Prevalence of Cardiovascular Risk Factors among Young Adults (18–25 Years) in Mozambique
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Selection of Participants
2.3. Evaluation of the Participants
2.4. Statistical Analysis
3. Results
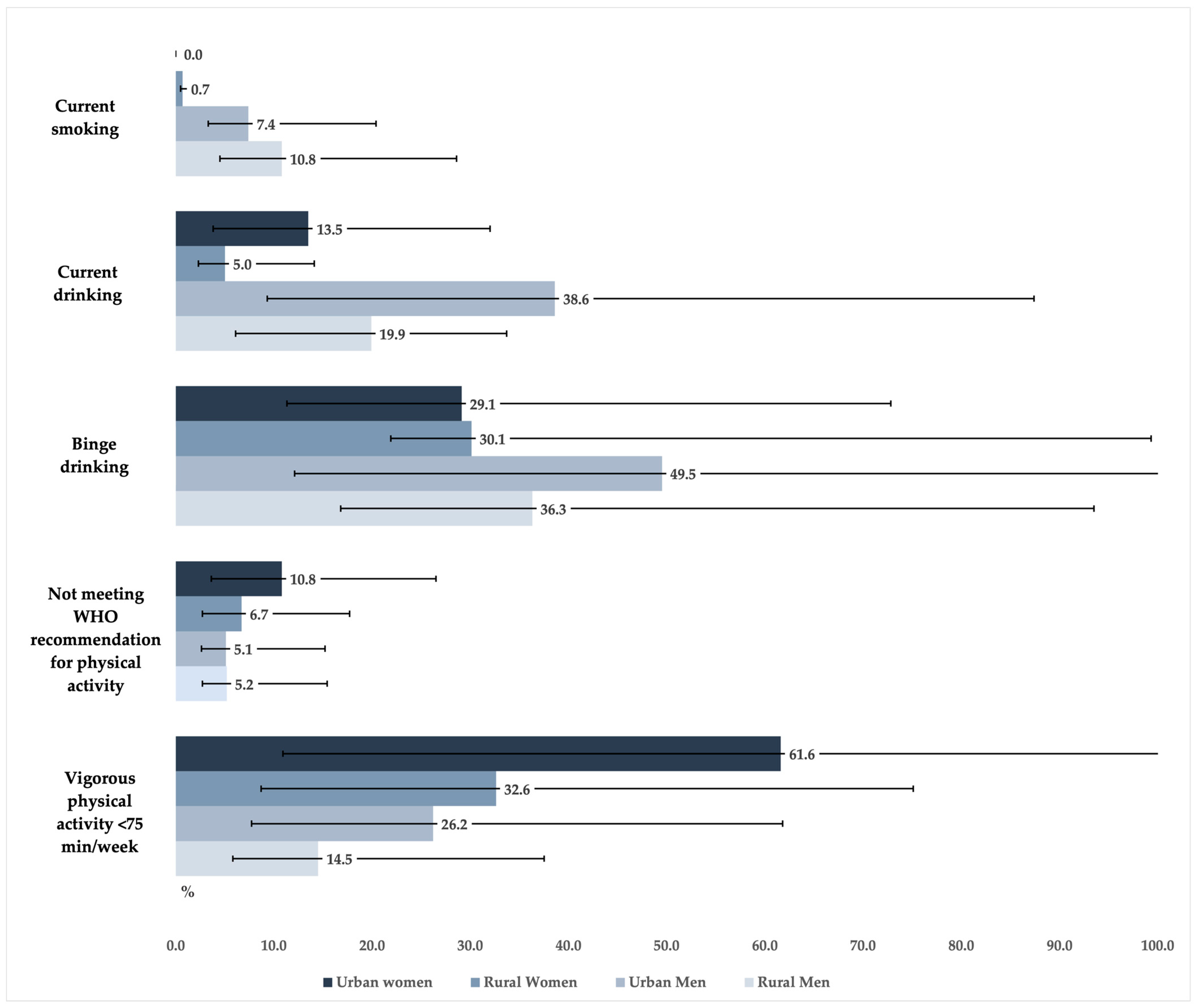
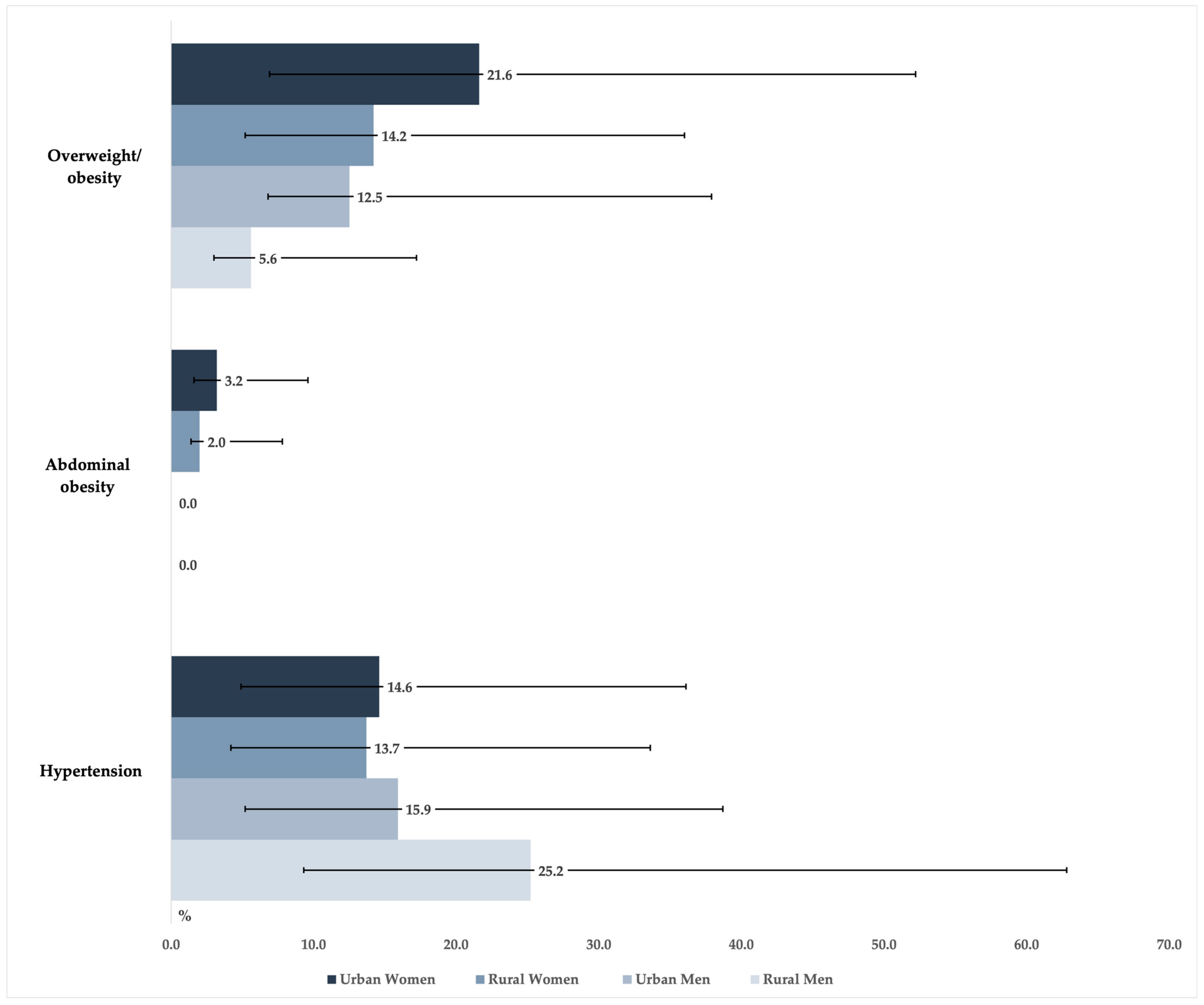
3.1. Prevalence of Risk Factors According to Sex and Place of Residence
3.2. Association between the Sociodemographic Characteristics and the Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar]
- Loukili, H.; Malka, G.; Hélène, L.; Frej, D.; Amine, M. Cardiovascular Diseases Risk Factors Among Young Adults: A STEPwise-Approach-Based Study in Three University Setups in Morocco. Open Public Health J. 2020, 13, 465–470. [Google Scholar] [CrossRef]
- Miura, K.; Daviglus, M.L.; Dyer, A.R.; Liu, K.; Garside, D.B.; Stamler, J.; Greenland, P. Relationship of Blood Pressure to 25-Year Mortality Due to Coronary Heart Disease, Cardiovascular Diseases, and All Causes in Young Adult Men: The Chicago Heart Association Detection Project in Industry. Arch. Intern. Med. 2001, 161, 1501–1508. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Aravkin, A.Y.; Zheng, P.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef] [PubMed]
- Lynch, E.B.; Liu, K.; Kiefe, C.I.; Greenland, P. Cardiovascular Disease Risk Factor Knowledge in Young Adults and 10-year Change in Risk Factors: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am. J. Epidemiol. 2006, 164, 1171–1179. [Google Scholar] [CrossRef]
- Shah, R.V.; Murthy, V.L.; Colangelo, L.A.; Reis, J.; Venkatesh, B.A.; Sharma, R.; Abbasi, S.A.; Goff, D.C., Jr.; Carr, J.J.; Rana, J.S.; et al. Association of Fitness in Young Adulthood with Survival and Cardiovascular Risk: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA Intern. Med. 2016, 176, 87–95. [Google Scholar] [CrossRef]
