Abstract
The passing of the years of life physiologically leads to the accumulation of changes in tissues in the oral cavity, influencing dentition, chewing and swallowing mechanisms, and the oral microbiota. Some diseases and medications can aggravate oral symptoms and negatively influence eating behaviours, increasing the likelihood of becoming malnourished. This could make older individuals more vulnerable to complications when undergoing major orthopaedic surgery. Hidden infection foci in the oral cavity are a recognised cause of post-operative periprosthetic joint infections. Dysfunctional oral problems might also compromise feeding after surgery when good nutrition represents a fundamental aspect of a proper recovery. To manage these shortcomings, in this article, the authors hypothesise a multidisciplinary path of care named the Integrated Oral Health Network applied to major Orthopaedic Surgery (IOHN-OS). This peri-operative initiative would include pre-operative oral health screening and risk management by a dental team, patient education programmes before and after surgery, and bedside gerodontology actions like oral care and meal and eating support for fragile individuals. The IOHN-OS has the potential to reshape the concept of suitability for major orthopaedic surgery and generate momentum for designing community-based surveillance programmes that can keep the mouths of older subjects healthy for a long time.
1. Introduction
Surgery is the reference approach when there is chronic hip, knee, or back pain that reduces a patient’s functional independence and quality of life. The age-related deterioration of joints and bones is the fundamental cause, and, therefore, the majority of patients are older adults. The insertion of joint endoprostheses or spine stabilisers leads to good results in most patients. However, a number of cases do not properly recover, indirectly producing far-reaching human and economic consequences [1]. The common denominators in these cases are smoking, polymorbidity, and malnutrition [2]. Improving outcomes requires innovations, both in surgery and in the peri-operative path of care [3]. This approach is more likely to correct modifiable physical, mental, and social conditions of vulnerability [4]. This notion is not new, and guidance stating that a holistic approach can counteract the reduction in the intrinsic capacity of older individuals has already been issued by the World Health Organization [5]. In orthopaedic surgery, examples of multidisciplinary and multimodal approaches are the Enhanced Recovery After Surgery (ERAS) [6], which has previously been applied in hospitals for some time, bringing notable improvements to clinical practice, and the Healthy Eating, Physical Activity, and Sleep hygiene (HEPAS) [7], which has remained a conceptual proposal for a novel territorial organisational model. Both initiatives demand alliances between orthopaedic surgeons, anaesthetists, case-manager nurses, physiotherapists, orthopaedic technicians, dietitians, and psychologists. A continuum of this collaborative care during home transitions and in the community might have the desired effect of guaranteeing the maintenance of a patient’s well-being in the long term [8]. To further enhance the quality of care of multidisciplinary approaches in orthopaedic surgery, we theorise a new in-hospital path that would integrate a dental team into the professional community that takes care of the older orthopaedic patient.
2. Ageing Poses a Risk to the Oral Cavity of Older Individuals
Tooth loss is not inevitable. However, ageing has a negative impact on teeth structure, salivation, chewing and swallowing mechanisms (i.e., presbyphagia) [9], oral microbiome [10], and oropharyngeal sensitivity. A decrease in gustatory and olfactory functioning influences the hedonic appreciation of food and can push a person towards increasingly rewarding food choices [11]. Food predispositions mainly drive the subject’s choices towards the more cariogenic or less healthy food nevertheless (e.g., sweeter and saltier) [12]. Xerostomia is known to impair cephalic digestion [13]. It is not uncommon for patients with poor oral moisture to modify their eating behaviours to avoid dry foods [14]. Low salivation increases the risk of oral diseases due to the lack of an optimal concentration of species-specific antimicrobial peptides, thus allowing tooth decay-causing bacteria to grow freely [13]. A recession of gingival tissues exposes the root surface to this contaminated environment. A lack of enamel and progressive demineralization make the area more susceptible to cavities and caries. Bone resorption and negative calcium balance in osteoporotic patients also affect trabecular bone parameters like number, thickness, and connectivity [15], further increasing alveolar porosity [16]. Alveolar bone, maintained by healthy oral conditions and reinforced by biting occlusal forces [17], deteriorates and no longer supports the teeth. Edentulism and ill-fitting dentures are associated with worse bite force and chewing efficiency [18]. Patients’ food choices will be further diverted to foods with a soft texture [19].
