.; Giugliano, R.P.; Deedwania, P.; De Ferrari, G.M.; Murphy, S.A.; Kuder, J.F.; Gouni-Berthold, I.; Lewis, B.S.; et al. Cardiovascular safety and efficacy of the PCSK9 inhibitor evolocumab in patients with and without diabetes and the effect of evolocumab on glycaemia and risk of new-onset diabetes: A prespecified analysis of the FOURIER randomised controlled trial. Lancet Diabetes Endocrinol. 2017, 5, 941–950. [Google Scholar] [CrossRef]
- Ray, K.K.; Colhoun, H.M.; Szarek, M.; Baccara-Dinet, M.; Bhatt, D.L.; Bittner, V.A.; Budaj, A.J.; Diaz, R.; Goodman, S.G.; Hanotin, C.; et al. Effects of alirocumab on cardiovascular and metabolic outcomes after acute coronary syndrome in patients with or without diabetes: A prespecified analysis of the ODYSSEY OUTCOMES randomised controlled trial. Lancet Diabetes Endocrinol. 2019, 7, 618–628. [Google Scholar] [CrossRef] [Green Version]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2019, 41, 255–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gencer, B.; Koskinas, K.C.; Räber, L.; Karagiannis, A.; Nanchen, D.; Auer, R.; Carballo, D.; Carballo, S.; Klingenberg, R.; Heg, D.; et al. Eligibility for PCSK9 Inhibitors According to American College of Cardiology (ACC) and European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) Guidelines After Acute Coronary Syndromes. J. Am. Heart Assoc. 2017. [Google Scholar] [CrossRef] [Green Version]
- Taskinen, M.-R.; Borén, J. New insights into the pathophysiology of dyslipidemia in type 2 diabetes. Atherosclerosis 2015, 239, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Comaschi, M.; Coscelli, C.; Cucinotta, M.; Malini, P.; Manzato, E.; Nicolucci, A. Cardiovascular risk factors and metabolic control in type 2 diabetic subjects attending outpatient clinics in Italy: The SFIDA (survey of risk factors in Italian diabetic subjects by AMD) study. Nutr. Metab. Cardiovasc. Dis. 2005, 15, 204–211. [Google Scholar] [CrossRef] [PubMed]
- März, W.; Dippel, F.-W.; Theobald, K.; Gorcyca, K.; Iorga, Ş.R.; Ansell, D. Utilization of lipid-modifying therapy and low-density lipoprotein cholesterol goal attainment in patients at high and very-high cardiovascular risk: Real-world evidence from Germany. Atherosclerosis 2018, 268, 99–107. [Google Scholar]
- Malik, S.; López, V.; Chen, R.; Wu, W.; Wong, N.D. Undertreatment of cardiovascular risk factors among persons with diabetes in the United States. Diabetes Res. Clin. Pr. 2007, 77, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.; Liu, S.; Krousel-Wood, M.; Shao, H.; Fonseca, V.; Shi, L. Long-term outcomes associated with triple-goal achievement in patients with type 2 diabetes mellitus (T2DM). Diabetes Res. Clin. Pract. 2018, 140, 45–54. [Google Scholar] [CrossRef]
- Zhang, X.; Ji, L.; Ran, X.; Su, B.; Ji, Q.; Hu, D. Gender Disparities in Lipid Goal Attainment among Type 2 Diabetes Outpatients with Coronary Heart Disease: Results from the CCMR-3B Study. Sci. Rep. 2017. [Google Scholar] [CrossRef] [Green Version]
- Al-Zakwani, I.; Al-Mahruqi, F.; Al-Rasadi, K.; Shehab, A.; Al Mahmeed, W.; Arafah, M.; Al-Hinai, A.T.; Al Tamimi, O.; Al Awadhi, M.; Santos, R.D. Sex disparity in the management and outcomes of dyslipidemia of diabetic patients in the Arabian Gulf: Findings from the CEPHEUS study. Lipids Health Dis. 2018. [Google Scholar] [CrossRef] [Green Version]
- Moreno-Arellano, S.; De-Mendoza, J.D.-; Santi-Cano, M. Sex disparity persists in the prevention of cardiovascular disease in women on statin therapy compared to that in men. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 810–815. [Google Scholar] [CrossRef]
