Higher LDL-C/HDL-C Ratio Is Associated with Elevated HbA1c and Decreased eGFR Levels and Cardiac Remodeling in Elderly with Hypercholesterolemia
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Diagnostic Criteria for Comorbidities
2.3. Measurement of Lipids, Glycated Hemoglobin and High-Sensitivity C-Reactive Protein
2.4. Calculation of Estimated Glomerular Filtration Rate and Body Mass Index
2.5. Detection of Cardiac Structure and Function
2.6. Statistical Analysis
3. Results
3.1. Clinical Characteristics According to the Tertiles of the LDL-C/HDL-C Ratio
3.2. Cardiac Remodeling Corresponding to the Tertiles of the LDL-C/HDL-C Ratio
3.3. Logistic Regression Analysis of High LDL-C/HDL-C Ratio with Clinical Characteristics and Echocardiographic Parameters
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lu, Y.; Zhang, H.; Lu, J.; Ding, Q.; Li, X.; Wang, X.; Sun, D.; Tan, L.; Mu, L.; Liu, J.; et al. Prevalence of dyslipidemia and availability of lipid-lowering medications among primary health care settings in China. JAMA. Netw. Open 2021, 4, e2127573. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Deng, Q.; Wang, L.; Huang, Z.; Zhou, M.; Li, Y.; Zhao, Z.; Zhang, Y.; Wang, L. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: A nationally representative survey of 163,641 adults. Int. J. Cardiol. 2018, 260, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Wei, D.; Wang, C.; Zhang, J.; Pan, L.; Ma, M.; Xue, F.; Wu, Z.; Shan, G. Prevalence of dyslipidemia and associated factors in the Yi farmers and migrants of southwestern China. Atherosclerosis 2012, 223, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Lu, Z.; Zhu, L.; Ouyang, X.; Yang, Y.; He, W.; Feng, Y.; Yi, F.; Song, Y. Lipoprotein ratios are better than conventional lipid parameters in predicting coronary heart disease in Chinese Han people. Kardiol. Pol. 2015, 73, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Awano, K. Is low-density lipoprotein/high-density lipoprotein (LDL/HDL)-cholesterol ratio a more important predictor of vulnerable plaque in coronary artery disease than LDL- or HDL-cholesterol? Circ. J. 2010, 74, 1294–1295. [Google Scholar] [CrossRef]