3. Impact of Medications and Illnesses on the Oral Health of Older Patients
Oral problems can arise due to concomitant illnesses prevalent in the older population or can worsen after the chronic use of drugs that treat the same diseases. Increased susceptibility to oral infections is a consequence of xerostomia-derived diabetes mellitus [20], with hyposalivation also being initiated by some antihypertensive medications and tricyclic antidepressants [21]. Glossitis, caries, and maxillary and mandibular osteoporosis are all common manifestations of thyroid dysfunction [22]. Swallowing disorders occur in advanced Parkinson’s disease and other neurodegenerative conditions involving hypotonia of the oral muscles [23]. Similar disorders are experienced in the case of severe gastropathy and gastroesophageal reflux. On the other hand, the use of aluminium-containing antiacids to relieve gastric hyperacidity can significantly increase the urinary and faecal excretion of calcium if not balanced by an adequate dietary intake, as well as phosphorus [24]. Similar consequences on calcium homeostasis and that of other minerals essential for dental health (e.g., zinc, magnesium, potassium) are elicited by loop diuretics [25], which are frequently used in disorders of sodium balance. The bone side effects of drugs include sparse facial bone structures and can also lead to consequences that are rare, serious, and definitive, such as the osteonecrosis of the jaw derived from prolonged therapy with antiresorptive bisphosphonates [26].
4. The Vicious Cycle between Oral Health and Nutrition in Older Adults
Oral health problems can be detrimental to an individual’s nutritional status [14,19]. Food choices are guided by the degree of masticatory and swallowing ability [19]. Hence, older adults with dentures may not be able to easily eat raw vegetables and nuts [27]. Softer and easier-to-chew foods are usually preferred, but they tend to have less nutritional value [28]. The prolonged consumption of texture-modified food groups can be harmful, analogous to extended cooking to soften the texture. In fact, this practice has been plainly recognised to deplete the content of heat-labile vitamins [29]. The mouth also mirrors the subject’s degree of commitment to oral hygiene. Individuals with cognitive dysfunction have generally poorer oral health [30], which in turn can indicate how physically inactive [31] or physically dependent [32] the subject is. Individuals who are already malnourished may show typical oral signs. Among the first consequences are effects on the mucosa due to its rapid turnover. Glossitis and angular cheilitis can occur in the case of inadequate levels of B-complex vitamins or iron, whose deficiency anaemia is associated with gingivitis, oral ulcers, glossitis, and dental decay [33]. L-ascorbic acid deficiency causes periodontal and gum diseases and bleeding on probing [34]. In the case of heartburn, patients often limit their intake of citrus fruits, further increasing the risk of scurvy. Folate and B12 deficiencies, present in approximately 1 in 15 older adults [35], are associated with a fiery red sore tongue and ulcer formation. In addition to deficiencies of water-soluble vitamins, older adults who use bile acid sequestrants like cholestyramine are also exposed to reduced absorption of lipophilic vitamins, all of which play an important role in oral health maintenance [36].
5. Unhealthy Oral Health Conditions Might Pose a Risk to Recovery after Surgery
It is not known what causes an impact first, whether it is the ageing process, malnutrition, or the oral consequences of medications and diseases. It is likely that these factors are intertwined in a complex, vicious cycle. It is estimated that there are around 100 million people over the age of 65 living on this planet with a disabling musculoskeletal condition who would benefit from surgery [8]. Among older adults scheduled for joint replacement surgery, only 1 in 10 eat healthily [37], 3 in 10 show systemic signs of micronutrient deficiencies [38], and 4 in 10 are malnourished before surgery [39]. Given the malnutritional phenotype of the older patient undergoing major orthopaedic surgery, it is not surprising that oral problems in this cluster have a higher prevalence than their healthy counterparts. Periodontal diseases and the decay of permanent teeth affect one in five older people globally, with a similar prevalence of edentulism, which grows exponentially after the age of 65 [40]. Conversely, oral problems that hide an active focus of infection afflict as many as one in three older patients waiting for a hip or knee replacement [41]. This is particularly relevant to pre-operative risk stratification. A healthy oral cavity harbours an ecological balance that depends on the conditions of the human host and living microorganisms. A disruption of this balance due to the worsening of the hosts’ strength of constitution or changes in the oral environment can lead to bacterial overgrowth, aspiration pneumonia, and translocation to other tissues [42]. It has been a common belief for more than thirty years now that infection foci in the oral cavity at the time of major orthopaedic surgery may increase the risk of periprosthetic joint infection (PJI) [43]. Intermittent/persistent bacteraemia from dental infections is known to be a source of haematogenous seeding, although the odontogenic aetiology of the infection would remain complex to demonstrate [44]. Experiences with pre-operative dental screening in orthopaedic surgery highlighted a significant number of older individuals requiring dental intervention [45]. It is not known how much time must elapse between dental and orthopaedic procedures to avoid the risk of the transient bacteraemia-derived PJI. It must be noted, however, that even in the case of an indication for a dental visit before orthopaedic surgery, an older individual could have various impediments to access: an inability to arrange the visit (e.g., distance, homebound), a lack of money or willingness to pay, or odontophobia [46]. There is also a recognised lack of professionals trained in the care of geriatric patients [47]. The notable gap regarding preventive or corrective treatments before surgery has led the current practice to predominantly focus on a few post-operative actions, such as the use of antibiotic prophylaxis during the initial healing period [48]. However, there is room for more comprehensive initiatives. Even in the absence of physical and mental impediments, a patient may eat only half of the calories served in the first days after spine surgery [49], with the other half possibly posing a risk of silent aspiration from unnoticed dental occlusion disorders, xerostomia, periodontal disease, or ill-fitting dentures [50]. Since osteoarthritis can also affect the hands, elbows, and shoulders, it is reasonable to think that even if the patient is able to move to the bathroom and brush their teeth, some may have difficulty handling a toothbrush. Temporomandibular joint deterioration, although subclinical, may also be quite common among older adults, further disrupting related musculature [51]. These and other reasons, which encompass the infectious and nutritional risks linked to an unhealthy mouth, diseases, and/or medications that worsen the symptoms and possible illiteracy about or an inability to apply effective oral hygiene techniques, together with frequent downtimes during hospitalisation, push us to construct a path of quality improvement.
