Cerebral and Spinal Cord Protection Strategies in Aortic Arch Surgery
Abstract
1. Introduction
2. Cerebral Neuroprotection for Aortic Arch Surgery
3. Spinal Cord Protection for Aortic Arch Surgery
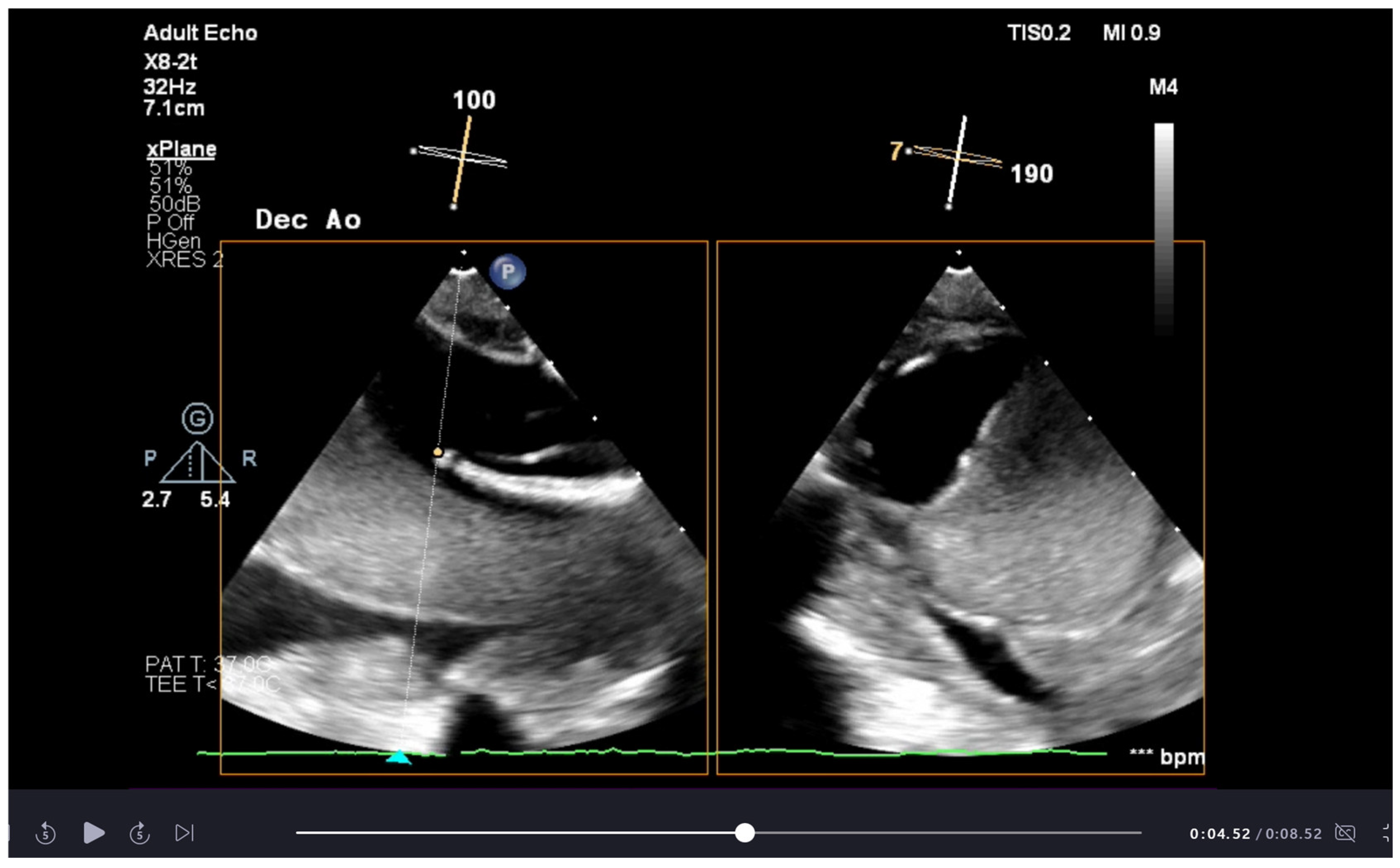
4. Additional Monitoring for Aortic Arch Surgery
5. Postoperative Management—Prevention and Treatment of Delayed SCI
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sanphasitvong, V.; Wongkornrat, W.; Jantarawan, T.; Khongchu, N.; Slisatkorn, W. Mortality and complications following total aortic arch replacement: 14 years’ experience. Asian Cardiovasc. Thorac. Ann. 2022, 30, 679–687. [Google Scholar] [CrossRef] [PubMed]
- Preventza, O.; Liao, J.L.; Olive, J.K.; Simpson, K.; Critsinels, A.C.; Price, M.D.; Galati, M.; Cornwall, L.D.; Orozco-Sevilla, V.; Omer, S.; et al. Neurologic complications after the frozen elephant trunk procedure: A meta-analysis of more than 3000 patients. J. Thorac. Cardiovasc. Surg. 2020, 160, 20–33.e4. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, M.; Kaufeld, T.; Beckmann, E.; Fleissner, F.; Umminger, J.; Abd Alhadi, F.; Boethig, D.; Krueger, H.; Haverich, A.; Martens, A. Total aortic arch replacement with a novel 4-branched frozen elephant trunk prosthesis: Single-center results of the first 100 patients. J. Thorac. Cardiovasc. Surg. 2016, 152, 148–159.e1. [Google Scholar] [CrossRef]
- Borst, H.G.; Walterbusch, G.; Schaps, D. Extensive aortic replacement using “elephant trunk” prosthesis. Thorac. Cardiovasc. Surg. 1983, 31, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Damberg, A.; Carino, D.; Charilaou, P.; Peterss, S.; Tranquilli, M.; Ziganshin, B.A.; Rizzo, J.A.; Elefteriades, J.A. Favorable late survival after aortic surgery under straight deep hypothermic circulatory arrest. J. Thorac. Cardiovasc. Surg. 2017, 154, 1831–1839.e1. [Google Scholar] [CrossRef]
- Gutsche, J.T.; Ghadimi, K.; Patel, P.A.; Robinson, A.R., 3rd; Lane, B.J.; Szeto, W.Y.; Augoustides, J.G. New Frontiers in Aortic Therapy: Focus on Deep Hypothermic Circulatory Arrest. J. Cardiothorac. Vasc. Anesth. 2014, 28, 1159–1163. [Google Scholar] [CrossRef]
- Pupovac, S.S.; Hemli, J.M.; Giammarino, A.T.; Varrone, M.; Aminov, A.; Scheinerman, S.J.; Hartman, A.R.; Brinster, D.R. Deep versus moderate hypothermia in acute type A aortic dissection: A propensity-matched analysis. Heart Lung Circ. 2022, 31, 1699–1705. [Google Scholar]
- Tian, D.H.; Wan, B.; Bannon, P.G.; Misfeld, M.; LeMaire, S.A.; Kazui, T.; Kouchoukos, N.T.; Elefteriades, J.A.; Bavaria, J.; Coselli, J.S.; et al. A meta-analysis of deep hypothermic circulatory arrest versus moderate hypothermic circulatory arrest with selective antegrade cerebral perfusion. Ann. Cardiothorac. Surg. 2013, 2, 148–158. [Google Scholar] [CrossRef]
- Malvindi, P.G.; Scrascia, G.; Vitale, N. Is unilateral antegrade cerebral perfusion equivalent to bilateral cerebral perfusion for patients undergoing aortic arch surgery? Interact. Cardiovasc. Thorac. Surg. 2008, 7, 891–897. [Google Scholar] [CrossRef]