- Young, K.A.; Maturu, A.; Lorenzo, C.; Langefeld, C.D.; Wagenknecht, L.E.; Chen, Y.I.; Taylor, K.D.; Rotter, J.I.; Norris, J.M.; Rasouli, N. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of insulin resistance, beta-cell function, and diabetes in Hispanics and African Americans. J. Diabetes Complicat. 2019, 33, 118–122. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Zhu, L.; Cui, X.; Feng, L.; Zhao, X.; He, S.; Ping, F.; Li, W.; Li, Y. The triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio as a predictor of insulin resistance but not of beta cell function in a Chinese population with different glucose tolerance status. Lipids Health Dis. 2016, 15, 104. [Google Scholar] [CrossRef]
- Wei, L.; Wei, M.; Chen, L.; Liang, S.; Gao, F.; Cheng, X.; Jiang, H. Low-density lipoprotein cholesterol: High-density lipoprotein cholesterol ratio is associated with incident diabetes in Chinese adults: A retrospective cohort study. J. Diabetes Investig. 2021, 12, 91–98. [Google Scholar] [CrossRef]
- Okumura, S.; Sakakibara, M.; Hayashida, R.; Jinno, Y.; Tanaka, A.; Okada, K.; Hayashi, M.; Ishii, H.; Murohara, T. Accelerated decline in renal function after acute myocardial infarction in patients with high low-density lipoprotein-cholesterol to high-density lipoprotein-cholesterol ratio. Heart Vessel. 2014, 29, 7–14. [Google Scholar] [CrossRef]
- Wang, H.; Li, Z.; Guo, X.; Chen, Y.; Chang, Y.; Chen, S.; Sun, Y. The impact of nontraditional lipid profiles on left ventricular geometric abnormalities in general Chinese population. BMC. Cardiovasc. Disord. 2018, 18, 88. [Google Scholar] [CrossRef]
- Lin, T.; Xia, X.; Yu, J.; Qiu, Y.; Yi, C.; Lin, J.; Mao, H.; Yang, X.; Huang, F. The predictive study of the relation between elevated low-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio and mortality in peritoneal dialysis. Lipids Health Dis. 2020, 19, 51. [Google Scholar] [CrossRef] [PubMed]
- Kunutsor, S.K.; Zaccardi, F.; Karppi, J.; Kurl, S.; Laukkanen, J.A. Is high serum LDL/HDL cholesterol ratio an emerging risk factor for sudden cardiac death? findings from the KIHD study. J. Atheroscler. Thromb. 2017, 24, 600–608. [Google Scholar] [CrossRef] [PubMed]
- Panes, O.; Gonzalez, C.; Hidalgo, P.; Valderas, J.P.; Acevedo, M.; Contreras, S.; Sanchez, X.; Pereira, J.; Rigotti, A.; Mezzno, D. Platelet tissue factor activity and membrane cholesterol are increased in hypercholesterolemia and normalized by rosuvastatin, but not by atorvastatin. Atherosclerosis 2017, 257, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.A.; Jones, J.G.; Cumming, S.P.; Coelhoe Silva, M.J.; Teixeira, A.M.; Verissimo, M.T. Glycated hemoglobin and associated risk factors in older adults. Cardiovasc. Diabetol. 2012, 11, 13. [Google Scholar] [CrossRef] [PubMed]