6. The Integrated Oral Health Network Applied to Orthopaedic Surgery (IOHN-OS)
We think that an indication for elective orthopaedic surgery is the ideal time to check on oral health and to start what can be defined as the Integrated Oral Health Network applied to Orthopaedic Surgery (IOHN-OS). The scope of a generalist dental consultation is to preserve or restore the desired degree of functionality of the oral cavity. The IOHN-OS would aim to (1) mitigate the patient’s pre-operative vulnerabilities, (2) integrate bedside gerodontology for in-hospital oral hygiene, meal, and eating support, (3) provide educational materials on geriatric dentistry, and (4), if needed, schedule follow-up dental visits. In Figure 1, we report an infographic that illustrates the various phases of the process.
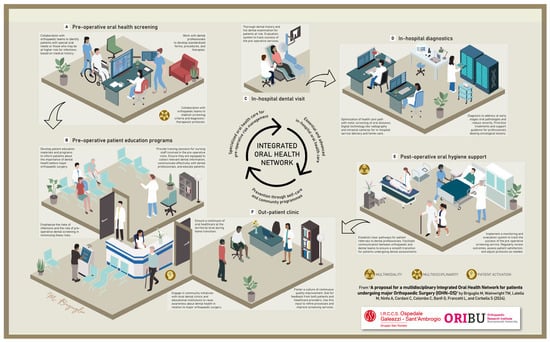
Figure 1.
Healthcare network and stages to improve the quality of orthopaedic care with the integration of a dental team. A framework that presents the Integrated Oral Health Network applied to Orthopaedic Surgery (IOHN-OS), designed to enhance the perioperative care trajectory of patients’ vulnerabilities, especially if they are old and malnourished. The successful application of the IOHN-OS would effectively implement an oral risk screening (A), diagnosis when needed (C,D), and corrective initiative before surgery (B), further delivering in-hospital services (E) and long-term oral health programmes (F) for the orthopaedic population.
In brief, trained case-manager nurses (or a dental professional if available) could lead the initial oral screening at pre-admission visits using standardised forms specifically developed to discover if there is any oral problem. If so, multidisciplinary management based on the patient’s prevailing clinical and surgical needs will be activated, including a specialist examination when required. Patients with special oral needs could benefit from in-hospital advanced diagnostic tools, such as radiographic equipment and laboratories, which can potentially shorten the time for an accurate and definitive diagnosis. The practice of oral hygiene at the bedside by dental hygienists would enhance the quality of health care and patient experiences and enrich the collaborative peri-operative team of dietitians (e.g., medical nutrition therapy), physiotherapists (e.g., masticatory muscle exercises [52]), and speech pathologists (e.g., chewing and swallowing rehabilitation). Inter-profession and patient interactions would be coordinated by a case-manager nurse and tailored to the post-operative patient’s level of autonomy, mobility, collaboration, and rehabilitative needs. Importantly, the oral consequences of degenerative conditions or medications must be projected over time, anticipating the involvement of other specialists or remodelling pharmacotherapy that poses a threat to oral health. A risk control initiative for potential infectious foci or aspiration pneumonia must be prioritized from a stratified risk management perspective. The continuity of care will be guaranteed even after discharge, with territorial care pathways integrated with the same multidisciplinary and multimodal competence. This would require rebuilding the existing pathways and creating economic, legal, and political conditions that adhere to a geriatric oral health care transition model as a basis for a population-relevant approach [53].