- Liu, K.; Daviglus, M.L.; Loria, C.M.; Colangelo, L.A.; Spring, B.; Moller, A.C.; Lloyd-Jones, D.M. Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation 2012, 125, 996–1004. [Google Scholar] [CrossRef] [PubMed]
- Hulsegge, G.; Looman, M.; Smit, H.A.; Daviglus, M.L.; van der Schouw, Y.T.; Verschuren, W.M. Lifestyle Changes in Young Adulthood and Middle Age and Risk of Cardiovascular Disease and All-Cause Mortality: The Doetinchem Cohort Study. J. Am. Heart Assoc. 2016, 5, e002432. [Google Scholar] [CrossRef]
- Nagata, J.M.; Vittinghoff, E.; Gabriel, K.P.; Rana, J.S.; Garber, A.K.; Moran, A.E.; Reis, J.P.; Lewis, C.E.; Sidney, S.; Bibbins-Domingo, K. Physical activity from young adulthood to middle age and premature cardiovascular disease events: A 30-year population-based cohort study. Int. J. Behav. Nutr. Phys. Act. 2022, 19, 123. [Google Scholar] [CrossRef] [PubMed]
- Gooding, H.C.; Shay, C.M.; Ning, H.; Gillman, M.W.; Chiuve, S.E.; Reis, J.P.; Allen, N.B.; Lloyd-Jones, D.M. Optimal Lifestyle Components in Young Adulthood Are Associated with Maintaining the Ideal Cardiovascular Health Profile into Middle Age. J. Am. Heart Assoc. 2015, 4, e002048. [Google Scholar] [CrossRef]
- Tran, D.M.; Zimmerman, L.M. Cardiovascular risk factors in young adults: A literature review. J. Cardiovasc. Nurs. 2015, 30, 298–310. [Google Scholar] [CrossRef] [PubMed]
- Oldenburg, B.; Baptista, S.; Cocker, F.; O’Neil, A. Changing Lifestyle Behaviors to Improve the Prevention and Management of Cardiovascular Disease. In Handbook of Psychocardiology; Alvarenga, M.E., Byrne, D., Eds.; Springer: Singapore, 2016; pp. 1077–1094. [Google Scholar]
