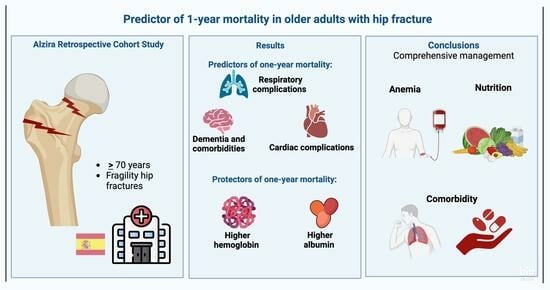
Respiratory Complications Are the Main Predictors of 1-Year Mortality in Patients with Hip Fractures: The Results from the Alzira Retrospective Cohort Study
Abstract
1. Introduction
2. Methods
2.1. Scope and Population
2.2. Eligibility Criteria
2.3. Sample Size
2.4. Intervention
2.5. Study Variables
2.6. Statistical Analysis
2.7. Ethical Considerations
3. Results
3.1. Descriptive and Bivariate Analyses
3.2. Multivariate Cox Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sáez-López, P.; Ojeda-Thies, C.; Alarcón, T.; Muñoz Pascual, A.; Mora-Fernández, J.; González de Villaumbrosia, C.; Molina Hernández, M.J.; Montero-Fernández, N.; Cancio Trujillo, J.M.; Díez Pérez, A.; et al. Spanish National Hip Fracture Registry (RNFC): First-year results and comparison with other registries and prospective multi-centric studies from Spain. Rev. Esp. Salud Publica 2019, 93, e201911072. [Google Scholar]
- Nishimura, Y.; Inagaki, Y.; Noda, T.; Nishioka, Y.; Myojin, T.; Ogawa, M.; Kido, A.; Imamura, T.; Tanaka, Y. Risk factors for mortality after hip fracture surgery in Japan using the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Arch. Osteoporos. 2023, 18, 91. [Google Scholar] [CrossRef]
- de Miguel Artal, M.; Roca Chacón, O.; Martínez-Alonso, M.; Serrano Godoy, M.; Mas Atance, J.; García Gutiérrez, R. Fractura de cadera en el paciente anciano: Factores pronóstico de mortalidad y recuperación funcional al año [Hip fracture in the elderly patient: Prognostic factors for mortality and functional recovery at one year]. Rev. Esp. Geriatr. Gerontol. 2018, 53, 247–254. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Belmont, P.J., Jr.; Garcia, E.J.; Romano, D.; Bader, J.O.; Nelson, K.J.; Schoenfeld, A.J. Risk factors for complications and in-hospital mortality following hip fractures: A study using the National Trauma Data Bank. Arch. Orthop. Trauma. Surg. 2014, 134, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Ariza-Vega, P.; Kristensen, M.T.; Martín-Martín, L.; Jiménez-Moleón, J.J. Predictors of long-term mortality in older people with hip fracture. Arch. Phys. Med. Rehabil. 2015, 96, 1215–1221. [Google Scholar] [CrossRef] [PubMed]
- Aranguren-Ruiz, M.I.; Acha-Arrieta, M.V.; Casas-Fernández de Tejerina, J.M.; Arteaga-Mazuelas, M.; Jarne-Betrán, V.; Arnáez-Solis, R. Risk factors for mortality after surgery of osteoporotic hip fracture in patients over 65 years of age. Rev. Esp. Cir. Ortop. Traumatol. 2017, 61, 185–192. (In English) [Google Scholar] [CrossRef] [PubMed]
- Hou, M.; Zhang, Y.; Chen, A.C.; Liu, T.; Yang, H.; Zhu, X.; He, F. The effects of dementia on the prognosis and mortality of hip fracture surgery: A systematic review and meta-analysis. Aging Clin. Exp. Res. 2021, 33, 3161–3172. [Google Scholar] [CrossRef]
- Yombi, J.C.; Putineanu, D.C.; Cornu, O.; Lavand’homme, P.; Cornette, P.; Castanares-Zapatero, D. Low haemoglobin at admission is associated with mortality after hip fractures in elderly patients. Bone Jt. J. 2019, 101, 1122–1128. [Google Scholar] [CrossRef]