- Dowla, S.; Aslibekyan, S.; Goss, A.; Fontaine, K.; Ashraf, A.P. Dyslipidemia is associated with pediatric nonalcoholic fatty liver disease. J. Clin. Lipidol. 2018, 12, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.V.; De Silva, D.A.; Macleod, M.R.; Coutts, S.B.; Schwamm, L.H.; Davis, S.M.; Donnan, G.A. Ischaemic stroke. Nat. Rev. Dis. Primers 2019, 5, 70. [Google Scholar] [CrossRef] [PubMed]
- Miida, T.; Nishimura, K.; Hirayama, S.; Miyamoto, Y.; Nakamura, M.; Masuda, D.; Yamashita, S.; Ushiyama, M.; Komori, T.; Fujita, N.; et al. Homogeneous assays for LDL-C and HDL-C are reliable in both the postprandial and fasting state. J. Atheroscler. Thromb. 2017, 24, 583–599. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Li, G.; Laukkanen, J.A.; Song, X.; Zhang, J.; Wei, L.; Chen, X.; Li, Y.; Liu, C. Higher neutrophil to lymphocyte ratio is associated with renal dysfunction and cardiac adverse remodeling in elderly with metabolic syndrome. Front. Cardiovasc. Med. 2022, 9, 921204. [Google Scholar] [CrossRef] [PubMed]
- Song, L.; Buggs, V.; Samara, V.A.; Bahri, S. Calculation of the estimated glomerular filtration rate using the 2021 CKD-EPI creatinine equation and whole blood creatinine values measured with radiometer ABL 827 FLEX. Clin. Chem. Lab. Med. 2022, 60, 867–876. [Google Scholar] [CrossRef]
- Sun, G.Z.; Li, Z.; Guo, L.; Zhou, Y.; Yang, H.M.; Sun, Y.X. High prevalence of dyslipidemia and associated risk factors among rural Chinese adults. Lipids Health Dis. 2014, 13, 189. [Google Scholar] [CrossRef]
- Galderisi, M.; Cosyns, B.; Edvardsen, T.; Cardim, N.; Delgado, V.; Di Salvo, G.; Donal, E.; Sade, L.E.; Ernande, L.; Garbi, M.; et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: An expert consensus document of the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 1301–1310. [Google Scholar] [PubMed]
- Liu, L.; Yin, P.; Lu, C.; Li, J.; Zang, Z.; Liu, Y.; Liu, S.; Wei, Y. Association of LDL-C/HDL-C ratio with stroke outcomes within 1 year after onset: A hospital-based follow-up study. Front. Neurol. 2020, 11, 408. [Google Scholar] [CrossRef] [PubMed]