- Nouraei, S.M.; Nouraei, S.R.; Sadashiva, A.K.; Pillay, T. Subclavian Cannulation Improves Outcome of Surgery for Type a Aortic Dissection. Asian Cardiovasc. Thorac. Ann. 2007, 15, 118–122. [Google Scholar] [CrossRef]
- Abe, T.; Usui, A. The cannulation strategy in surgery for acute type A dissection. Gen. Thorac. Cardiovasc. Surg. 2017, 65, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Papantchev, V.; Stoinova, V.; Aleksandrov, A.; Todorova-Papantcheva, D.; Hristov, S.; Petkov, D.; Nachev, G.; Ovtscharoff, W. The role of Willis circle variations during unilateral selective cerebral perfusion: A study of 500 circles†. Eur. J. Cardio-Thorac. Surg. 2013, 44, 743–753. [Google Scholar] [CrossRef]
- Nordon, D.G.; Júnior, R. Variations in the Brain Circulation-the Circle of Willis. Braz. J. Morphol. Sci. 2012, 29, 243–247. [Google Scholar]
- Merkkola, P.; Tulla, H.; Ronkainen, A.; Soppi, V.; Oksala, A.; Koivisto, T.; Hippeläinen, M. Incomplete circle of Willis and right axillary artery perfusion. Ann. Thorac. Surg. 2006, 82, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Urbanski, P.P.; Lenos, A.; Kolowca, M.; Bougioukakis, P.; Keller, G.; Zacher, M.; Diegeler, A. Near-infrared spectroscopy for neuromonitoring of unilateral cerebral perfusion. Eur. J. Cardio-Thorac. Surg. 2013, 43, 1140–1144. [Google Scholar] [CrossRef]
- Brouns, R.; De Vil, B.; Cras, P.; De Surgeloose, D.; Mariën, P.; De Deyn, P.P. Neurobiochemical Markers of Brain Damage in Cerebrospinal Fluid of Acute Ischemic Stroke Patients. Clin. Chem. 2010, 56, 451–458. [Google Scholar] [CrossRef]
- Nishimura, Y.; Honda, K.; Yuzaki, M.; Kunimoto, H.; Fujimoto, T.; Agematsu, K. Bilateral Axillary Artery Perfusion in Total Arch Replacement. Ann. Thorac. Surg. 2023, 116, 35–41. [Google Scholar] [CrossRef]
- Reinsfelt, B.; Ricksten, S.E.; Zetterberg, H.; Blennow, K.; Fredén-Lindqvist, J.; Westerlind, A. Cerebrospinal fluid markers of brain injury, inflammation, and blood-brain barrier dysfunction in cardiac surgery. Ann. Thorac. Surg. 2012, 94, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Haldenwang, P.L.; Strauch, J.T.; Amann, I.; Klein, T.; Sterner-Kock, A.; Christ, H.; Wahlers, T. Impact of pump flow rate during selective cerebral perfusion on cerebral hemodynamics and metabolism. Ann. Thorac. Surg. 2010, 90, 1975–1984. [Google Scholar] [CrossRef]
- Spielvogel, D.; Kai, M.; Tang, G.H.L.; Malekan, R.; Lansman, S.L. Selective cerebral perfusion: A review of the evidence. J. Thorac. Cardiovasc. Surg. 2013, 145, S59–S62. [Google Scholar] [CrossRef]
- Liu, Y.; Jiang, H.; Wang, B.; Yang, Z.; Xia, L.; Wang, H. Efficacy of pump-controlled selective antegrade cerebral perfusion in total arch replacement: A propensity-matched analysis. Front. Surg. 2022, 9, 918461. [Google Scholar] [CrossRef] [PubMed]