- Macuane, J.J.; Buur, L.; Monjane, C.M. Power, conflict and natural resources: The Mozambican crisis revisited. Afr. Aff. 2017, 117, 415–438. [Google Scholar] [CrossRef]
- Fontes, F.; Damasceno, A.; Jessen, N.; Prista, A.; Silva-Matos, C.; Padrão, P.; Lunet, N. Prevalence of overweight and obesity in Mozambique in 2005 and 2015. Public Health Nutr. 2019, 22, 3118–3126. [Google Scholar] [CrossRef] [PubMed]
- Tulsidás, S.; Fontes, F.; Brandão, M.; Lunet, N.; Carrilho, C. Oncology in Mozambique: Overview of the Diagnostic, Treatment, and Research Capacity. Cancers 2023, 15, 1163. [Google Scholar] [CrossRef]
- Julius Chacha, M.; Brian, G. Poverty and Cardiovascular Diseases in Sub-Saharan Africa. In Lifestyle and Epidemiology; Kotsedi, D.M., Han, C.G.K., Eds.; IntechOpen: Rijeka, Croatia, 2021; p. Ch. 2. [Google Scholar]
- Jessen, N.; Damasceno, A.; Silva-Matos, C.; Tuzine, E.; Madede, T.; Mahoque, R.; Padrão, P.; Mbofana, F.; Polónia, J.; Lunet, N. Hypertension in Mozambique: Trends between 2005 and 2015. J. Hypertens. 2018, 36, 779–784. [Google Scholar] [CrossRef]
- Instituto Nacional de Estatística. III Recenseamento Geral da População 2007. Available online: http://www.ine.gov.mz/operacoes-estatisticas/censos/censo-2007/rgph-2007 (accessed on 3 February 2023).
- World Health Organization. The STEPS Instrument and Support Materials. Available online: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps/instrument (accessed on 3 February 2023).
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2011.
- World Health Organization. Guideline for the Pharmacological Treatment of Hypertension in Adults: Summary 2022. Available online: https://apps.who.int/iris/bitstream/handle/10665/344424/9789240033986-eng.pdf (accessed on 7 February 2023).
