Enhanced Nutritional and Functional Recovery in Femur Fracture Patients Post-Surgery: Preliminary Evidence of Muscle-Targeted Nutritional Support in Real-World Practice
Abstract
1. Introduction
2. Materials and Methods
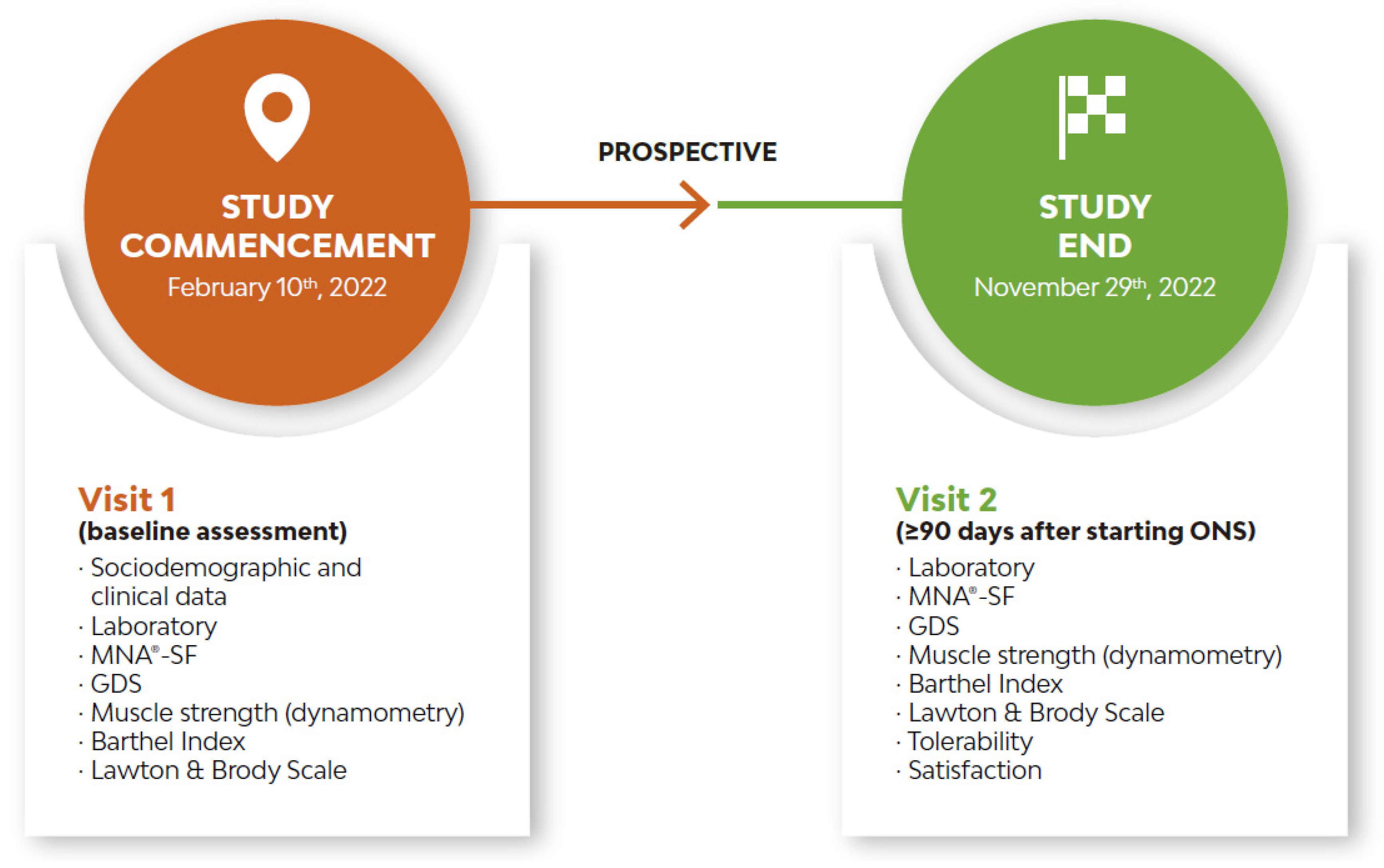
2.1. Design
2.2. Study Population
2.3. Oral Nutritional Supplementation
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Baseline Demographic and Clinical Characteristics at Visit 1
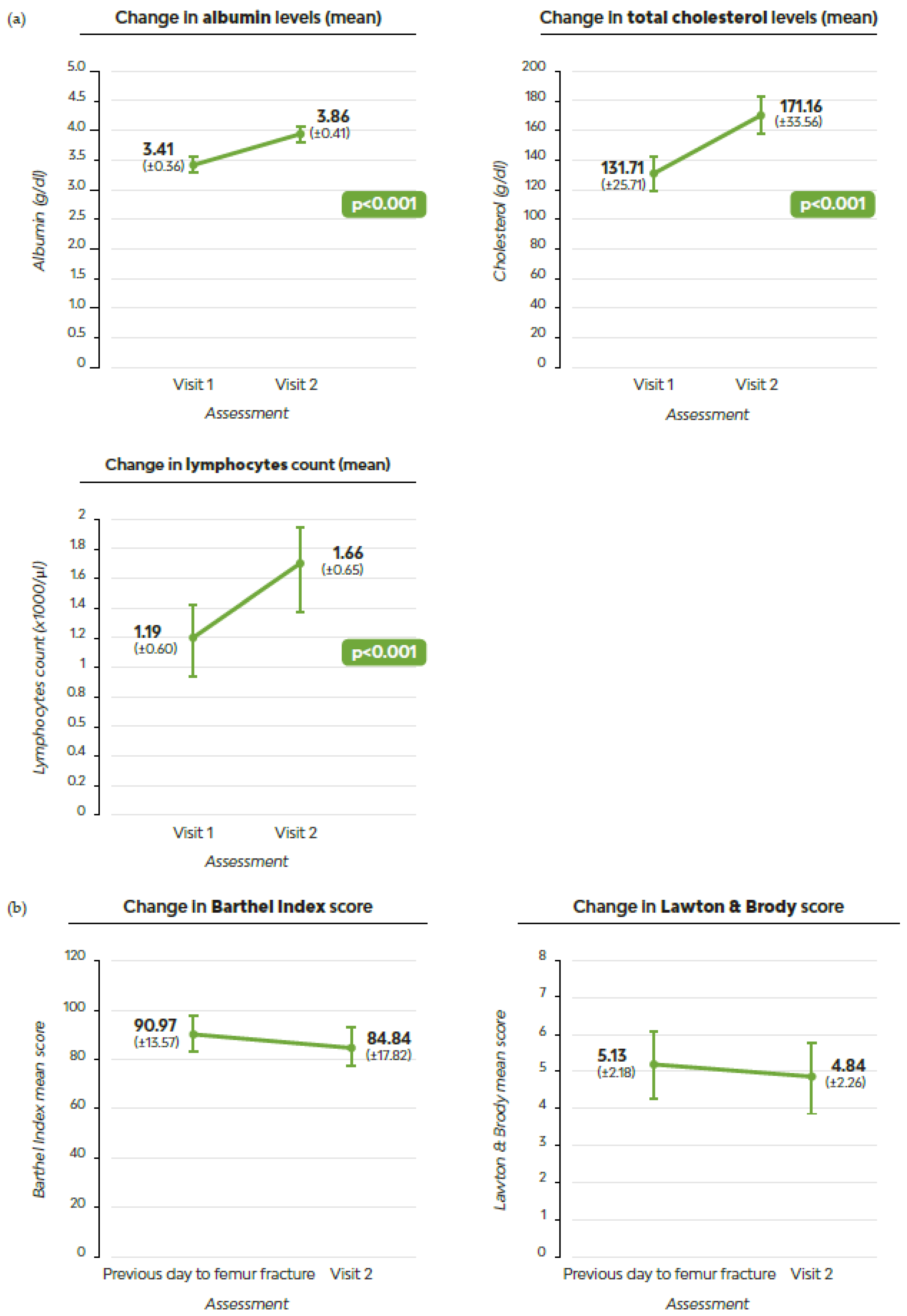
3.2. Clinical Characteristics at Visit 2
3.3. Drivers of Changes in Nutritional Status
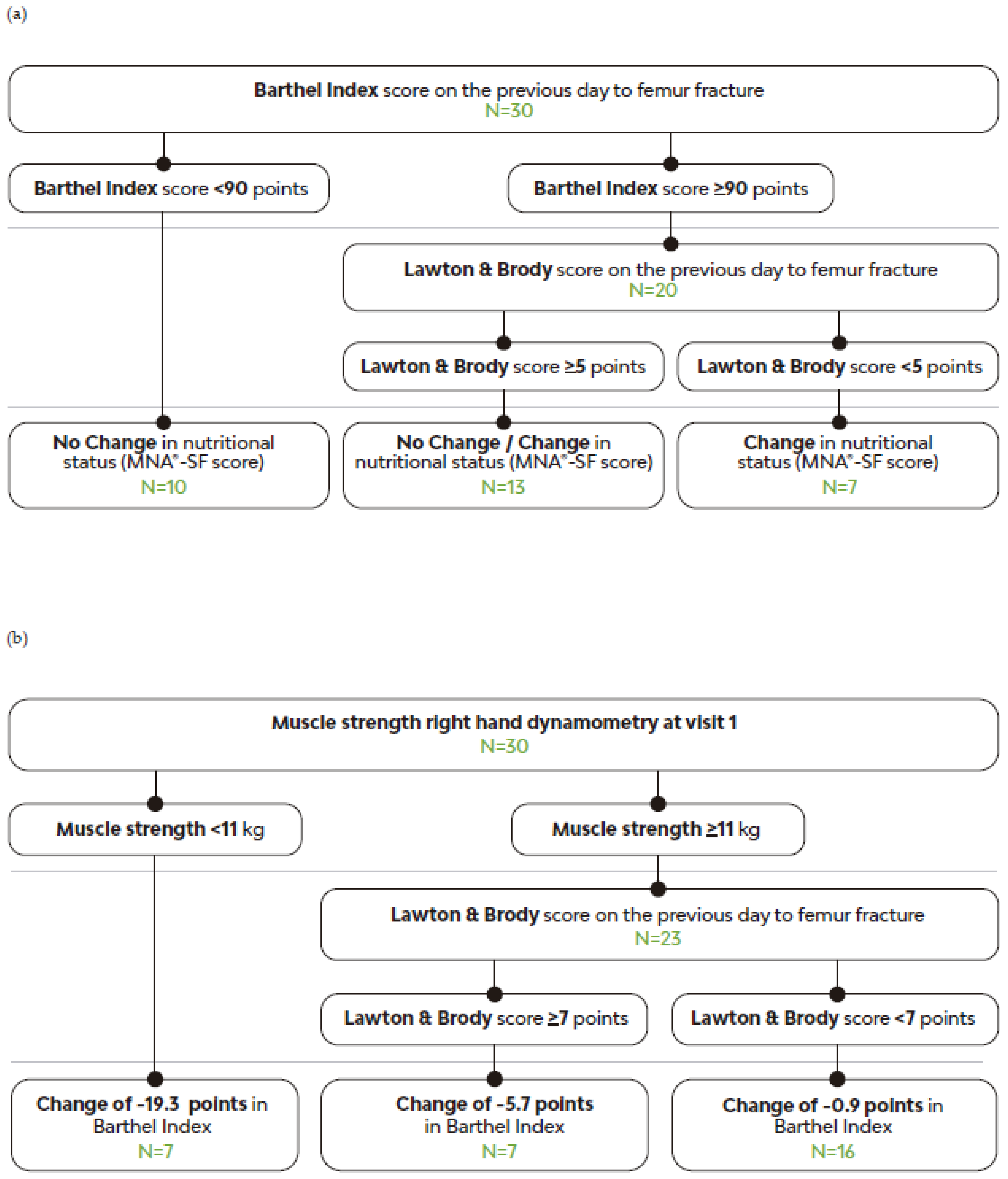
3.4. Factors Predicting Nutritional Improvement with MT-ONS
3.5. Drivers of Changes in Independence to Perform Activities of Daily Living
3.6. Factors Predicting Independent Functionality Improvement with MT-ONS
3.7. Tolerability and Satisfaction with the MT-ONS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Middleton, R.; Poveda, J.L.; Orfila Pernas, F.; Martinez Laguna, D.; Diez Perez, A.; Nogués, X.; Carbonell Abella, C.; Reyes, C.; Prieto-Alhambra, D. Mortality, Falls, and Fracture Risk Are Positively Associated with Frailty: A SIDIAP Cohort Study of 890,000 Patients. J. Gerontol. Ser. A 2022, 77, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Azagra, R.; López-Expósito, F.; Martin-Sánchez, J.C.; Aguyé, A.; Moreno, N.; Cooper, C.; Díez-Pérez, A.; Dennison, E.M. Changing trends in the epidemiology of hip fracture in Spain. Osteoporos. Int. 2014, 25, 1267–1274. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Reig, J.; Salvador Marín, J.; Pérez Alba, J.M.; Ferrández Martínez, J.; Orozco Beltrán, D.; Martínez López, J.F. Risk factors for in-hospital mortality following hip fracture. Rev. Esp. Cir. Ortop. Traumatol. 2017, 61, 209–215. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Reig, J.; Salvador Marín, J.; Ferrández Martínez, J.; Orozco Beltrán, D.; Martínez López, J.F.; Quesada Rico, J.A. Prognostic factors and predictive model for in-hospital mortality following hip fractures in the elderly. Chin. J. Traumatol. 2018, 21, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Dyer, S.M.; Crotty, M.; Fairhall, N.; Magaziner, J.; Beaupre, L.A.; Cameron, I.D.; Sherrington, C. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016, 16, 158. [Google Scholar] [CrossRef]