- Lewis, F.J.; Taufic, M. Closure of atrial septal defects with the aid of hypothermia; experimental accomplishments and the report of one successful case. Surgery 1953, 33, 52–59. [Google Scholar]
- Griepp, R.B.; Stinson, E.B.; Hollingsworth, J.F.; Buehler, D. Prosthetic replacement of the aortic arch. J. Thorac. Cardiovasc. Surg. 1975, 70, 1051–1063. [Google Scholar]
- Manetta, F.; Mullan, C.W.; Catalano, M.A. Neuroprotective Strategies in Repair and Replacement of the Aortic Arch. Int. J. Angiol. 2018, 27, 98–109. [Google Scholar] [CrossRef]
- Stecker, M.M.; Cheung, A.T.; Pochettino, A.; Kent, G.P.; Patterson, T.; Weiss, S.J.; Bavaria, J.E. Deep hypothermic circulatory arrest: I. Effects of cooling on electroencephalogram and evoked potentials. Ann. Thorac. Surg. 2001, 71, 14–21. [Google Scholar] [CrossRef] [PubMed]
- McCullough, J.N.; Zhang, N.; Reich, D.L.; Juvonen, T.S.; Klein, J.J.; Spielvogel, D.; Ergin, M.A.; Griepp, R.B. Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann. Thorac. Surg. 1999, 67, 1895–1899. [Google Scholar] [CrossRef]
- Boening, A.; Karck, M.; Conzelmann, L.O.; Easo, J.; Krüger, T.; Rylski, B.; Weigang, E. German Registry for Acute Aortic Dissection Type A: Structure, Results, and Future Perspectives. Thorac. Cardiovasc. Surg. 2017, 65, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Gupta, P.; Harky, A.; Jahangeer, S.; Adams, B.; Bashir, M. Varying Evidence on Deep Hypothermic Circulatory Arrest in Thoracic Aortic Aneurysm Surgery. Tex. Heart Inst. J. 2018, 45, 70–75. [Google Scholar] [CrossRef]
- Leshnower, B.G.; Myung, R.J.; Chen, E.P. Aortic arch surgery using moderate hypothermia and unilateral selective antegrade cerebral perfusion. Ann. Cardiothorac. Surg. 2013, 2, 288–295. [Google Scholar] [CrossRef]
- Keenan, J.E.; Wang, H.; Gulack, B.C.; Ganapathi, A.M.; Andersen, N.D.; Englum, B.R.; Krishnamurthy, Y.; Levy, J.H.; Welsby, I.J.; Hughes, G.C. Does moderate hypothermia really carry less bleeding risk than deep hypothermia for circulatory arrest? A propensity-matched comparison in hemiarch replacement. J. Thorac. Cardiovasc. Surg. 2016, 152, 1559–1569.e2. [Google Scholar] [CrossRef]
- Englum, B.R.; Andersen, N.D.; Husain, A.M.; Mathew, J.P.; Hughes, G.C. Degree of hypothermia in aortic arch surgery—Optimal temperature for cerebral and spinal protection: Deep hypothermia remains the gold standard in the absence of randomized data. Ann. Cardiothorac. Surg. 2013, 2, 184–193. [Google Scholar] [CrossRef]
- Preventza, O.; Garcia, A.; Kashyap, S.A.; Akvan, S.; Cooley, D.A.; Simpson, K.; Rammou, A.; Price, M.D.; Omer, S.; Bakaeen, F.G.; et al. Moderate hypothermia ≥24 and ≤28 °C with hypothermic circulatory arrest for proximal aortic operations in patients with previous cardiac surgery. Eur. J. Cardio-Thorac. Surg. 2016, 50, 949–954. [Google Scholar] [CrossRef]