- Chido-Amajuoyi, O.G.; Fueta, P.; Mantey, D. Age at Smoking Initiation and Prevalence of Cigarette Use Among Youths in Sub-Saharan Africa, 2014–2017. JAMA Network Open 2021, 4, e218060. [Google Scholar] [CrossRef]
- Nansseu, J.R.; Kameni, B.S.; Assah, F.K.; Bigna, J.J.; Petnga, S.-J.; Tounouga, D.N.; Ndoula, S.T.; Noubiap, J.J.; Kamgno, J. Prevalence of major cardiovascular disease risk factors among a group of sub-Saharan African young adults: A population-based cross-sectional study in Yaoundé, Cameroon. BMJ Open 2019, 9, e029858. [Google Scholar] [CrossRef]
- Fagbamigbe, A.F.; Desai, R.; Sewpaul, R.; Kandala, N.-B.; Sekgala, D.; Reddy, P. Age at the onset of tobacco smoking in South Africa: A discrete-time survival analysis of the prognostic factors. Arch. Public Health 2020, 78, 128. [Google Scholar] [CrossRef]
- Ayman, T.; Ameen, T. The role of social media in influencing smoking among Youths. J. Econ. Bus. Stud. 2020, 3, 1–4. [Google Scholar]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Gakidou, E.; Afshin, A.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulle, A.M.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national comparative risk assessment of 84 behavioural environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1345–1422. [Google Scholar] [CrossRef] [PubMed]
- Filby, S.; van Walbeek, C. Cigarette Prices and Smoking Among Youth in 16 African Countries: Evidence from the Global Youth Tobacco Survey. Nicotine Tob. Res. 2022, 24, 1218–1227. [Google Scholar] [CrossRef] [PubMed]
- Cabo, F.; Nunues, A. Mozambique 2020 Tobacco Industry Interference Index 2020. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjqkuyHha79AhUsh_0HHWWHCyUQFnoECBMQAQ&url=https%3A%2F%2Fglobaltobaccoindex.org%2Fdownload%2F1443&usg=AOvVaw0EOjlIyNGlVJ8l1p0QY2LJ (accessed on 24 February 2023).