- Orive, M.; Anton-Ladislao, A.; García-Gutiérrez, S.; Las Hayas, C.; González, N.; Zabala, J.; Quintana, J.M. Prospective study of predictive factors of changes in pain and hip function after hip fracture among the elderly. Osteoporos. Int. 2016, 27, 527–536. [Google Scholar] [CrossRef]
- Kurkcu, M.; Meijer, R.I.; Lonterman, S.; Muller, M.; de van der Schueren, M.A.E. The association between nutritional status and frailty characteristics among geriatric outpatients. Clin. Nutr. ESPEN 2018, 23, 112–116. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Foo, M.X.E.; Wong, G.J.Y.; Lew, C.C.H. A systematic review of the malnutrition prevalence in hospitalized hip fracture patients and its associated outcomes. JPEN J. Parenter. Enter. Nutr. 2021, 45, 1141–1152. [Google Scholar] [CrossRef]
- Chiavarini, M.; Ricciotti, G.M.; Genga, A.; Faggi, M.I.; Rinaldi, A.; Toscano, O.D.; D’Errico, M.M.; Barbadoro, P. Malnutrition-Related Health Outcomes in Older Adults with Hip Fractures: A Systematic Review and Meta-Analysis. Nutrients 2024, 16, 1069. [Google Scholar] [CrossRef]
- Rempel, A.N.; Rigassio Radler, D.L.; Zelig, R.S. Effects of the use of oral nutrition supplements on clinical outcomes among patients who have undergone surgery for hip fracture: A literature review. Nutr. Clin. Pract. 2023, 38, 775–789. [Google Scholar] [CrossRef] [PubMed]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.; Sobotka, L.; et al. ESPEN practical guideline: Clinical nutrition and hydration in geriatrics. Clin. Nutr. 2022, 41, 958–989. [Google Scholar] [CrossRef] [PubMed]
- Campbell, W.W.; Deutz, N.E.P.; Volpi, E.; Apovian, C.M. Nutritional Interventions: Dietary Protein Needs and Influences on Skeletal Muscle of Older Adults. J. Gerontol. Ser. A 2023, 78, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Yao, P.; Bennett, D.; Mafham, M.; Lin, X.; Chen, Z.; Armitage, J.; Clarke, R. Vitamin D and Calcium for the Prevention of Fracture: A Systematic Review and Meta-analysis. JAMA Netw. Open 2019, 2, e1917789. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Fu, X.; Hu, Q.; Chen, L.; Zuo, H. The Effect of Leucine Supplementation on Sarcopenia-Related Measures in Older Adults: A Systematic Review and Meta-Analysis of 17 Randomized Controlled Trials. Front. Nutr. 2022, 9, 929891. [Google Scholar] [CrossRef]