- Bayona, N.A.; Gelb, A.W.; Jiang, Z.; Wilson, J.X.; Urquhart, B.L.; Cechetto, D.F. Propofol Neuroprotection in Cerebral Ischemia and Its Effects on Low-molecular-weight Antioxidants and Skilled Motor Tasks. Anesthesiology 2004, 100, 1151–1159. [Google Scholar] [CrossRef]
- Head, B.P.; Patel, P. Anesthetics and brain protection. Curr. Opin. Anaesthesiol. 2007, 20, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.; Gao, S.; Lou, S.; Yu, C.; Sun, X.; Qian, X.; Ji, B. Does methylprednisolone provide protective effect in total aortic arch replacement requiring hypothermia circulatory arrest and selective cerebral perfusion? Perfusion 2023, 38, 1384–1392. [Google Scholar] [CrossRef] [PubMed]
- Abbasciano, R.G.; Olivieri, G.M.; Chubsey, R.; Gatta, F.; Tyson, N.; Easwarakumar, K.; Fudulu, D.P.; Marsico, R.; Kofler, M.; Elshafie, G.; et al. Prophylactic corticosteroids for cardiopulmonary bypass in adult cardiac surgery. Cochrane Database Syst. Rev. 2024, 3, CD005566. [Google Scholar] [CrossRef] [PubMed]
- Whitlock, R.P.; Devereaux, P.J.; Teoh, K.H.; Lamy, A.; Vincent, J.; Pogue, J.; Paparella, D.; Sessler, D.I.; Karthikeyan, G.; Villar, J.C.; et al. Methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): A randomised, double-blind, placebo-controlled trial. Lancet 2015, 386, 1243–1253. [Google Scholar] [CrossRef]
- Langley, S.M.; Chai, P.J.; Jaggers, J.J.; Ungerleider, R.M. Preoperative high dose methylprednisolone attenuates the cerebral response to deep hypothermic circulatory arrest. Eur. J. Cardiothorac. Surg. 2000, 17, 279–286. [Google Scholar] [CrossRef]
- Shum-Tim, D.; Tchervenkov, C.I.; Jamal, A.; Nimeh, T.; Juo, C.Y.; Chedrawy, E.; Laliberte, E.; Philip, A.; Rose, C.P.; Lavoie, J. Systemic steroid pretreatment improves cerebral protection after circulatory arrest. Ann. Thorac. Surg. 2001, 72, 1465–1471, discussion 1471–1472. [Google Scholar] [CrossRef]
- Krüger, T.; Hoffmann, I.; Blettner, M.; Borger, M.A.; Schlensak, C.; Weigang, E.; GERAADA Investigators. Intraoperative neuroprotective drugs without beneficial effects? Results of the German Registry for Acute Aortic Dissection Type A (GERAADA). Eur. J. Cardiothorac. Surg. 2013, 44, 939–946. [Google Scholar] [CrossRef]
- Wang, Y.; Gu, T.; Shi, E.; Yu, L.; Wang, C.; Zhang, Y.; Fang, Q. Inhibition of microRNA-29c protects the brain in a rat model of prolonged hypothermic circulatory arrest. J. Thorac. Cardiovasc. Surg. 2015, 150, 675–684.e1. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Martens, A.; Beckmann, E.; Kaufeld, T.; Umminger, J.; Fleissner, F.; Koigeldiyev, N.; Krueger, H.; Puntigam, J.; Haverich, A.; Shrestha, M. Total aortic arch repair: Risk factor analysis and follow-up in 199 patients. Eur. J. Cardio-Thorac. Surg. 2016, 50, 940–948. [Google Scholar] [CrossRef]
- Leone, A.; Beckmann, E.; Martens, A.; Di Marco, L.; Pantaleo, A.; Reggiani, L.B.; Haverich, A.; Di Bartolomeo, R.; Pacini, D.; Shrestha, M. Total aortic arch replacement with frozen elephant trunk technique: Results from two European institutes. J. Thorac. Cardiovasc. Surg. 2020, 159, 1201–1211. [Google Scholar] [CrossRef] [PubMed]