- El Khoudary, S.R. HDL and the menopause. Curr. Opin. Lipidol. 2017, 28, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Deng, B.; Luo, T.; Huang, Y.; Shen, T.; Ma, J. Prevalence and determinants of hyperlipidemia in moderate altitude areas of the Yunnan-Kweichow plateau in southwestern China. High. Alt. Med. Biol. 2012, 13, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Lorbek, G.; Perse, M.; Horvat, S.; Bjorkhem, I.; Rozman, D. Sex differences in the hepatic cholesterol sensing mechanisms in mice. Molecules 2013, 18, 11067–11085. [Google Scholar] [CrossRef] [PubMed]
- De Marinis, E.; Martini, C.; Trentalance, A.; Pallottini, V. Sex differences in hepatic regulation of cholesterol homeostasis. J. Endocrinol. 2008, 198, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Ambikairajah, A.; Walsh, E.; Cherbuin, N. Lipid profile differences during menopause: A review with meta-analysis. Menopause 2019, 26, 1327–1333. [Google Scholar] [CrossRef]
- Lee, C.E.; Kang, J.S.; Kim, K.I. Effects of gender, gonadectomy and sex hormones on growth and plasma cholesterol level in rats. Ann. Nutr. Metab. 2008, 53, 1–5. [Google Scholar] [CrossRef]
- Vincent, M.J.; Allen, B.; Palacios, O.M.; Haber, L.T.; Maki, K.C. Meta-regression analysis of the effects of dietary cholesterol intake on LDL and HDL cholesterol. Am. J. Clin. Nutr. 2019, 109, 7–16. [Google Scholar] [CrossRef]
- Goh, V.H.; Tong, T.Y.; Mok, H.P.; Said, B. Differential impact of aging and gender on lipid and lipoprotein profiles in a cohort of healthy Chinese Singaporeans. Asian J. Androl. 2007, 9, 787–794. [Google Scholar] [CrossRef]
- Wakabayashi, I.; Groschner, K. Age-dependent associations of smoking and drinking with non-high-density lipoprotein cholesterol. Metabolism 2010, 59, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Zaid, M.; Miura, K.; Okayama, A.; Nakagawa, H.; Sakata, K.; Saitoh, S.; Okuda, N.; Yoshita, K.; Choudhury, S.R.; Rodriguez, B.; et al. Associations of high-density lipoprotein particle and high-density lipoprotein cholesterol with alcohol intake, smoking, and body mass index -the INTERLIPID study. Circ. J. 2018, 82, 2557–2565. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Ogawa, K.; Tanaka, T.D.; Nagoshi, T.; Minai, K.; Ogawa, T.; Kawai, M.; Yoshimura, M. Increase in oxidized low-density lipoprotein level according to hyperglycemia in patients with cardiovascular disease: A study by structure equation modeling. Diabetes Res. Clin. Pract. 2020, 161, 108036. [Google Scholar] [CrossRef]