- Cereda, E.; Pisati, R.; Rondanelli, M.; Caccialanza, R. Whey Protein, Leucine- and Vitamin-D-Enriched Oral Nutritional Supplementation for the Treatment of Sarcopenia. Nutrients 2022, 14, 1524. [Google Scholar] [CrossRef]
- Arkley, J.; Dixon, J.; Wilson, F.; Charlton, K.; Ollivere, B.J.; Eardley, W. Assessment of Nutrition and Supplementation in Patients With Hip Fractures. Geriatr. Orthop. Surg. Rehabil. 2019, 10, 2151459319879804. [Google Scholar] [CrossRef]
- Dempewolf, S.; Mouser, B.; Rupe, M.; Owen, E.C.; Reider, L.; Willey, M.C. What Are the Barriers to Incorporating Nutrition Interventions Into Care of Older Adults With Femoral Fragility Fractures? Iowa Orthop. J. 2023, 43, 172–182. [Google Scholar]
- Guigoz, Y.; Vellas, B.; Garry, P.J. Assessing the nutritional status of the elderly: The Mini Nutritional Assessment as part of the geriatric evaluation. Nutr. Rev. 1996, 54, S59–S65. [Google Scholar] [CrossRef]
- Molina-Luque, R.; Muñoz Díaz, B.; de la Iglesia, J.; Romero-Saldaña, M.; Molina-Recio, G. Is the Spanish short version of Mini Nutritional Assessment (MNA-SF) valid for nutritional screening of the elderly? Nutr. Hosp. Hosp. 2019, 36, 290–295. [Google Scholar]
- Ignacio de Ulíbarri, J.; González-Madroño, A.; de Villar, N.G.P.; González, P.; González, B.; Mancha, A.; Rodríguez, F.; Fernández, G. CONUT: A tool for controlling nutritional status. First validation in a hospital population. Nutr. Hosp. 2005, 20, 38–45. [Google Scholar] [PubMed]
- Cabañero-Martínez, M.J.; Cabrero-García, J.; Richart-Martínez, M.; Muñoz-Mendoza, C.L. Structured review of activities of daily living measures in older people. Rev. Esp. Geriatr. Gerontol. 2008, 43, 271–283. [Google Scholar] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Reisberg, B.; Ferris, S.H.; de Leon, M.J.; Crook, T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am. J. Psychiatry 1982, 139, 1136–1139. [Google Scholar]
- Lemon, S.C.; Roy, J.; Clark, M.A.; Friedmann, P.D.; Rakowski, W. Classification and regression tree analysis in public health: Methodological review and comparison with logistic regression. Ann. Behav. Med. A Publ. Soc. Behav. Med. 2003, 26, 172–181. [Google Scholar] [CrossRef]