- World Health Organization. 2021 Global Progress Report on Implementation of the WHO Framework Convention on Tobacco Control. Available online: https://apps.who.int/iris/rest/bitstreams/1409824/retrieve (accessed on 27 February 2023).
- Bryazka, D.; Reitsma, M.B.; Griswold, M.G.; Abate, K.H.; Abbafati, C.; Abbasi-Kangevari, M.; Abbasi-Kangevari, Z.; Abdoli, A.; Abdollahi, M.; Abdullah, A.Y.M.; et al. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: A systematic analysis for the Global Burden of Disease Study 2020. Lancet 2022, 400, 185–235. [Google Scholar] [CrossRef]
- Takahashi, R.; Wilunda, C.; Magutah, K.; Mwaura-Tenambergen, W.; Wilunda, B.; Perngparn, U. Correlates of alcohol consumption in rural western Kenya: A cross-sectional study. BMC Psychiatry 2017, 17, 175. [Google Scholar] [CrossRef]
- Owolabi, E.O.; Goon, D.T.; Adeniyi, O.V.; Seekoe, E. Adult binge drinking: Rate, frequency and intensity in Buffalo City Metropolitan Municipality, South Africa. S. Afr. Fam. Pract. 2018, 60, 46–52. [Google Scholar] [CrossRef]
- Kendagor, A.; Gathecha, G.; Ntakuka, M.W.; Nyakundi, P.; Gathere, S.; Kiptui, D.; Abubakar, H.; Ombiro, O.; Juma, P.; Ngaruiya, C. Prevalence and determinants of heavy episodic drinking among adults in Kenya: Analysis of the STEPwise survey, 2015. BMC Public Health 2018, 18, 1216. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2019.
- Mukoma, G.; Wrottesley, S.V.; Kagura, J.; Oni, T.; Micklesfield, L.; Norris, S.A. The relationships between socioeconomic status, dietary knowledge and patterns, and physical activity with adiposity in urban South African women. S. Afr. J. Clin. Nutr. 2022, 36, 56–62. [Google Scholar] [CrossRef]
- Gallina, A.; Chidiamassamba, C. Gender Aware Approaches in Agricultural Programmes—Mozambique Country Report; SIDA: Stockholm, Sweden, 2010; Available online: https://cdn.sida.se/publications/files/sida61282en-gender-aware-approaches-in-agricultural-programmes-mozambique-country-report.pdf (accessed on 27 February 2023).