- Dong, H.; Wang, J.; Hu, P.; Lu, N. Associations of apolipoprotein A1, high density lipoprotein cholesterol with hemoglobin glycation index and triglyceride-glucose index in Chinese adults with coronary artery disease. J. Diabetes Complicat. 2023, 37, 108516. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Lu, N.; Hu, P.; Wang, J. Associations of serum apolipoprotein A1 and high density lipoprotein cholesterol with glucose level in patients with coronary artery disease. Angiology 2023, 33197231187228. [Google Scholar] [CrossRef]
- Dong, H.; Ni, W.; Bai, Y.; Yuan, X.; Zhang, Y.; Zhang, H.; Sun, Y.; Xu, J. Cross-sectional and longitudinal associations of apolipoprotein A1 and B with glycosylated hemoglobin in Chinese adults. Sci. Rep. 2022, 12, 2751. [Google Scholar] [CrossRef]
- Yao, C.A.; Yen, T.Y.; Hsu, S.H.; Su, T.C. Glycative stress, glycated hemoglobin, and atherogenic dyslipidemia in patients with hyperlipidemia. Cells 2023, 12, 640. [Google Scholar] [CrossRef] [PubMed]
- Kuma, A.; Uchino, B.; Ochiai, Y.; Kawashima, M.; Enta, K.; Tamura, M.; Otsuji, Y.; Kato, A. Impact of low-density lipoprotein cholesterol on decline in estimated glomerular filtration rate in apparently healthy young to middle-aged working men. Clin. Exp. Nephrol. 2018, 22, 15–27. [Google Scholar] [CrossRef]
- Morita, Y.; Homma, Y.; Igarashi, M.; Miyano, R.; Yamaguchi, H.; Matsuda, M.; Tanigaki, T.; Shiina, Y.; Homma, K. Decrease in glomerular filtration rate by plasma low-density lipoprotein cholesterol in subjects with normal kidney function assessed by urinalysis and plasma creatinine. Atherosclerosis 2010, 210, 602–606. [Google Scholar] [CrossRef]
- Markovic, D.; Trgo, G.; Prkacin, I.; Fabijanic, D.; Kovacic, V. The association between high-density lipoproteins and estimated glomerular filtration rate in patients without severe kidney disease. Int. Urol. Nephrol. 2018, 50, 1105–1112. [Google Scholar] [CrossRef]
- Wang, F.; Zheng, J.; Ye, P.; Luo, L.; Bai, Y.; Xu, R.; Sheng, L.; Xiao, T.; Wu, H. Association of high-density lipoprotein cholesterol with the estimated glomerular filtration rate in a community-based population. PLoS ONE 2013, 8, e79738. [Google Scholar] [CrossRef]
- Keddis, M.T.; Garovic, V.D.; Bailey, K.R.; Wood, C.M.; Raissian, Y.; Grande, J.P. Ischaemic nephropathy secondary to atherosclerotic renal artery stenosis: Clinical and histopathological correlates. Nephrol. Dial. Transplant. 2010, 25, 3615–3622. [Google Scholar] [CrossRef]
- Li, X.; Bayliss, G.; Zhuang, S. Cholesterol crystal embolism and chronic kidney disease. Int. J. Mol. Sci. 2017, 18, 1120. [Google Scholar] [CrossRef] [PubMed]