- Guzon-Illescas, O.; Perez Fernandez, E.; Crespí Villarias, N.; Quirós Donate, F.J.; Peña, M.; Alonso-Blas, C.; García-Vadillo, A.; Mazzucchelli, R. Mortality after osteoporotic hip fracture: Incidence, trends, and associated factors. J. Orthop. Surg. Res. 2019, 14, 203. [Google Scholar] [CrossRef]
- Babagoli, M.; Raeini, A.G.; Sheykhvatan, M.; Baghdadi, S.; Shafiei, S.H. Influencing factors on morbidity and mortality in intertrochanteric fractures. Sci. Rep. 2023, 13, 12090. [Google Scholar] [CrossRef]
- Chang, W.; Lv, H.; Feng, C.; Yuwen, P.; Wei, N.; Chen, W.; Zhang, Y. Preventable risk factors of mortality after hip fracture surgery: Systematic review and meta-analysis. Int. J. Surg. 2018, 52, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Tarazona-Santabalbina, F.J.; Belenguer-Varea, A.; Rovira-Daudi, E.; Salcedo-Mahiques, E.; Cuesta-Peredó, D.; Doménech-Pascual, J.R.; Salvador-Pérez, M.I.; Avellana-Zaragoza, J.A. Early interdisciplinary hospital intervention for elderly patients with hip fractures: Functional outcome and mortality. Clinics 2012, 67, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Linn, B.S.; Linn, M.W.; Gurel, L. Cumulative illness rating scale. J. Am. Geriatr. Soc. 1968, 16, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Ignacio de Ulíbarri, J.; González-Madroño, A.; de Villar, N.G.; González, P.; González, B.; Mancha, A.; Rodríguez, F.; Fernández, G. CONUT: A tool for controlling nutritional status. First validation in a hospital population. Nutr. Hosp. 2005, 20, 38–45. [Google Scholar] [PubMed]
- Müller-Mai, C.M.; Schulze Raestrup, U.S.; Kostuj, T.; Dahlhoff, G.; Günster, C.; Smektala, R. One-year outcomes for proximal femoral fractures: Posthospital analysis of mortality and care levels based on health insurance data. Der Unfallchirurg 2015, 118, 780–794. [Google Scholar] [CrossRef] [PubMed]
- Haddad, B.I.; Hamdan, M.; Alshrouf, M.A.; Alzubi, A.; Khirsheh, A.; Al-Oleimat, A.; Aldabaibeh, M.; Al-Qaryouti, R.; Abulubbad, W.; Al-Saber, M.; et al. Preoperative hemoglobin levels and mortality outcomes after hip fracture patients. BMC Surg. 2023, 23, 266. [Google Scholar] [CrossRef] [PubMed]
- González-Marcos, E.; González-García, E.; Rodríguez-Fernández, P.; Sánchez-González, E.; González-Bernal, J.J.; González-Santos, J. Determinants of Higher Mortality at Six Months in Patients with Hip Fracture: A Retrospective Study. J. Clin. Med. 2022, 11, 2514. [Google Scholar] [CrossRef] [PubMed]
- Heyes, G.J.; Tucker, A.; Marley, D.; Foster, A. Predictors for 1-year mortality following hip fracture: A retrospective review of 465 consecutive patients. Eur. J. Trauma Emerg. Surg. 2017, 43, 113–119. [Google Scholar] [CrossRef]
- Shi, H.; Gao, Y.; Zhao, W.; Wang, H.; Wu, X.; Wang, F.; Yang, X.; Li, J. Development of a prediction model for postoperative complications and economic burden analysis in older patients with hip fractures. Heliyon 2023, 9, e20342. [Google Scholar] [CrossRef]
- Chung, H.J.; Kim, D.S.; Lee, J.W.; Hong, S.I. Analyzing the Risk Factors of Mortality after Osteoporotic Hip Fractures Using the National Health Insurance Service Sample Cohort 2.0 Database. Hip Pelvis. 2022, 34, 150–160. [Google Scholar] [CrossRef] [PubMed]