- Leontyev, S.; Misfeld, M.; Daviewala, P.; Borger, M.A.; Etz, C.D.; Belaev, S.; Seeburger, J.; Holzhey, D.; Bakhtiary, F.; Mohr, F.W. Early- and medium-term results after aortic arch replacement with frozen elephant trunk techniques-a single center study. Ann. Cardiothorac. Surg. 2013, 2, 606–611. [Google Scholar] [CrossRef]
- Acher, C.; Wynn, M. Paraplegia after thoracoabdominal aortic surgery: Not just assisted circulation, hypothermic arrest, clamp and sew, or TEVAR. Ann. Cardiothorac. Surg. 2012, 1, 365–372. [Google Scholar] [CrossRef]
- Kremer, J.; Preisner, F.; Dib, B.; Tochtermann, U.; Ruhparwar, A.; Karck, M.; Farag, M. Aortic arch replacement with frozen elephant trunk technique—A single-center study. J. Cardiothorac. Surg. 2019, 14, 147. [Google Scholar] [CrossRef] [PubMed]
- Griepp, R.B.; Ergin, M.A.; Galla, J.D.; Lansman, S.; Khan, N.; Quintana, C.; McCollough, J.; Bodian, C. Looking for the artery of Adamkiewicz: A quest to minimize paraplegia after operations for aneurysms of the descending thoracic and thoracoabdominal aorta. J. Thorac. Cardiovasc. Surg. 1996, 112, 1202–1215. [Google Scholar] [CrossRef]
- Kowalczyk, J. Albert Wojciech Adamkiewicz and his artery. South Afr. Med. J. 2002, 92, 702. [Google Scholar]
- Etz, C.D.; Zoli, S.; Bischoff, M.S.; Bodian, C.; Di Luozzo, G.; Griepp, R.B. Measuring the collateral network pressure to minimize paraplegia risk in thoracoabdominal aneurysm resection. J. Thorac. Cardiovasc. Surg. 2010, 140, S125–S130. [Google Scholar] [CrossRef]
- Etz, C.D.; Kari, F.A.; Mueller, C.S.; Silovitz, D.; Brenner, R.M.; Lin, H.M.; Griepp, R.B. The collateral network concept: A reassessment of the anatomy of spinal cord perfusion. J. Thorac. Cardiovasc. Surg. 2011, 141, 1020–1028. [Google Scholar] [CrossRef]
- Okita, Y.; Okada, K.; Omura, A.; Kano, H.; Minami, H.; Inoue, T.; Miyahara, S. Total arch replacement using antegrade cerebral perfusion. J. Thorac. Cardiovasc. Surg. 2013, 145, S63–S71. [Google Scholar] [CrossRef]
- Dong, Z.; Liu, H.; Kim, J.B.; Gu, J.; Li, M.; Li, G.; Du, J.; Gu, W.; Shao, Y.; Ni, B. False lumen-dependent segmental arteries are associated with spinal cord injury in frozen elephant trunk procedure for acute type I aortic dissection. JTCVS Open 2023, 15, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, M.; Martens, A.; Krüger, H.; Maeding, I.; Ius, F.; Fleissner, F.; Haverich, A. Total aortic arch replacement with the elephant trunk technique: Single-centre 30-year results. Eur. J. Cardio-Thorac. Surg. 2014, 45, 289–296. [Google Scholar] [CrossRef]
- Kiryu, K.; Yamamoto, H.; Kadohama, T.; Takagi, D.; Itagaki, Y.; Wada, T.; Igarashi, I. Risk factors for spinal cord ischemia in frozen elephant trunk–induced upper spinal cord ischemia in patients with combination of degenerative arch aneurysms and peripheral artery diseases: A possible mechanism. Cardiothorac. Surg. 2021, 29, 22. [Google Scholar] [CrossRef]