- Jaehn, P.; Fügemann, H.; Gödde, K.; Holmberg, C. Using decision tree analysis to identify population groups at risk of subjective unmet need for assistance with activities of daily living. BMC Geriatr. 2023, 23, 543. [Google Scholar] [CrossRef]
- Sánchez-Torralvo, F.J.; Pérez-Del-Río, V.; García-Olivares, M.; Porras, N.; Abuín-Fernández, J.; Bravo-Bardají, M.F.; García-de-Quevedo, D.; Olveira, G. Global Subjective Assessment and Mini Nutritional Assessment Short Form Better Predict Mortality Than GLIM Malnutrition Criteria in Elderly Patients with Hip Fracture. Nutrients 2023, 15, 1828. [Google Scholar] [CrossRef]
- Malafarina, V.; Uriz-Otano, F.; Malafarina, C.; Martinez, J.A.; Zulet, M.A. Effectiveness of nutritional supplementation on sarcopenia and recovery in hip fracture patients. A multi-centre randomized trial. Maturitas 2017, 101, 42–50. [Google Scholar] [CrossRef]
- Solsona Fernández, S.; Caverni Muñoz, A.; Labari Sanz, G.; Monterde Hernandez, B.; Martínez Marco, M.A.; Mesa Lampré, P. Preliminary Evidence on the Effectiveness of a Multidisciplinary Nutritional Support for Older People with Femur Fracture at an Orthogeriatric Unit in Spain. J. Nutr. Gerontol. Geriatr. 2022, 41, 270–293. [Google Scholar] [CrossRef] [PubMed]
- Wyers, C.E.; Reijven, P.L.M.; Breedveld-Peters, J.J.L.; Denissen, K.F.M.; Schotanus, M.G.M.; van Dongen, M.C.J.M.; Eussen, S.J.P.M.; Heyligers, I.C.; van den Brandt, P.A.; Willems, P.C.; et al. Efficacy of Nutritional Intervention in Elderly After Hip Fracture: A Multicenter Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 1429–1437. [Google Scholar] [CrossRef] [PubMed]
- Ashkenazi, I.; Rotman, D.; Amzalleg, N.; Graif, N.; Khoury, A.; Ben-Tov, T.; Steinberg, E. Efficacy of Oral Nutritional Supplements in Patients Undergoing Surgical Intervention for Hip Fracture. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221102252. [Google Scholar] [CrossRef] [PubMed]
- Di Monaco, M.; Castiglioni, C.; Bardesono, F.; Milano, E.; Massazza, G. The handgrip strength threshold of 16 kg discriminates successful rehabilitation: A prospective short-term study of 258 women with hip fracture. Arch. Gerontol. Geriatr. 2020, 91, 104190. [Google Scholar] [CrossRef]