- Ercin, E.; Bilgili, M.G.; Sari, C.; Basaran, S.H.; Tanriverdi, B.; Edipoglu, E.; Celen, K.M.; Cetingok, H.; Kural, C. Risk factors for mortality in geriatric hip fractures: A compressional study of different surgical procedures in 785 consecutive patients. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Fu, S.; Yao, Y.; Yuan, W.; Zhao, Y. Age, Prognostic Nutritional Index, and Charlson Comorbidity Index Were Independent Risk Factors for PostoperativePostoperative Long-Term Mortality in Chinese Geriatric Patients Who Sustain Hip Fracture. J. Am. Med. Dir. Assoc. 2021, 22, 2602–2603. [Google Scholar] [CrossRef] [PubMed]
- Duaso, E.; Gamboa-Arango, A.; Formiga, F.; Marimón, P.; Salgado, M.T.; Murga, V.; Lumbreras, C.; Tarrida, A. Factores pronósticos de mortalidad al año de una fractura de cadera por fragilidad ósea. Estudio Maluc Anoia [Prognostic factors of mortality one year after a hip fragility fracture. Anoia hip study]. Rev. Esp. Geriatr. Gerontol. 2021, 56, 18–23. (In Spanish) [Google Scholar] [CrossRef]
- Xing, F.; Luo, R.; Chen, W.; Zhou, X. The risk-adjusted Charlson comorbidity index as a new predictor of one-year mortality rate in elderly Chinese patients who underwent hip fracture surgery. Orthop. Traumatol. Surg. Res. 2021, 107, 102860. [Google Scholar] [CrossRef]
- Drevet, S.; Bornu, B.C.; Boudissa, M.; Bioteau, C.; Mazière, S.; Merloz, P.; Couturier, P.; Tonetti, J.; Gavazzi, G. One-year mortality after a hip fracture: Prospective study of a cohort of patients aged over 75 years old. Geriatr. Psychol. Neuropsychiatr. Vieil. 2019, 17, 369–376. [Google Scholar] [CrossRef]
- Novoa-Parra, C.D.; Hurtado-Cerezo, J.; Morales-Rodríguez, J.; Sanjuan-Cerveró, R.; Rodrigo-Pérez, J.L.; Lizaur-Utrilla, A. Factores predictivos de la mortalidad al año en pacientes mayores de 80 años intervenidos de fractura del cuello femoral. Rev. Española De Cirugía Ortopédica Y Traumatol. 2019, 63, 202–208. [Google Scholar] [CrossRef]
- Cabrerizo, S.; Cuadras, D.; Gomez-Busto, F.; Artaza-Artabe, I.; Marín-Ciancas, F.; Malafarina, V. Serum albumin and health in older people: Review and meta analysis. Maturitas 2015, 81, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.U.; Rho, J.H.; Choi, Y.J.; Jun, S.W.; Shin, Y.J.; Lee, Y.S.; Shin, H.J.; Lim, H.; Shin, H.W.; Kim, J.H.; et al. Postoperative hypoalbuminemia is an independent predictor of 1-year mortality after surgery for geriatric intertrochanteric femoral fracture: A retrospective cohort study. Medicine 2021, 100, e28306. [Google Scholar] [CrossRef]
- Li, S.; Zhang, J.; Zheng, H.; Wang, X.; Liu, Z.; Sun, T. Prognostic Role of Serum Albumin, Total Lymphocyte Count, and Mini Nutritional Assessment on Outcomes After Geriatric Hip Fracture Surgery: A Meta-Analysis and Systematic Review. J. Arthroplasty. 2019, 34, 1287–1296. [Google Scholar] [CrossRef]