- Skalski, J.H.; Zembala, M. Albert Wojciech Adamkiewicz: The discoverer of the variable vascularity of the spinal cord. Ann. Thorac. Surg. 2005, 80, 1971–1975. [Google Scholar] [CrossRef]
- Ahn, H.; Fehlings, M.G. Prevention, identification, and treatment of perioperative spinal cord injury. Neurosurg. Focus 2008, 25, E15. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, L.J.; Rezayat, C.; Shrikhande, G.V.; Bush, H.L. Delayed permanent paraplegia after endovascular repair of abdominal aortic aneurysm. J. Vasc. Surg. 2010, 51, 725–728. [Google Scholar] [CrossRef][Green Version]
- Wei, J.; Hu, Z.; Wang, W.; Ding, R.; Chen, Z.; Yuan, X.; Xu, F. Posterior False Lumen and Paraplegia After FET Procedure in Acute Type A Aortic Dissection. Ann. Thorac. Surg. 2024, 117, 1136–1143. [Google Scholar] [CrossRef]
- Geisbüsch, S.; Schray, D.; Bischoff, M.S.; Lin, H.M.; Griepp, R.B.; Di Luozzo, G. Imaging of vascular remodeling after simulated thoracoabdominal aneurysm repair. J. Thorac. Cardiovasc. Surg. 2012, 144, 1471–1478. [Google Scholar] [CrossRef][Green Version]
- Geisbüsch, S.; Stefanovic, A.; Koruth, J.S.; Lin, H.M.; Morgello, S.; Weisz, D.J.; Griepp, R.B.; Di Luozzo, G. Endovascular coil embolization of segmental arteries prevents paraplegia after subsequent thoracoabdominal aneurysm repair: An experimental model. J. Thorac. Cardiovasc. Surg. 2014, 147, 220–227. [Google Scholar] [CrossRef]
- Tanaka, A.; Safi, H.J.; Estrera, A.L. Current strategies of spinal cord protection during thoracoabdominal aortic surgery. Gen. Thorac. Cardiovasc. Surg. 2018, 66, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, T.; Yoshida, H.; Hachiro, K.; Suzuki, T.; Asai, T. Spinal cord collateral flow during antegrade cerebral perfusion for aortic arch surgery. J. Thorac. Cardiovasc. Surg. 2020, 160, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Czerny, M.; Grabenwöger, M.; Berger, T.; Aboyans, V.; Della Corte, A.; Chen, E.P.; Desai, N.D.; Dumfarth, J.; Elefteriades, J.A.; Etz, C.D.; et al. EACTS/STS Guidelines for Diagnosing and Treating Acute and Chronic Syndromes of the Aortic Organ. Ann. Thorac. Surg. 2024, 118, 5–115. [Google Scholar] [CrossRef]
- Cambria, R.P.; Davison, J.K.; Carter, C.; Brewster, D.C.; Chang, Y.; Clark, K.A.; Atamian, S. Epidural cooling for spinal cord protection during thoracoabdominal aneurysm repair: A five-year experience. J. Vasc. Surg. 2000, 31, 1093–1102. [Google Scholar] [CrossRef]
- Shimizu, H.; Mori, A.; Yoshitake, A.; Yamada, T.; Morisaki, H.; Okano, H.; Yozu, R. Thoracic and thoracoabdominal aortic repair under regional spinal cord hypothermia. Eur. J. Cardiothorac. Surg. 2014, 46, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Coselli, J.S.; LeMaire, S.A.; Köksoy, C.; Schmittling, Z.C.; Curling, P.E. Cerebrospinal fluid drainage reduces paraplegia after thoracoabdominal aortic aneurysm repair: Results of a randomized clinical trial. J. Vasc. Surg. 2002, 35, 631–639. [Google Scholar] [CrossRef]