- Lin, I.; Sung, J.; Sanchez, R.J.; Mallya, U.G.; Friedman, M.; Panaccio, M.; Koren, A.; Neumann, P.; Menzin, J. Patterns of Statin Use in a Real-World Population of Patients at High Cardiovascular Risk. J. Manag. Care Spéc. Pharm. 2016, 22, 685–698. [Google Scholar] [CrossRef]
- Ziemer, D.C.; Miller, C.D.; Rhee, M.K.; Doyle, J.P.; Watkins, C.; Cook, C.B.; Gallina, D.L.; El-Kebbi, I.M.; Barnes, C.S.; Dunbar, V.G.; et al. Clinical Inertia Contributes to Poor Diabetes Control in a Primary Care Setting. Diabetes Educ. 2005, 31, 564–571. [Google Scholar] [CrossRef]
- García Díaz, E.; Ramírez Medina, D.; Morera Porras, Ó.M.; Cabrera Mateos, J.L. Determinants of inertia with lipid-lowering treatment in patients with type 2 diabetes mellitus. Endocrinol. Diabetes Nutr. 2019, 66, 223–231. [Google Scholar]
- Masson, W.; Lobo, M.; Manente, D.; Vitagliano, L.; Rostán, M.; Siniawski, D.; Huerín, M.; Giorgi, M. Respuesta a las estatinas en prevención cardiovascular. Evaluación de los hiporrespondedores. Rev. Argent. Cardiol. 2014, 82, 34–41. [Google Scholar] [CrossRef]
- Rallidis, L.S.; Triantafyllis, A.S.; Iliodromitis, E. Eligibility for treatment with PCSK9 inhibitors among patients with stable coronary artery disease presumed to be on maximum hypolipidaemic therapy. Hell. J. Cardiol. 2018, 59, 293–295. [Google Scholar] [CrossRef] [PubMed]
- Landmesser, U.; Chapman, M.J.; Stock, J.K.; Amarenco, P.; Belch, J.J.F.; Borén, J.; Farnier, M.; Ference, B.A.; Gielen, S.; Graham, I.; et al. 2017 Update of ESC/EAS Task Force on practical clinical guidance for proprotein convertase subtilisin/kexin type 9 inhibition in patients with atherosclerotic cardiovascular disease or in familial hypercholesterolaemia. Eur. Heart J. 2017, 39, 1131–1143. [Google Scholar] [CrossRef] [Green Version]
- McEwen, L.N.; Casagrande, S.S.; Kuo, S.; Herman, W.H. Why Are Diabetes Medications So Expensive and What Can Be Done to Control Their Cost? Curr. Diabetes Rep. 2017. [Google Scholar] [CrossRef]
- Soppi, A.; Heino, P.; Kurko, T.; Maljanen, T.; Saastamoinen, L.; Aaltonen, K. Growth of diabetes drug expenditure decomposed-A nationwide analysis. Health Policy 2018, 122, 1326–1332. [Google Scholar] [CrossRef]
| Continuous Variables * | N = 528 |
|---|---|
| Age, years | 62.1 ± 12.7 |
| Diabetes time, years | 5.5 (3.0–12.0) |
| Body mass index, kg/m2 | 31.4 ± 5.6 |
| Creatinine, mg/dL | 1.0 ± 0.4 |
| Blood glucose, mg/dL | 129.2 (110.5−151.5) |
| Glycated hemoglobin (HbA1c), % (mmol/mol) | 7.1 (54) ±1.3 |
| Total cholesterol, mg/dL | 171.8 ± 43.4 |
| LDL-C, mg/dL | 95.8 ± 38.5 |
| HDL-C, mg/dL | 43.9 ± 12.4 |
| Triglycerides, mg/dL | 139.0 (100.0–189.0) |
| Non-HDL-C, mg/dL | 127.9 ± 41.7 |
| Systolic blood pressure, mmHg | 128.7 ± 14.1 |
| Diastolic blood pressure, mmHg | 77.9 ± 10.2 |
| Waist circumference, cm | 106.0 ± 13.7 |
| Categorical variables, % | |
| Male gender | 64.0 |
| Current smoking | 10.0 |
| Hypertension | 70.3 |
| Family history of early cardiovascular disease | 11.2 |
| Retinopathy | 4.4 |
| Neuropathy | 5.7 |
| Microalbuminuria | 27.6 |
| Obesity | 55.7 |
| Secondary prevention | 37.3 |
| Treatment, % | n (%) |
|---|---|
| Aspirin | 196 (37.1) |
| ACE inhibitors/angiotensin antagonists | 336 (63.6) |
| β-adrenergic blockers | 194 (36.7) |
| Calcium channel blockers | 103 (19.5) |
| Diuretics | 110 (20.8) |
| Biguanides (Metformin) | 416 (78.8) |
| Sulfonylureas | 53 (10.1) |