- Manosroi, W.; Atthakomol, P.; Isaradech, N.; Phinyo, P.; Vaseenon, T. Preoperative Correction of Low Hemoglobin Levels Can Reduce 1-Year All-Cause Mortality in Osteoporotic Hip Fracture Patients: A Retrospective Observational Study. Clin. Interv. Aging. 2022, 17, 165–173. [Google Scholar] [CrossRef] [PubMed]
| Variable | Survivors n = 2380 | Deceased n = 846 | p-Value |
|---|---|---|---|
| Age (years), m (SD) | 83.5 (6.1) | 86.7 (6.2) | <0.001 |
| Male sex, n (%) | 529 (22.2%) | 318 (37.6%) | <0.001 |
| Biochemical | |||
| Hemoglobin upon admission (g/dL), m (SD) | 12.5 (1.6) | 11.9 (1.9) | <0.001 |
| Albumin upon admission (g/dL), m (SD) | 3.9 (0.4) | 3.8 (0.5) | <0.001 |
| Clinical | |||
| Charlson Comorbidity Index, m (SD) | 2.2 (2.1) | 3.5 (2.7) | <0.001 |
| Initial CONUT, m (SD) | 2.9 (1.9) | 3.7 (2.1) | <0.001 |
| CIRS-G, m (SD) | 10.2 (3.9) | 12.0 (4.1) | <0.001 |
| ICC with age, m (SD) | 5.8 (2.3) | 7.3 (2.8) | <0.001 |
| Glomerular filtration rate upon admission (mL/min), m (SD) | 66.0 (24.3) | 59.9 (26.5) | <0.001 |
| Initial CONUT with moderate or severe nutritional risk, n (%) | 299 (14.5%) | 218 (29.4%) | <0.001 |
| Previous ischemic heart disease, n (%) | 173 (7.3%) | 81 (9.6%) | 0.037 |
| Previous heart failure, n (%) | 127 (5.3%) | 73 (8.6%) | <0.001 |
| Previous COPD, n (%) | 323 (13.6%) | 168 (19.9%) | <0.001 |
| Previous chronic renal failure, n (%) | 217 (9.1%) | 133 (15.7%) | <0.001 |
| Previous diabetes, n (%) | 651 (27.4%) | 264 (31.2%) | 0.037 |
| Variable | Survivors n = 2380 | Deceased n = 846 | p-Value |
|---|---|---|---|
| Clinical | |||
| Length of stay, m (SD) | 7.8 (3.0) | 8.9 (5.9) | <0.001 |
| Number of complications, m (SD) | 1.6 (1.8) | 0.9 (1.2) | <0.001 |
| Number of major complications, m (SD) | 1.4 (1.6) | 0.8 (1.1) | <0.001 |
| Days until re-entry, m (SD) | 80.1 (83.8) | 55.4 (63.6) | <0.001 |
| Surgical delay, m (SD) | 44.0 (28.3) | 48.9 (38.3) | <0.001 |
| Number of concentrates transfused, m (SD) | 1.4 (1.7) | 2.0 (2.2) | <0.001 |
| Complication during admission, n (%) | 1085 (45.6%) | 532 (62.9%) | <0.001 |
| Major complication during admission, n (%) | 1047 (44%) | 512 (60.5%) | <0.001 |
| Hospital readmissions, n (%) | 357 (15%) | 298 (35.2%) | <0.001 |
| Reintervention, n (%) | 29 (1.2%) | 23 (2.7%) | 0.006 |
| Intervention first 36 h, n (%) | 1528 (64.2%) | 511 (60.4%) | 0.051 |
| Intervention first 72 h, n (%) | 2026 (85.1%) | 687 (81.2%) | 0.009 |
| ASA score >2, n (%) | 69 (3.4%) | 69 (9.4%) | <0.001 |
| Patients transfused, n (%) | 1335 (56.1%) | 573 (67.7%) | <0.001 |
| Final CONUT with moderate or severe nutritional risk, n (%) | 362 (17.6%) | 273 (36.8%) | <0.001 |
| Delirium (%) | 225 (9.5%) | 128 (15.1%) | <0.001 |
| Cardiac complication during admission, n (%) | 95 (4%) | 110 (13%) | <0.001 |
| Final CONUT, m (SD) | 2.7 (2.1) | 4.0 (2.5) | <0.001 |
| Respiratory complications | 61 (2.6%) | 97 (11.5%) | <0.001 |
| Biochemical | |||
| Hemoglobin at discharge (g/dL), m (SD) | 10.3 (1.2) | 10.4 (1.6) | 0.796 |
| Albumin at discharge (g/dL), m (SD) | 3.8 (0.5) | 3.6 (0.5) | <0.001 |
| Glomerular filtration rate at discharge (mL/min), m (SD) | 82.3 (36.4) | 72.8 (39.1) | <0.001 |