- Banga, P.V.; Oderich, G.S.; Reis de Souza, L.; Hofer, J.; Cazares Gonzalez, M.L.; Pulido, J.N.; Cha, S.; Gloviczki, P. Neuromonitoring, Cerebrospinal Fluid Drainage, and Selective Use of Iliofemoral Conduits to Minimize Risk of Spinal Cord Injury During Complex Endovascular Aortic Repair. J. Endovasc. Ther. 2016, 23, 139–149. [Google Scholar] [CrossRef]
- Fedorow, C.A.; Moon, M.C.; Mutch, W.A.C.; Grocott, H.P. Lumbar cerebrospinal fluid drainage for thoracoabdominal aortic surgery: Rationale and practical considerations for management. Anesth. Analg. 2010, 111, 46–58. [Google Scholar] [CrossRef]
- Marturano, F.; Nisi, F.; Giustiniano, E.; Benedetto, F.; Piccioni, F.; Ripani, U. Prevention of Spinal Cord Injury during Thoracoabdominal Aortic Aneurysms Repair: What the Anaesthesiologist Should Know. J. Pers. Med. 2022, 12, 1629. [Google Scholar] [CrossRef]
- Laschinger, J.C.; Cunningham, J.N.; Cooper, M.M.; Krieger, K.; Nathan, I.M.; Spencer, F.C. Prevention of ischemic spinal cord injury following aortic cross-clamping: Use of corticosteroids. Ann. Thorac. Surg. 1984, 38, 500–507. [Google Scholar] [CrossRef]
- Woloszyn, T.T.; Marini, C.P.; Coons, M.S.; Nathan, I.M.; Basu, S.; Acinapura, A.J.; Cunningham, J.N. Cerebrospinal fluid drainage and steroids provide better spinal cord protection during aortic cross-clamping than does either treatment alone. Ann. Thorac. Surg. 1990, 49, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Acher, C.; Acher, C.W.; Marks, E.; Wynn, M. Intraoperative neuroprotective interventions prevent spinal cord ischemia and injury in thoracic endovascular aortic repair. J. Vasc. Surg. 2016, 63, 1458–1465. [Google Scholar] [CrossRef]
- Witcher, A.C.; Meers, B.; Lewis, C.T.; Beck, A.W.; Eudailey, K.W. Rescue of False Lumen Frozen Elephant Trunk Deployment Intraoperatively. Ann. Thorac. Surg. 2023, 116, e5–e7. [Google Scholar] [CrossRef] [PubMed]
- Ghazy, T.; Darwisch, A.; Schmidt, T.; Fajfrova, Z.; Zickmüller, C.; Masshour, A.; Matschke, K.; Kappert, U. Transcranial Doppler Sonography for Optimization of Cerebral Perfusion in Aortic Arch Operation. Ann. Thorac. Surg. 2016, 101, e15–e16. [Google Scholar] [CrossRef][Green Version]
- D’Andrea, A.; Conte, M.; Cavallaro, M.; Scarafile, R.; Riegler, L.; Cocchia, R.; Pezzullo, E.; Carbone, A.; Natale, F.; Santoro, G.; et al. Transcranial Doppler ultrasonography: From methodology to major clinical applications. World J. Cardiol. 2016, 8, 383–400. [Google Scholar] [CrossRef] [PubMed]
- Ostberg, N.P.; Zafar, M.A.; Ziganshin, B.A.; Elefteriades, J.A. The Genetics of Thoracic Aortic Aneurysms and Dissection: A Clinical Perspective. Biomolecules 2020, 10, 182. [Google Scholar] [CrossRef]
- Isselbacher, E.; Preventza, O.; Hamilton Black Iii, J.; Augoustides, J.G.; Beck, A.W.; Bolen, M.A.; Braverman, A.C.; Bray, B.E.; Brown-Zimmerman, M.M.; Chen, E.P.; et al. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. JACC 2022, 80, e223–e393. [Google Scholar] [CrossRef]