- Meskers, C.G.M.; Reijnierse, E.M.; Numans, S.T.; Kruizinga, R.C.; Pierik, V.D.; van Ancum, J.M.; Slee-Valentijn, M.; Scheerman, K.; Verlaan, S.; Maier, A.B. Association of Handgrip Strength and Muscle Mass with Dependency in (Instrumental) Activities of Daily Living in Hospitalized Older Adults -The EMPOWER Study. J. Nutr. Health Aging 2019, 23, 232–238. [Google Scholar] [CrossRef]
- Wang, D.X.M.; Yao, J.; Zirek, Y.; Reijnierse, E.M.; Maier, A.B. Muscle mass, strength, and physical performance predicting activities of daily living: A meta-analysis. J. Cachexia Sarcopenia Muscle 2020, 11, 3–25. [Google Scholar] [CrossRef]
- Mithal, A.; Bonjour, J.P.; Boonen, S.; Burckhardt, P.; Degens, H.; El Hajj Fuleihan, G.; Josse, R.; Lips, P.; Morales Torres, J.; Rizzoli, R.; et al. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos. Int. 2013, 24, 1555–1566. [Google Scholar] [CrossRef]
- Laudisio, A.; Giovannini, S.; Finamore, P.; Loreti, C.; Vannetti, F.; Coraci, D.; Incalzi, R.A.; Zuccal, G.; Macchi, C.; Padua, L.; et al. Muscle strength is related to mental and physical quality of life in the oldest old. Arch. Gerontol. Geriatr. 2020, 89, 104109. [Google Scholar] [CrossRef]
- Verlaan, S.; Maier, A.B.; Bauer, J.M.; Bautmans, I.; Brandt, K.; Donini, L.M.; Maggio, M.; McMurdo, M.E.T.; Mets, T.; Seal, C.; et al. Sufficient levels of 25-hydroxyvitamin D and protein intake required to increase muscle mass in sarcopenic older adults—The PROVIDE study. Clin. Nutr. 2018, 37, 551–557. [Google Scholar] [CrossRef]
- Landi, F.; Calvani, R.; Tosato, M.; Martone, A.M.; Ortolani, E.; Savera, G.; D’Angelo, E.; Sisto, A.; Marzetti, E. Protein Intake and Muscle Health in Old Age: From Biological Plausibility to Clinical Evidence. Nutrients 2016, 8, 295. [Google Scholar] [CrossRef]
- Baum, J.I.; Wolfe, R.R. The Link between Dietary Protein Intake, Skeletal Muscle Function and Health in Older Adults. Healthc 2015, 3, 529–543. [Google Scholar] [CrossRef] [PubMed]
- Cereda, E.; Veronese, N.; Caccialanza, R. Role of muscle-targeted nutritional therapy: New data. Curr. Opin. Clin. Nutr. Metab. Care 2022, 25, 142–153. [Google Scholar] [CrossRef] [PubMed]