- Kawakami, R.; Matsumoto, I.; Shiomi, M.; Kurozumi, M.; Miyake, Y.; Ishizawa, M.; Ishikawa, K.; Murakami, K.; Noma, T.; Takagi, Y.; et al. Role of the low-density lipoprotein-cholesterol/high-density lipoprotein-cholesterol ratio in predicting serial changes in the lipid component of coronary plaque. Circ. J. 2017, 81, 1439–1446. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Wen, S.J.; Li, Z.Z.; Li, N.; Huang, J. Low-density lipoprotein cholesterol/high-density lipoprotein cholesterol ratio as predictor of first acute myocardial infarction and major adverse cardiovascular event after intervention in young males. Chin. Med. J. 2018, 131, 2239–2241. [Google Scholar] [CrossRef]
- Kanaoka, T.; Takahashi, J.; Wakamatsu, Y.; Ishii, K.; Gohda, T.; Sasaki, S.; Matsui, Y. Lowered postoperative LDL-C/HDL-C ratio reduces later cardiovascular events after abdominal aortic aneurysm surgery. Ann. Vasc. Dis. 2012, 5, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Song, X.; Li, G.; Zhu, Y.; Laukkanen, J.A. Glomerular filtration dysfunction is associated with cardiac adverse remodeling in menopausal diabetic Chinese women. Clin. Interv. Aging 2021, 16, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.C.; Chang, J.M.; Liu, W.C.; Tsai, Y.C.; Tsai, J.C.; Su, H.M.; Hwang, S.J.; Chen, H.C. Stepwise increases in left ventricular mass index and decreases in left ventricular ejection fraction correspond with the stages of chronic kidney disease in diabetes patients. Exp. Diabetes Res. 2012, 2012, 789325. [Google Scholar] [CrossRef]
- Opoku, S.; Gan, Y.; Fu, W.; Chen, D.; Addo-Yobo, E.; Trofimovitch, D.; Yue, W.; Yan, F.; Wang, Z.; Lu, Z. Prevalence and risk factors for dyslipidemia among adults in rural and urban China: Findings from the China national stroke screening and prevention project (CNSSPP). BMC. Public. Health 2019, 19, 1500. [Google Scholar] [CrossRef]

| Low LHR | Moderate LHR | High LHR | r | p | |
|---|---|---|---|---|---|
| LHR < 2.63 | 2.63 ≤ LHR < 3.33 | LHR ≥ 3.33 | |||
| n = 376 | n = 376 | n = 377 | |||
| LHR | 2.22 ± 0.29 | 2.98 ± 0.20 * | 3.99 ± 0.72 *† | 1.000 | <0.001 |
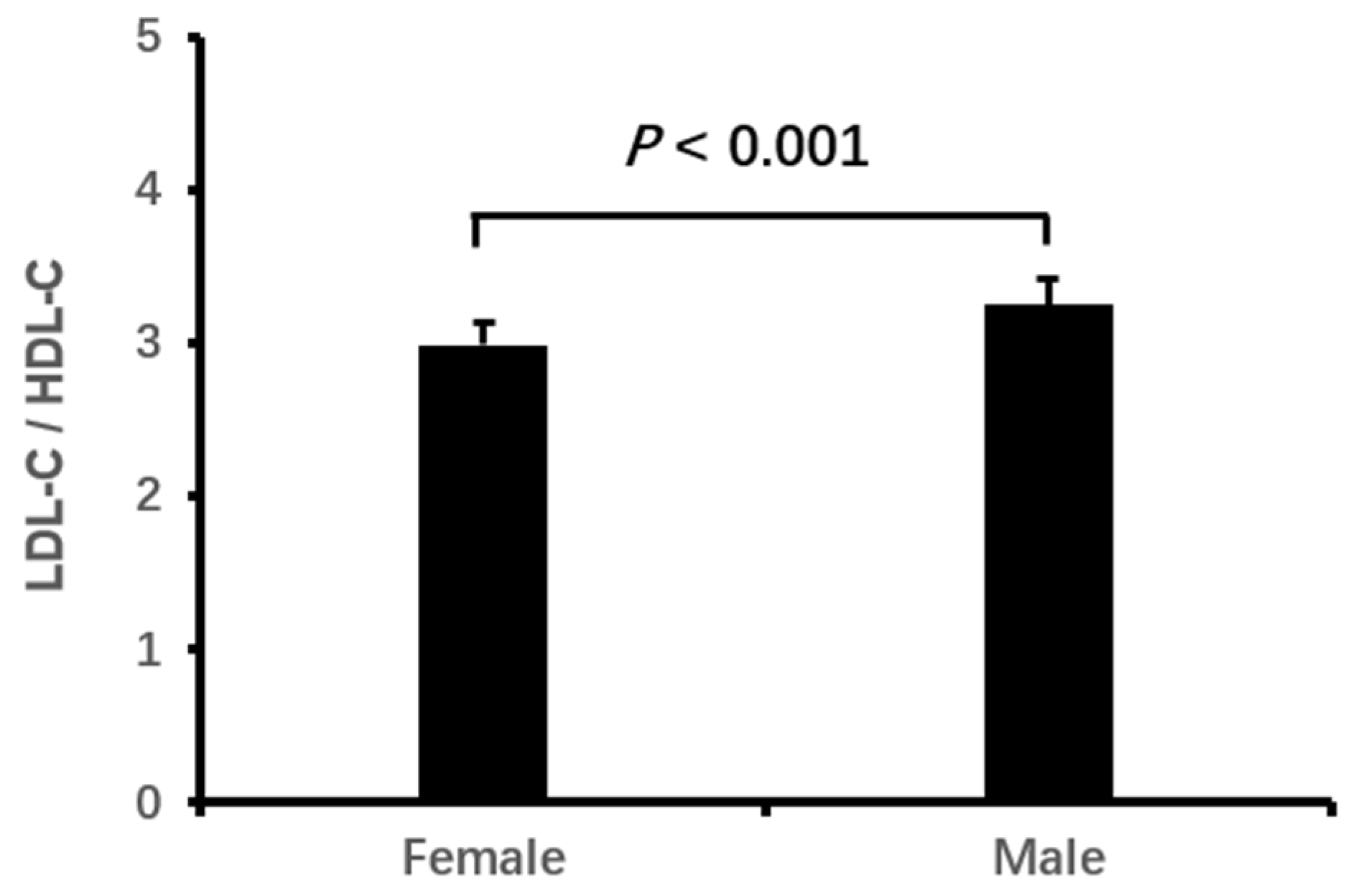
| Male, n (%) | 85 (22.6) | 100 (26.6) | 141 (37.4) *† | 0.133 | <0.001 |
| Age, year | 75.50 ± 6.51 | 75.14 ± 7.26 | 74.69 ± 6.68 | −0.049 | 0.240 |
| Body mass index, kg/m2 | 23.20 ± 3.63 | 24.43 ± 3.38 * | 24.69 ± 3.17 * | 0.176 | <0.001 |
| Smoking, n (%) | 44 (11.9) | 49 (13.2) | 90 (24.2) *† | 0.136 | <0.001 |