| Variable | Hazard Ratio | 95%CI | p-Value |
|---|---|---|---|
| Sex | 1.72 | 1.46–2.03 | <0.001 |
| ASA score ≥3 | 1.47 | 1.12–1.94 | 0.008 |
| Dementia | 1.38 | 1.14–1.67 | <0.001 |
| Charlson Comorbidity Index | 1.12 | 1.10–1.15 | <0.001 |
| Age | 1.07 | 1.06–1.09 | <0.001 |
| Hemoglobin upon admission (g/dL) | 0.90 | 0.85–0.93 | <0.001 |
| Albumin upon admission (g/dL) | 0.65 | 0.55–0.76 | <0.001 |
| Variable | Hazard Ratio | 95%CI | p-Value |
|---|---|---|---|
| Respiratory complication | 2.20 | 1.66–2.80 | <0.001 |
| Hospital readmission | 2.17 | 1.86–2.52 | <0.001 |
| Cardiac complication | 1.64 | 1.28–2.10 | <0.001 |
| Delirium during admission | 1.38 | 1.12–1.69 | 0.002 |
| Complications during admission | 1.31 | 1.12–1.54 | 0.001 |
| Glomerular filtration rate at discharge (mL/min) | 995 | 0.993–0.998 | <0.001 |
| Albumin at discharge (mg/dL) | 0.59 | 0.51–0.67 | <0.001 |
| Variable | Hazard Ratio | 95%CI | p-Value |
|---|---|---|---|
| Respiratory complications | 2.42 | 1.42–4.14 | 0.001 |
| Hospital readmission | 1.96 | 1.66–2.32 | <0.001 |
| Cardiac complication | 1.88 | 1.46–2.42 | <0.001 |
| Male sex | 1.65 | 1.40–1.96 | <0.001 |
| Dementia | 1.37 | 1.13–1.66 | <0.001 |
| ASA score ≥3 | 1.34 | 1.02–1.77 | 0.036 |
| Charlson Comorbidity Index | 1.08 | 1.05–1.12 | <0.001 |
| Age | 1.08 | 1.06–1.09 | <0.001 |
| Hemoglobin upon admission (g/dL) | 0.89 | 0.85–0.93 | <0.001 |
| Albumin at discharge (mg/dL) | 0.64 | 0.56–0.74 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Tercero, E.; Belenguer-Varea, Á.; Villalon-Ruibio, D.; López Gómez, J.; Trigo-Suarez, R.; Cunha-Pérez, C.; Borda, M.G.; Tarazona-Santabalbina, F.J. Respiratory Complications Are the Main Predictors of 1-Year Mortality in Patients with Hip Fractures: The Results from the Alzira Retrospective Cohort Study. Geriatrics 2024, 9, 47. https://doi.org/10.3390/geriatrics9020047
García-Tercero E, Belenguer-Varea Á, Villalon-Ruibio D, López Gómez J, Trigo-Suarez R, Cunha-Pérez C, Borda MG, Tarazona-Santabalbina FJ. Respiratory Complications Are the Main Predictors of 1-Year Mortality in Patients with Hip Fractures: The Results from the Alzira Retrospective Cohort Study. Geriatrics. 2024; 9(2):47. https://doi.org/10.3390/geriatrics9020047
Chicago/Turabian StyleGarcía-Tercero, Elisa, Ángel Belenguer-Varea, Daniela Villalon-Ruibio, Jesús López Gómez, Rodrigo Trigo-Suarez, Cristina Cunha-Pérez, Miguel Germán Borda, and Francisco Jose Tarazona-Santabalbina. 2024. "Respiratory Complications Are the Main Predictors of 1-Year Mortality in Patients with Hip Fractures: The Results from the Alzira Retrospective Cohort Study" Geriatrics 9, no. 2: 47. https://doi.org/10.3390/geriatrics9020047
APA StyleGarcía-Tercero, E., Belenguer-Varea, Á., Villalon-Ruibio, D., López Gómez, J., Trigo-Suarez, R., Cunha-Pérez, C., Borda, M. G., & Tarazona-Santabalbina, F. J. (2024). Respiratory Complications Are the Main Predictors of 1-Year Mortality in Patients with Hip Fractures: The Results from the Alzira Retrospective Cohort Study. Geriatrics, 9(2), 47. https://doi.org/10.3390/geriatrics9020047