- González-Zabaleta, J.; Pita-Fernandez, S.; Seoane-Pillado, T.; López-Calviño, B.; Gonzalez-Zabaleta, J.L. Dependence for basic and instrumental activities of daily living after hip fractures. Arch. Gerontol. Geriatr. 2015, 60, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Alhambra, D.; Moral-Cuesta, D.; Palmer, A.; Aguado-Maestro, I.; Bardaji, M.F.B.; Brañas, F.; Bueno, G.A.; Caeiro-Rey, J.R.; Cano, I.A.; Barres-Carsi, M.; et al. The impact of hip fracture on health-related quality of life and activities of daily living: The SPARE-HIP prospective cohort study. Arch. Osteoporos. 2019, 14, 56. [Google Scholar] [CrossRef] [PubMed]
- Knauf, T.; Buecking, B.; Hack, J.; Barthel, J.; Bliemel, C.; Aigner, R.; Ruchholtz, S.; Eschbach, D. Development of the Barthel Index 5 years after hip fracture: Results of a prospective study. Geriatr. Gerontol. Int. 2019, 19, 809–814. [Google Scholar] [CrossRef]
- Motamed-Jahromi, M.; Kaveh, M.H. Effective Interventions on Improving Elderly’s Independence in Activity of Daily Living: A Systematic Review and Logic Model. Front. Public Health 2020, 8, 516151. [Google Scholar] [CrossRef]
- Inoue, T.; Misu, S.; Tanaka, T.; Sakamoto, H.; Iwata, K.; Chuman, Y.; Ono, R. Pre-fracture nutritional status is predictive of functional status at discharge during the acute phase with hip fracture patients: A multicenter prospective cohort study. Clin. Nutr. 2017, 36, 1320–1325. [Google Scholar] [CrossRef]
- Dakhil, S.; Saltvedt, I.; Benth, J.Š.; Thingstad, P.; Watne, L.O.; Bruun Wyller, T.; Helbostad, J.L.; Frihagen, F.; Johnsen, L.G.; Taraldsen, K. Longitudinal trajectories of functional recovery after hip fracture. PLoS ONE 2023, 18, e0283551. [Google Scholar] [CrossRef]
- Ramírez-García, E.; García de la Torre, G.S.; Rodríguez Reyes, E.J.; Moreno-Tamayo, K.; Espinel-Bermudez, M.C.; Sánchez-García, S. Factors Associated with Recovered Functionality After Hip Fracture in Non-Institutionalized Older Adults: A Case-Control Study Nested in a Cohort. Clin. Interv. Aging 2021, 16, 1515–1525. [Google Scholar] [CrossRef]
- Serra-Prat, M.; Sist, X.; Saiz, A.; Jurado, L.; Domenich, R.; Roces, A.; Papiol, M. Clinical and Functional Characterization of Pre-frailty among Elderly Patients Consulting Primary Care Centres. J. Nutr. Health Aging 2016, 20, 653–658. [Google Scholar] [CrossRef]
- Consejería de Sanidad de la Comunidad de Madrid. Plan de Atención Integral a la Fragilidad y Promoción de la Longevidad Saludable en Personas Mayores de la Comunidad de Madrid 2022–2025; Consejería de Sanidad de la Comunidad de Madrid: Madrid, Spain, 2022; pp. 1–165. [Google Scholar]