- Lear, S.A.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R.; et al. The effect of physical activity on mortality and cardiovascular disease in 130,000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
- Macicame, I.; Prista, A.; Parhofer, K.G.; Cavele, N.; Manhiça, C.; Nhachungue, S.; Saathoff, E.; Rehfuess, E. Social determinants and behaviors associated with overweight and obesity among youth and adults in a peri-urban area of Maputo City, Mozambique. J. Glob. Health 2021, 11, 04021. [Google Scholar] [CrossRef] [PubMed]
- Kanter, R.; Caballero, B. Global Gender Disparities in Obesity: A Review. Adv. Nutr. 2012, 3, 491–498. [Google Scholar] [CrossRef]
- Kapoor, N.; Arora, S.; Kalra, S. Gender Disparities in People Living with Obesity—An Unchartered Territory. J. Midlife Health 2021, 12, 103–107. [Google Scholar] [PubMed]
- Popkin, B.M.; Adair, L.S.; Ng, S.W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 2012, 70, 3–21. [Google Scholar] [CrossRef]
- Gomes, A.; Damasceno, A.; Azevedo, A.; Prista, A.; Silva-Matos, C.; Saranga, S.; Lunet, N. Body mass index and waist circumference in Mozambique: Urban/rural gap during epidemiological transition. Obes. Rev. 2010, 11, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Bermudez, V.; Salazar, J.; Martínez, M.S.; Olivar, L.C.; Nava, M.; Rojas, M.; Ortega, Á.; Añez, R.; Toledo, A.; Rojas, J.; et al. Age-specific waist circumference cutoff-points for abdominal obesity diagnosis: A personalized strategy for a large Venezuelan population. J. Diabetes Metab. Disord. 2021, 20, 217–227. [Google Scholar] [CrossRef]
- Kirschbaum, T.K.; Sudharsanan, N.; Manne-Goehler, J.; De Neve, J.W.; Lemp, J.M.; Theilmann, M.; Marcus, M.E.; Ebert, C.; Chen, S.; Yoosefi, M.; et al. The Association of Socioeconomic Status with Hypertension in 76 Low- and Middle-Income Countries. J. Am. Coll. Cardiol. 2022, 80, 804–817. [Google Scholar] [CrossRef] [PubMed]
- Addo, J.; Smeeth, L.; Leon, D.A. Hypertension In Sub-Saharan Africa. Hypertension 2007, 50, 1012–1018. [Google Scholar] [CrossRef]
- Kayima, J.; Wanyenze, R.K.; Katamba, A.; Leontsini, E.; Nuwaha, F. Hypertension awareness, treatment and control in Africa: A systematic review. BMC Cardiovasc. Disord. 2013, 13, 54. [Google Scholar] [CrossRef]
| Women (n = 488) | Men (n = 288) | |||||
|---|---|---|---|---|---|---|
| n | Unweighted (%) 1 | Weighted (%) 2,3 | n | Unweighted (%) 1 | Weighted (%) 2,3 | |
| Place of residence | ||||||
| Urban | 250 | 51.2 | 44.8 | 162 | 56.3 | 44.2 |
| Rural | 238 | 48.8 | 55.2 | 126 | 43.8 | 55.8 |
| Education (years) | ||||||
| None | 80 | 16.4 | 18.6 | 22 | 7.6 | 7.9 |
| 1–4 | 121 | 24.8 | 28.9 | 47 | 16.3 | 18.6 |