| Thiazolidinediones | 11 (2.1) |
| Dipeptidyl peptidase-4 inhibitors | 133 (25.2) |
| Glucagon-like peptide-1 receptor agonists | 38 (7.2) |
| Sodium–glucose cotransporter-2 inhibitors | 44 (8.3) |
| Atorvastatin | 127 (24.1) |
| 5 mg/day | 2 (1.5) |
| 10 mg/day | 62 (47.7) |
| 20 mg/day | 42 (32.3) |
| 40 mg/day | 20 (15.4) |
| 80 mg/day | 4 (3.1) |
| Rosuvastatin | 183 (34.6) |
| 5 mg/day | 30 (16.4) |
| 10 mg/day | 95 (51.9) |
| 20 mg/day | 53 (29.0) |
| 40 mg/day | 5 (2.7) |
| Simvastatin | 20 (3.8) |
| 10 mg/day | 9 (47.4) |
| 20 mg/day | 10 (52.6) |
| Fluvastatin 80 mg/day | 3 (0.6) |
| Ezetimibe | 50 (9.5) |
| Fibrates | 56 (10.6) |
| Omega 3 | 20 (3.8) |
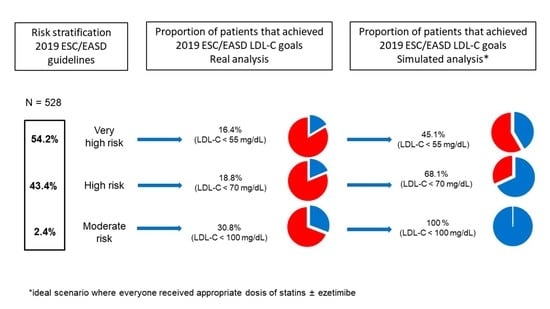
| Lipid Goals | Moderate Risk n = 13 n (%) | High Risk n = 229 n (%) | Very High Risk n = 286 n (%) |
|---|---|---|---|
| LDL-C < 55 mg/dL | 47 (16.4) | ||
| Non-HDL-C < 85 mg/dL | 56 (19.6) | ||
| LDL-C < 70 mg/dL | 43(18.8) | ||
| Non-HDL-C < 100 mg/dL | 42 (18.3) | ||
| LDL-C < 100 mg/dL | 4 (30.8%) | ||
| Non-HDL-C < 130 mg/dL | 6 (46.2%) |
| Statin Doses | Moderate Risk n = 13 n (%) | High Risk n = 229 n (%) | Very High Risk n = 286 n (%) |
|---|---|---|---|
| High intensity | 0 | 25 (10.9) | 61 (21.3) |
| Moderate intensity | 2 (15.4) | 93 (40.6) | 146 (51.1) |
| Low intensity | 0 | 4 (1.8) | 5 (1.7) |
| Without statins | 11 (84.6) | 107 (46.7) | 74 (25.9) |
| Lipid Goals | Moderate Risk n = 13 n (%) | High Risk n = 229 n (%) | Very High Risk n = 286 n (%) |
|---|---|---|---|
| Adding statins at appropriate doses | |||
| LDL-C < 55 mg/dL | 100 (35.5) | ||
| Non-HDL-C < 85 mg/dL | 103 (36.0) | ||
| LDL-C < 70 mg/dL | 130 (56.8) | ||
| Non-HDL-C < 100 mg/dL | 132 (57.2) | ||
| LDL-C < 100 mg/dL | 13 (100) | ||
| Non-HDL-C < 130 mg/dL | 13 (100) | ||
| Adding ezetimibe | |||
| LDL-C < 55 mg/dL | 129 (45.1) | ||
| Non-HDL-C < 85 mg/dL | 148 (51.8) | ||
| LDL-C < 70 mg/dL | 156 (68.1) | ||
| Non-HDL-C < 100mg/dL | 168 (73.2) | ||
| LDL-C < 100 mg/dL | not applicable | ||
| Non-HDL-C < 130 mg/dL | not applicable |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masson, W.; Huerín, M.; Lobo, L.M.; Masson, G.; Molinero, G.; Nemec, M.; Boccadoro, M.; Romero, C.; Micali, G.; Siniawski, D. Impact of the 2019 European Guidelines on Diabetes in Clinical Practice: Real and Simulated Analyses of Lipid Goals. J. Cardiovasc. Dev. Dis. 2020, 7, 6. https://doi.org/10.3390/jcdd7010006
Masson W, Huerín M, Lobo LM, Masson G, Molinero G, Nemec M, Boccadoro M, Romero C, Micali G, Siniawski D. Impact of the 2019 European Guidelines on Diabetes in Clinical Practice: Real and Simulated Analyses of Lipid Goals. Journal of Cardiovascular Development and Disease. 2020; 7(1):6. https://doi.org/10.3390/jcdd7010006
Chicago/Turabian StyleMasson, Walter, Melina Huerín, Lorenzo Martin Lobo, Gerardo Masson, Graciela Molinero, Mariano Nemec, Mariela Boccadoro, Cinthia Romero, Gabriel Micali, and Daniel Siniawski. 2020. "Impact of the 2019 European Guidelines on Diabetes in Clinical Practice: Real and Simulated Analyses of Lipid Goals" Journal of Cardiovascular Development and Disease 7, no. 1: 6. https://doi.org/10.3390/jcdd7010006
APA StyleMasson, W., Huerín, M., Lobo, L. M., Masson, G., Molinero, G., Nemec, M., Boccadoro, M., Romero, C., Micali, G., & Siniawski, D. (2020). Impact of the 2019 European Guidelines on Diabetes in Clinical Practice: Real and Simulated Analyses of Lipid Goals. Journal of Cardiovascular Development and Disease, 7(1), 6. https://doi.org/10.3390/jcdd7010006