| Characteristics | |
|---|---|
| Age, years (±SD) | 87 (±3.9) |
| Gender | |
| Female, n (%) | 23 (74%) |
| Male, n (%) | 8 (26%) |
| Marital status | |
| Single, n (%) | 0 (0%) |
| In a relationship, n (%) | 0 (0%) |
| Married, n (%) | 7 (23%) |
| Divorced, n (%) | 0 (0%) |
| Widow, n (%) | 24 (77%) |
| Habitual residence location | |
| Home, alone without a contracted caregiver, n (%) | 13 (42%) |
| Home, alone with a contracted caregiver, n (%) | 12 (36%) |
| Home, with a family member, n (%) | 5 (16%) |
| Home, with a family member and a contracted caregiver, n (%) | 1 (3%) |
| Home of a family member, relative or friend, n (%) | 1 (3%) |
| Institution | 0 (0%) |
| Residence location at hospital discharge | |
| Habitual residence | 24 (78%) |
| Habitual institution | 1 (3%) |
| Intermediate care centre | 6 (19%) |
| Nursing home | 0 (0%) |
| Others | 0 (0%) |
| Characteristics | Visit 1 | Visit 2 |
|---|---|---|
| Type of fracture | ||
| Trochanteric | 21 (68%) | - |
| Sub-trochanteric | 1 (3%) | - |
| Sub-capital | 9 (29%) | - |
| MNA®-SF score | ||
| 12–14 points, well-nourished, n (%) | 1 (3%) | 10 (32%) |
| 8–11 points, at risk of malnutrition, n (%) | 20 (65%) | 17 (55%) |
| 0–7 points, malnourished, n (%) | 10 (32%) | 4 (13%) |
| Laboratory parameters | ||
| Serum albumin levels (g/dL) mean (±SD) | 3.4 (±0.36) | 3.9 (±0.41) |
| Cholesterol levels (md/dL) mean (±SD) | 131.7 (±25.71) | 171.2 (±33.56) |
| Lymphocyte count (×1000/µL) mean (±SD) | 1.2 (±0.60) | 1.7 (±0.65) |
| CONUT® | ||
| 9–12 points, high risk of malnutrition, n (%) | 1 (3%) | 0 (0%) |
| 5–8 points, moderate risk of malnutrition, n (%) | 13 (42%) | 1 (3%) |
| 0–4 points, low risk of malnutrition, n (%) | 17 (55%) | 30 (97%) |
| Weight, kg (SD) | 60.4 (±9.9) | 62.4 (±9.2) |
| Muscle strength right hand, kg (SD) | 15.7 (±5.0) | 17.1 (±5.1) |
| Muscle strength left hand, kg (SD) | 14.2 (±5.1) | 15.1 (±4.2) |
| Cognitive status | ||
| GDS 1: no cognitive decline, n (%) | 21 (67.7%) | 21 (67.7%) |
| GDS 2: very mild cognitive decline, n (%) | 2 (6.5%) | 3 (9.7) |
| GDS 3: mild cognitive decline, n (%) | 5 (16.1%) | 5 (16.1%) |
| GDS 4: moderate cognitive decline, n (%) | 3 (9.7%) | 2 (6.5%) |
| GDS 5: moderately severe cognitive decline, n (%) | 0% (0) | 0% (0) |
| GDS 6: severe cognitive decline, n (%) | 0% (0) | 0% (0) |