| 5–7 | 68 | 13.9 | 14.8 | 69 | 24.0 | 26.6 |
| 8–10 | 129 | 26.4 | 23.5 | 73 | 25.4 | 25.0 |
| 11–12 | 72 | 14.8 | 11.6 | 61 | 21.2 | 17.7 |
| >12 | 18 | 3.70 | 2.60 | 16 | 5.60 | 4.20 |
| Monthly income (USD/household member aged ≥18 years) | ||||||
| 0–15 | 116 | 29.5 | 32.2 | 76 | 20.5 | 35.2 |
| 16–22 | 81 | 30.6 | 227 | 36 | 14.5 | 17.6 |
| 23–44 | 83 | 21.1 | 19.3 | 48 | 19.3 | 17.8 |
| 45–89 | 60 | 15.3 | 13.8 | 39 | 15.7 | 13.3 |
| ≥90 | 53 | 13.5 | 12.0 | 50 | 20.1 | 16.0 |
| Current Smoking | Current Drinking | Binge Drinking 2 | Not Meeting WHO Recommendation Physical Activity 3 | Vigorous Physical Activity <75 min/Week 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % (95%CI) | OR 1 (95%CI) | % (95%CI) | OR 1 (95%CI) | % (95%CI) | OR 1 (95%CI) | % (95%CI) | OR 1 (95%CI) | % (95%CI) | OR 1 (95%CI) | |
| Sex 5 | ||||||||||
| Women | 0.3 (0.1–1.3) | ref | 8.8 (6.7–11.5) | ref | 29.6 (17.6–45.4) | ref | 8.5 (6.2–11.6) | ref | 45.5 (37.8–53.4) | ref |
| Men | 9.3 (6.2–13.7) | 32.42 (8.21–128.04) | 28.2 (22.6–34.5) | 3.94 (2.61–5.95) | 44.4 (34.0–55.3) | 1.59 (0.61–3.71) | 5.1 (3.1–8.3) | 0.64 (0.34–1.20) | 19.6 (14.7–25.8) | 0.28 (0.18–0.44) |
| Place of residence 5 | ||||||||||
| Rural | 4.6 (2.8–7.3) | ref | 10.7 (7.5–15.2) | ref | 34.7 (20.6–52.1) | ref | 6.1 (4.0–9.2) | ref | 25.7 (19.6–32.9) | ref |
| Urban | 2.8 (1.5–5.2) | 1.00 (0.34–2.90) | 23.0 (17.2–30.0) | 2.36 (1.36–4.10) | 41.9 (32.5–51.8) | 1.59 (0.66–3.84) | 8.6 (6.1–12.1) | 0.84 (0.40–1.77) | 48.2 (39.7–56.9) | 1.91 (1.06–3.45) |
| Education (years) 5 | ||||||||||
| None | 7.4 (3.8–14.3) | ref | 6.9 (3.9–12.2) | ref | 28.7 (8.4–63.8) | ref | 4.3 (1.4–12.7) | ref | 36.1 (23.8–50.5) | ref |
| 1–7 | 4.4 (2.4–8.2) | 0.26 (0.08–0.87) | 13.2 (8.9–19.0) | 1.32 (0.58–2.98) | 43.3 (28.4–59.6) | 1.69 (0.31–9.32) | 6.3 (4.0–9.6) | 2.46 (0.71–8.56) | 28.8 (21.9–36.9) | 0.71 (0.35–1.44) |
| >8 | 1.7 (0.8–3.7) | 0.06 (0.02–0.25) | 22.7 (18.0–28.3) | 1.67 (0.75–3.72) | 37.9 (26.6–50.6) | 1.20 (0.21–6.74) | 9.3 (6.6–13.1) | 3.03 (0.76–12.14) | 42.9 (36.0–50.2) | 1.02 (0.48–2.16) |
| Monthly income (USD/household member aged ≥18 years) 5 | ||||||||||
| 0–15 | 5.3 (2.7–10.0) | ref | 17.3 (12.4–23.5) | ref | 44.3 (26.2–64.0) | ref | 4.5 (4.5–8.1) | ref | 34.0 (25.8–43.6) | ref |
| 16–44 | 4.3 (2.2–8.1) | 0.85 (0.28–2.57) | 16.1 (11.5–22.1) | 0.91 (0.55–1.49) | 33.8 (22.0–48.1) | 0.67 (0.27–1.60) | 6.8 (4.5–10.4) | 1.52 (0.67–3.46) | 33.8 (27.3–40.9) | 0.85 (0.55–1.33) |
| ≥45 | 3.1 (1.4–6.7) | 0.88 (0.28–2.83) | 21.9 (15.7–29.6) | 1.02 (0.58–1.79) | 43.7 (28.4–60.3) | 0.96 (0.33–2.84) | 11.4 (7.5–17.0) | 2.53 (1.08–5.91) | 44.5 (36.4–53.0) | 1.36 (0.83–2.23) |