| Drinking, n (%) | 43 (11.6) | 47 (12.7) | 68 (18.3) * | 0.078 | 0.019 |
| Type 2 DM, n (%) | 95 (25.3) | 128 (34.0) * | 159 (42.2) * | 0.146 | <0.001 |
| Diabetic duration, year | 1.74 ± 4.62 | 2.88 ± 6.39 * | 3.67 ± 6.81 * | 0.131 | <0.001 |
| Hypertension, n (%) | 243 (64.6) | 250 (66.5) | 277 (73.5) * | 0.078 | 0.023 |
| Hypertensive duration, year | 7.62 ± 10.15 | 8.18 ± 11.24 | 8.28 ± 10.53 | 0.025 | 0.654 |
| Systolic BP, mmHg | 142.43 ± 22.52 | 143.11 ± 21.37 | 144.64 ± 21.58 | 0.041 | 0.365 |
| Diastolic BP, mmHg | 76.48 ± 12.65 | 77.51 ± 12.11 | 79.23 ± 13.40 * | 0.088 | 0.011 |
| Fatty liver, n (%) | 66 (22.8) | 105 (38.9) * | 107 (39.6) * | 0.147 | <0.001 |
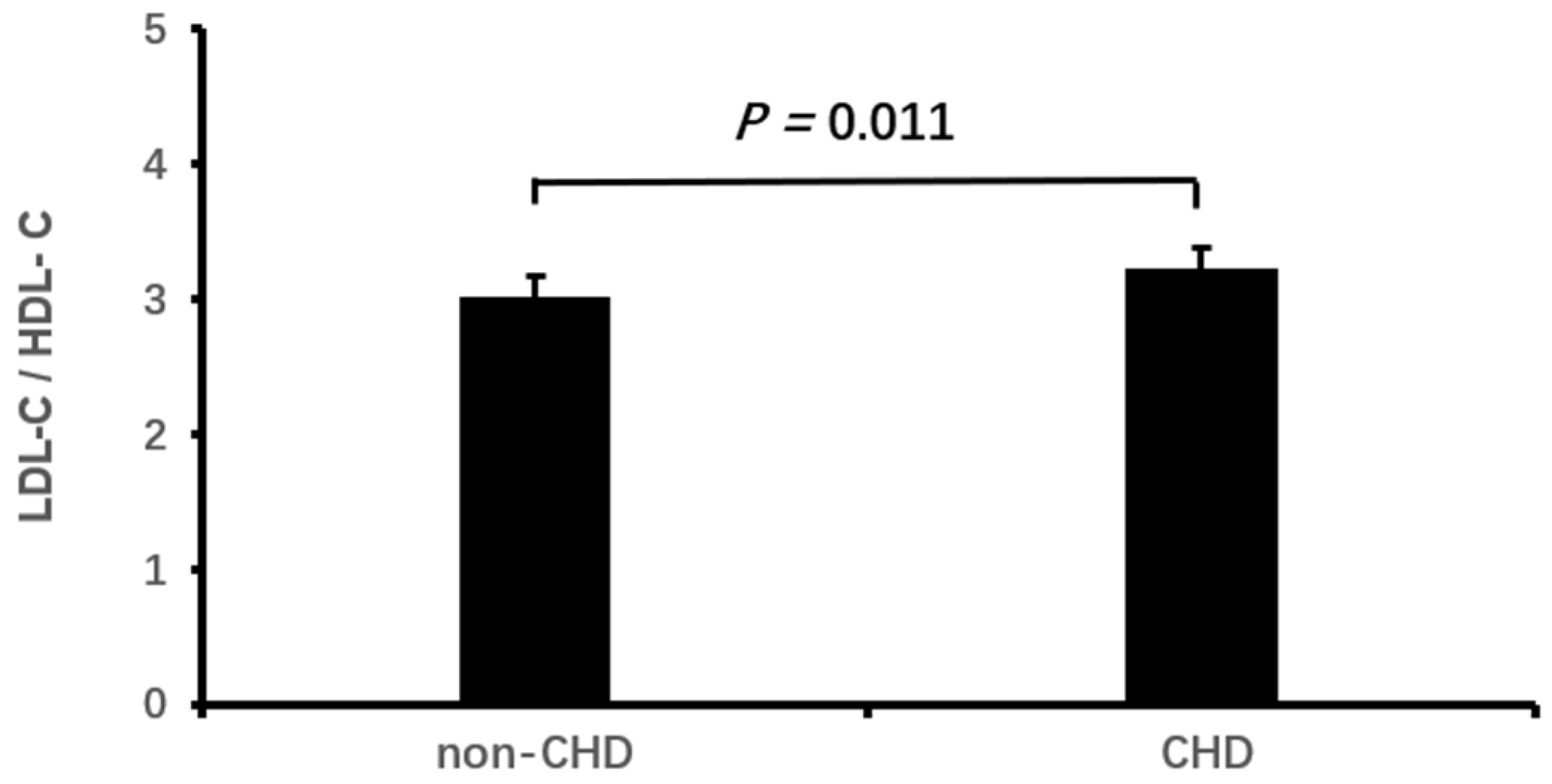
| Coronary heart disease, n (%) | 67 (17.8) | 78 (20.7) | 108 (28.6) *† | 0.106 | 0.001 |
| Stroke, n (%) | 141 (37.5) | 129 (34.3) | 126 (33.4) | −0.035 | 0.468 |
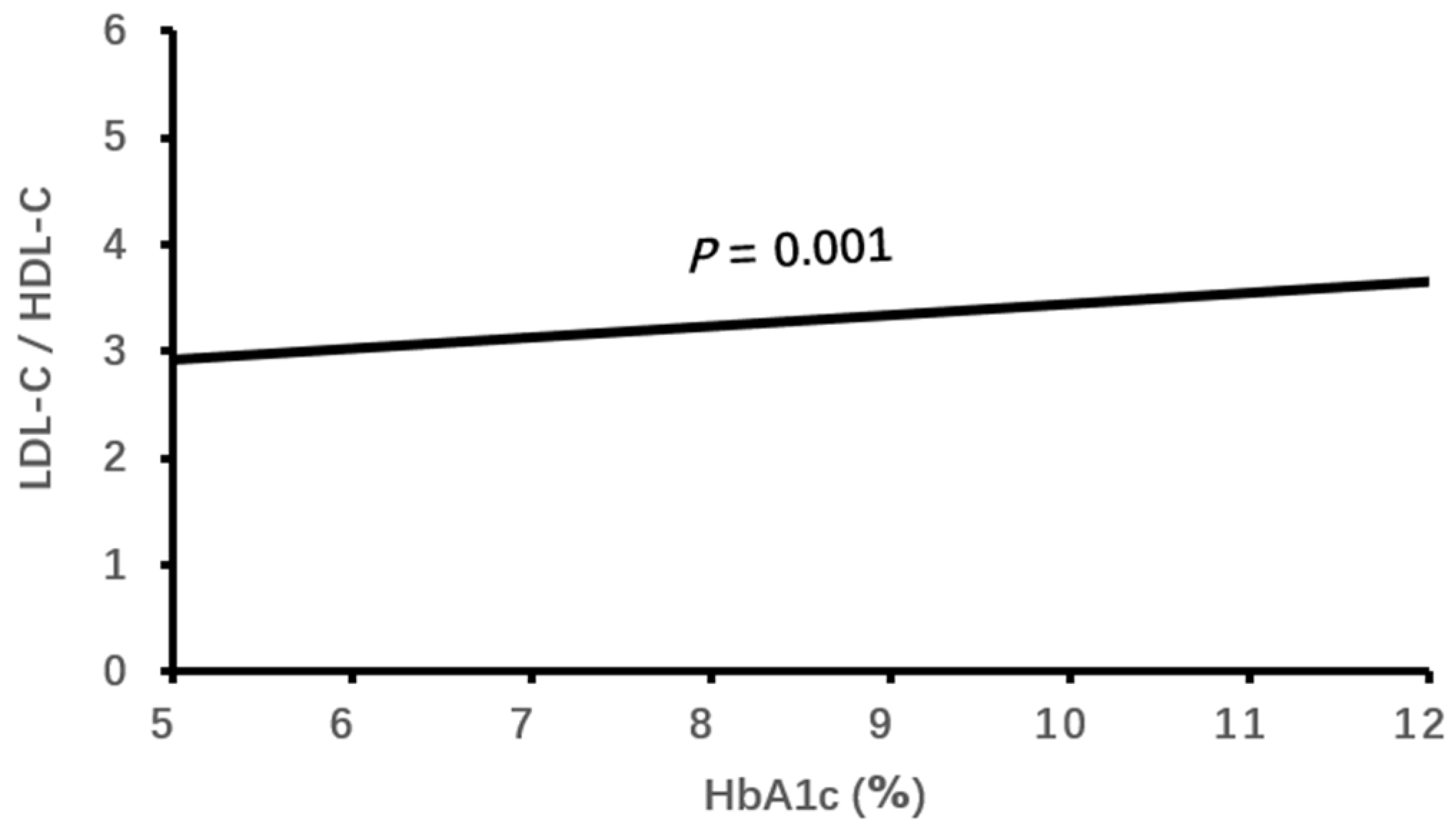
| HbA1c, % | 6.12 ± 1.04 | 6.51 ± 1.45 * | 6.81 ± 1.76 *† | 0.190 | <0.001 |
| eGFR, mL/min·1.73 m2 | 73.63 ± 18.40 | 73.71 ± 19.53 | 68.65 ± 21.85 *† | −0.101 | 0.001 |
| hsCRP, mg/L | 2.01 ± 2.79 | 2.29 ± 2.94 | 2.81 ± 3.27 * | 0.109 | 0.002 |
| LDL-C, mmol/L | 3.77 ± 0.35 | 3.91 ± 0.46 * | 4.19 ± 0.68 *† | 0.314 | <0.001 |
| HDL-C, mmol/L | 1.73 ± 0.28 | 1.32 ± 0.16 * | 1.07 ± 0.18 *† | −0.776 | <0.001 |
| TC, mmol/L | 5.75 ± 0.56 | 5.62 ± 0.62 * | 5.87 ± 0.89 *† | 0.067 | <0.001 |
| TG, mmol/L | 1.33 ± 0.60 | 1.70 ± 0.73 * | 2.20 ± 1.18 *† | 0.377 | <0.001 |
| Low LHR | Moderate LHR | High LHR | r | p | |
|---|---|---|---|---|---|
| LHR < 2.63 | 2.63 ≤ LHR < 3.33 | LHR ≥ 3.33 | |||
| n = 376 | n = 376 | n = 377 | |||
| RAD, mm | 33.32 ± 3.63 | 33.39 ± 3.54 | 33.72 ± 3.98 | 0.045 | 0.276 |
| RVD, mm | 18.85 ± 1.65 | 19.13 ± 1.57 * | 19.26 ± 1.75 * | 0.102 | 0.002 |
| LAD, mm | 29.51 ± 4.69 | 30.42 ± 4.62 * | 31.22 ± 5.55 *† | 0.139 | <0.001 |
| LVESD, mm | 30.48 ± 5.16 | 30.60 ± 4.31 | 31.71 ± 6.01 *† | 0.095 | 0.005 |
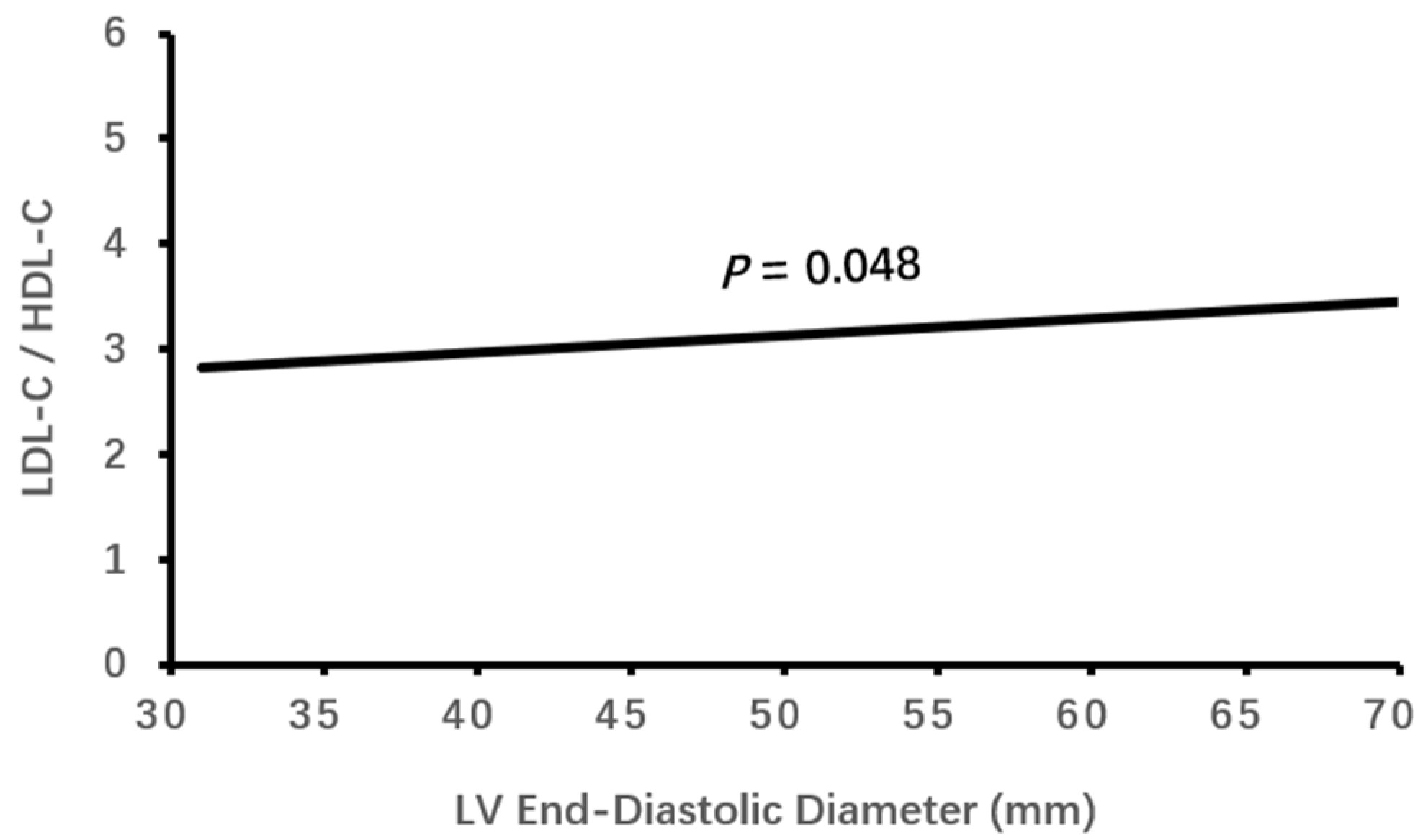
| LVEDD, mm | 45.92 ± 5.04 | 46.09 ± 4.69 | 46.87 ± 5.77 *† | 0.075 | 0.027 |
| IVST, mm | 10.52 ± 1.20 | 10.66 ± 1.22 | 10.90 ± 1.32 *† | 0.123 | <0.001 |
| LVPWT, mm | 10.36 ± 1.08 | 10.49 ± 1.18 | 10.68 ± 1.25 *† | 0.110 | 0.001 |
| LVEF, % | 62.61 ± 6.40 | 62.66 ± 5.28 | 61.06 ± 7.35 *† | −0.099 | 0.001 |
| E/A < 1, n (%) | 336 (100) | 347 (99.4) | 334 (98.5) | −0.073 | 0.064 |
| β | SE | Wald χ2 | p | OR (95% CI) | |