| GDS 7: very severe cognitive decline, n (%) | 0% (0) | 0% (0) |
| Barthel Index score (previous day to femur fracture) | ||
| 100 points (independent in the daily activities), n (%) | 15 (48.4%) | 13 (41.9%) |
| 60–95 points (needs minimal help with daily activities), n (%) | 15 (48.4%) | 14 (45.2%) |
| 45–55 points (partially dependant), n (%) | 1 (3.2%) | 4 (12.9%) |
| 20–40 points (very dependant), n (%) | 0 (0%) | 0 (0%) |
| <20 points (totally dependent), n (%) | 0 (0%) | 0 (0%) |
| Lawton and Brody scale scores (previous day to femur fracture) | ||
| 0–1 point (totally dependent), n (%) | 1 (3.2%) | 0 (0%) |
| 2–3 points (very dependant), n (%) | 7 (22.6%) | 12 (38.7%) |
| 4–5 points (partially dependant), n (%) | 11 (35.5%) | 8 (25.8%) |
| 6–7 points (low dependence), n (%) | 3 (9.7%) | 3 (9.7%) |
| 8 points (independent), n (%) | 9 (29.0%) | 8 (25.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soria Perdomo, F.J.; Fernández Villaseca, S.; Zaragoza Brehcist, C.; García Gómez, E. Enhanced Nutritional and Functional Recovery in Femur Fracture Patients Post-Surgery: Preliminary Evidence of Muscle-Targeted Nutritional Support in Real-World Practice. Geriatrics 2024, 9, 153. https://doi.org/10.3390/geriatrics9060153
Soria Perdomo FJ, Fernández Villaseca S, Zaragoza Brehcist C, García Gómez E. Enhanced Nutritional and Functional Recovery in Femur Fracture Patients Post-Surgery: Preliminary Evidence of Muscle-Targeted Nutritional Support in Real-World Practice. Geriatrics. 2024; 9(6):153. https://doi.org/10.3390/geriatrics9060153
Chicago/Turabian StyleSoria Perdomo, Francisco José, Sara Fernández Villaseca, Cristina Zaragoza Brehcist, and Elena García Gómez. 2024. "Enhanced Nutritional and Functional Recovery in Femur Fracture Patients Post-Surgery: Preliminary Evidence of Muscle-Targeted Nutritional Support in Real-World Practice" Geriatrics 9, no. 6: 153. https://doi.org/10.3390/geriatrics9060153
APA StyleSoria Perdomo, F. J., Fernández Villaseca, S., Zaragoza Brehcist, C., & García Gómez, E. (2024). Enhanced Nutritional and Functional Recovery in Femur Fracture Patients Post-Surgery: Preliminary Evidence of Muscle-Targeted Nutritional Support in Real-World Practice. Geriatrics, 9(6), 153. https://doi.org/10.3390/geriatrics9060153