| Overweight/Obesity 2,3 | Abdominal Obesity 3,4 | Hypertension 5 | ||||
|---|---|---|---|---|---|---|
| % (95%CI) | OR 1 (95%CI) | % (95%CI) | OR 1 (95%CI) | % (95%CI) | OR 1 (95%CI) | |
| Sex 6 | ||||||
| Women | 17.6 (13.0–23.2) | ref | 2.5 (1.3–4.6) | ref | 14.1 (10.8–18.4) | ref |
| Men | 8.6 (4.9–15.0) | 0.43 (0.21–0.87) | --- | --- | 21.0 (14.8–28.9) | 2.09 (1.20–3.63) |
| Place of residence 6 | ||||||
| Rural | 10.7 (7.3–15.4) | ref | 1.1 (0.3–3.5) | ref | 18.0 (13.2–24.1) | ref |
| Urban | 18.0 (12.8–24.5) | 1.57 (0.73- 3.39) | 1.9 (1.0–3.7) | 1.20 (0.35–4.10) | 15.0 (11.2–20.0) | 0.97 (0.49–1.93) |
| Education (years) 6 | ||||||
| None | 9.8 (4.8–19.2) | ref | 2.3 (0.5–8.5) | ref | 24.4 (16.1–35.0) | ref |
| 1–7 | 11.7 (7.1–18.5) | 1.07 (0.40–2.86) | 0.7 (0.2–2.2) | 0.29 (0.09–0.93) | 18.1 (13.4–24.1) | 0.41 (0.19–0.89) |
| >8 | 17.6 (13.0–23.5) | 1.26 (0.41–3.87) | 2.0 (1.1–3.9) | 0.76 (0.21–2.79) | 12.5 (8.4–18.0) | 0.24 (0.11–0.54) |
| Monthly income (USD/household member aged ≥18 years) 6 | ||||||
| 0–15 | 10.8 (6.6–17.4) | ref | 0.8 (0.1–5.8) | ref | 14.3 (9.4–21.0) | ref |
| 16–44 | 15.0 (10.3–21.2) | 1.29 (0.67–2.48) | 2.3 (1.2–4.6) | 2.58 (0.44–15.26) | 21.0 (14.9–28.5) | 1.75 (0.97–3.18) |
| ≥45 | 20.2 (14.0–28.3) | 1.84 (0.95–3.57) | 2.1 (0.8–5.1) | 2.47 (0.37–16.71) | 17.3 (11.9–24.6) | 1.65 (0.92–2.97) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, I.; Damasceno, A.; Fontes, F.; Araújo, N.; Prista, A.; Jessen, N.; Padrão, P.; Silva-Matos, C.; Lunet, N. Prevalence of Cardiovascular Risk Factors among Young Adults (18–25 Years) in Mozambique. J. Cardiovasc. Dev. Dis. 2023, 10, 298. https://doi.org/10.3390/jcdd10070298
Silva I, Damasceno A, Fontes F, Araújo N, Prista A, Jessen N, Padrão P, Silva-Matos C, Lunet N. Prevalence of Cardiovascular Risk Factors among Young Adults (18–25 Years) in Mozambique. Journal of Cardiovascular Development and Disease. 2023; 10(7):298. https://doi.org/10.3390/jcdd10070298
Chicago/Turabian StyleSilva, Isa, Albertino Damasceno, Filipa Fontes, Natália Araújo, António Prista, Neusa Jessen, Patrícia Padrão, Carla Silva-Matos, and Nuno Lunet. 2023. "Prevalence of Cardiovascular Risk Factors among Young Adults (18–25 Years) in Mozambique" Journal of Cardiovascular Development and Disease 10, no. 7: 298. https://doi.org/10.3390/jcdd10070298
APA StyleSilva, I., Damasceno, A., Fontes, F., Araújo, N., Prista, A., Jessen, N., Padrão, P., Silva-Matos, C., & Lunet, N. (2023). Prevalence of Cardiovascular Risk Factors among Young Adults (18–25 Years) in Mozambique. Journal of Cardiovascular Development and Disease, 10(7), 298. https://doi.org/10.3390/jcdd10070298