- Olsen, P.L.; Hoffman, C.R.; Green, M.S. Naloxone Infusion During Thoracic Endovascular Aortic Aneurysm Repair to Prevent Spinal Cord Injury. J. Cardiothorac. Vasc. Anesth. 2018, 32, e37. [Google Scholar] [CrossRef]
- Kunihara, T.; Matsuzaki, K.; Shiiya, N.; Saijo, Y.; Yasuda, K. Naloxone lowers cerebrospinal fluid levels of excitatory amino acids after thoracoabdominal aortic surgery. J. Vasc. Surg. 2004, 40, 681–690. [Google Scholar] [CrossRef]
- Faden, A.I.; Jacobs, T.P.; Zivin, J.A. Comparison of naloxone and a δ-selective antagonist in experimental spinal stroke. Life Sci. 1983, 33, 707–710. [Google Scholar] [CrossRef]
- Liu, L.Y.; Callahan, B.; Peterss, S.; Dumfarth, J.; Tranquilli, M.; Ziganshin, B.A.; Elefteriades, J.A. Neuromonitoring Using Motor and Somatosensory Evoked Potentials in Aortic Surgery. J. Card. Surg. 2016, 31, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Aru, R.G.; Stonko, D.P.; Tan, L.T.; Sorber, R.A.; Hicks, C.W.; Black, J.H. Utility of motor-evoked potentials in contemporary open thoracoabdominal aortic repair. J. Vasc. Surg. 2024, 80, 979–987. [Google Scholar] [CrossRef] [PubMed]
| High Risk | Low Risk | |
|---|---|---|
| Demographics | Age > 70 | Age < 50 |
| Hx of CKD | Low arterial calcification score | |
| Hx of diabetes mellitus Redo cardiovascular surgery Previous stroke Atherosclerotic disease of aorta | ||
| Factors Associated with Pathology | Type A aortic dissection with carotid involvement | Aortic aneurysm with no dissection |
| Type B aortic dissection with posterior false lumen Highly perfused false lumen Aneurysm w/abdominal aortic distention | Poorly perfused false lumen Platelet count > 60 × 109 L | |
| Factors Associated with Procedure | Femoral artery cannulation | Subclavian graft |
| Prolonged LBCA > 50 min | Dual cannulation | |
| Lack of subclavian artery reimplantation | ||
| Postoperative hypotension |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myers, A.; Nita, C.; Martinez, G. Cerebral and Spinal Cord Protection Strategies in Aortic Arch Surgery. J. Cardiovasc. Dev. Dis. 2025, 12, 130. https://doi.org/10.3390/jcdd12040130
Myers A, Nita C, Martinez G. Cerebral and Spinal Cord Protection Strategies in Aortic Arch Surgery. Journal of Cardiovascular Development and Disease. 2025; 12(4):130. https://doi.org/10.3390/jcdd12040130
Chicago/Turabian StyleMyers, Andrea, Ciprian Nita, and Guillermo Martinez. 2025. "Cerebral and Spinal Cord Protection Strategies in Aortic Arch Surgery" Journal of Cardiovascular Development and Disease 12, no. 4: 130. https://doi.org/10.3390/jcdd12040130
APA StyleMyers, A., Nita, C., & Martinez, G. (2025). Cerebral and Spinal Cord Protection Strategies in Aortic Arch Surgery. Journal of Cardiovascular Development and Disease, 12(4), 130. https://doi.org/10.3390/jcdd12040130