|---|---|---|---|---|---|
| Male | 0.690 | 0.193 | 12.848 | <0.001 | 1.994 (1.367–2.909) |
| Type 2 DM | −0.024 | 0.217 | 0.012 | 0.911 | 0.976 (0.638–1.493) |
| Hypertension | −0.012 | 0.204 | 0.003 | 0.955 | 0.989 (0.662–1.476) |
| Body mass index | 0.048 | 0.028 | 2.971 | 0.085 | 1.049 (0.993–1.017) |
| Diastolic BP | 0.002 | 0.007 | 0.234 | 0.628 | 1.003 (0.990–1.017) |
| Fatty liver | 0.368 | 0.192 | 3.679 | 0.055 | 1.445 (0.992–2.106) |
| Coronary heart disease | 0.547 | 0.215 | 6.471 | 0.011 | 1.727 (1.135–2.632) |
| HbA1c | 0.233 | 0.071 | 10.660 | 0.001 | 1.262 (1.097–1.451) |
| eGFR | −0.009 | 0.004 | 4.243 | 0.039 | 0.991 (0.983–1.000) |
| hsCRP | 0.016 | 0.025 | 0.381 | 0.537 | 1.016 (0.967–1.068) |
| RVD | 0.026 | 0.061 | 0.189 | 0.664 | 1.027 (0.911–1.157) |
| LAD | −0.005 | 0.024 | 0.041 | 0.840 | 0.995 (0.950–1.043) |
| LVESD | 0.158 | 0.102 | 2.391 | 0.122 | 1.171 (0.757–1.430) |
| LVEDD | −0.139 | 0.071 | 3.819 | 0.048 | 0.870 (0.756–1.000) |
| IVST | 0.074 | 0.115 | 0.412 | 0.521 | 1.077 (0.859–1.349) |
| LVPWT | 0.043 | 0.123 | 0.120 | 0.729 | 1.044 (0.820–1.329) |
| LVEF | 0.024 | 0.040 | 0.351 | 0.553 | 1.024 (0.947–1.108) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Li, G.; Laukkanen, J.A.; Wei, L.; Chen, X. Higher LDL-C/HDL-C Ratio Is Associated with Elevated HbA1c and Decreased eGFR Levels and Cardiac Remodeling in Elderly with Hypercholesterolemia. J. Cardiovasc. Dev. Dis. 2024, 11, 140. https://doi.org/10.3390/jcdd11050140
Li Y, Li G, Laukkanen JA, Wei L, Chen X. Higher LDL-C/HDL-C Ratio Is Associated with Elevated HbA1c and Decreased eGFR Levels and Cardiac Remodeling in Elderly with Hypercholesterolemia. Journal of Cardiovascular Development and Disease. 2024; 11(5):140. https://doi.org/10.3390/jcdd11050140
Chicago/Turabian StyleLi, Yufeng, Gang Li, Jari A. Laukkanen, Linping Wei, and Xinrui Chen. 2024. "Higher LDL-C/HDL-C Ratio Is Associated with Elevated HbA1c and Decreased eGFR Levels and Cardiac Remodeling in Elderly with Hypercholesterolemia" Journal of Cardiovascular Development and Disease 11, no. 5: 140. https://doi.org/10.3390/jcdd11050140
APA StyleLi, Y., Li, G., Laukkanen, J. A., Wei, L., & Chen, X. (2024). Higher LDL-C/HDL-C Ratio Is Associated with Elevated HbA1c and Decreased eGFR Levels and Cardiac Remodeling in Elderly with Hypercholesterolemia. Journal of Cardiovascular Development and Disease, 11(5), 140. https://doi.org/10.3390/jcdd11050140