Limitations
The theoretical IOHN-OS must be interpreted with caution. First, communication between the dental team, the orthopaedic surgeon, and the patient is essential, and without it, this approach is unsuitable. Patients should be activated by the orthopaedic surgeon or any other deputy in charge, such as the case-manager nurse, who takes the initiative. Simply increasing pre-operative awareness about proper oral hygiene is not sufficient to push patients to undergo a dental consultation before orthopaedic surgery [54]. Second, the treatment of some oral problems, such as periodontal diseases and ill-fitting dentures, takes time. The IOHN-OS team, together with the patient, will have to balance the risks/benefits of a temporary pre-operative risk mitigation treatment without postponing orthopaedic surgery against a time-consuming restoration of the desired degree of function of the mouth. Third, the success of the IOHN-OS may strongly depend on where the pre-operative dental consultation is organised. Reduced feasibility could occur when dental visits do not take place where a patient is scheduled to be operated on. A similar inapplicability may also arise when there are no dentists or dental hygienists on-site for bedside gerodontology activities. Fourth, educational initiatives before and after surgery may not be viable for older patients who are routinely depending on a caregiver since it ought to be that the latter are involved in the training programme. Digital technologies for oral health literacy, training, detection, and surveillance like mOralHealth [55] might help. Fifth, specialist oral care, diagnostic, and bedside visits with portable equipment pose an economic obstacle that cannot always be overcome [45]. A similar costly burden may arise when a transversal dental referral with oriented therapy before surgery is imposed by the hospital [41]. The IOHN-OS will need to be more sustainable [43], perhaps providing different degrees of support through the allocation of more comprehensive and in-depth resources to more at-risk and/or vulnerable patients (i.e., health equity). This could also help overcome eventual dental system decay and dentist shortages. In time, investments ought to be made to cover in-hospital dental visits, accompanying diagnostic–therapeutic expenses, and external consultations when an orthopaedic clinic lacks a dental department. Forecasting/longitudinal studies will have to justify the cost.
7. Conclusions
As healthcare providers in orthopaedic surgery, we diligently endeavour to correct modifiable pre-operative patients’ vulnerabilities and enhance peri-operative experiences to mitigate the risk of complications and support patients in living a burden-free, happy, and long life after surgery. The theorised IOHN-OS incorporates oral health assessment and management before surgery, in-hospital oral hygiene and support, and both usual and innovative education programmes before and after surgery (e.g., techniques to minimise recessions, fluoride regimens, tailored antibiotic treatment that preserves “good” bacteria [1]). This integrated network has the potential to prolong an older person’s desire to smile and their ability to eat and speak over time. It can also motivate stakeholders to align with the functional, psychosocial, and economic perspectives of patients. Population-based actions like the IOHN-OS may be equally important in dealing with increasing life expectancy, phenotypic complexities, and healthcare demands and costs. It could be the missing piece of a truly holistic, patient-centred approach required in today’s medicine.
Author Contributions
Conceptualization, M.B., T.W.W. and S.C.; writing—original draft preparation, M.B.; writing—review and editing, T.W.W., M.L., A.N., C.C. (Claudio Cordani), C.C. (Cecilia Colombo), G.B., L.F. and S.C.; visualization, M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This article is part of the project “Ricerca Corrente” of the Italian Ministry of Health, which funded the APC.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Abdeen, A.; Della Valle, C.J.; Kendoff, D.; Chen, A.F. The Paradox of Prosthetic Joint Infection and the Microbiome: Are Some Bacteria Actually Helpful? Arthroplast. Today 2022, 13, 116–119. [Google Scholar] [CrossRef]
- Patel, R. Periprosthetic Joint Infection. N. Engl. J. Med. 2023, 388, 251–262. [Google Scholar] [CrossRef]
- Kappenschneider, T.; Maderbacher, G.; Weber, M.; Greimel, F.; Holzapfel, D.; Parik, L.; Schwarz, T.; Leiss, F.; Knebl, M.; Reinhard, J.; et al. Special orthopaedic geriatrics (SOG)—A new multiprofessional care model for elderly patients in elective orthopaedic surgery: A study protocol for a prospective randomized controlled trial of a multimodal intervention in frail patients with hip and knee replacement. BMC Musculoskelet. Disord. 2022, 23, 1079. [Google Scholar] [CrossRef]
- Briguglio, M.; Wainwright, T.W. Nutritional and Physical Prehabilitation in Elective Orthopedic Surgery: Rationale and Proposal for Implementation. Ther. Clin. Risk Manag. 2022, 18, 21–30. [Google Scholar] [CrossRef] [PubMed]
- Tavassoli, N.; de Souto Barreto, P.; Berbon, C.; Mathieu, C.; de Kerimel, J.; Lafont, C.; Takeda, C.; Carrie, I.; Piau, A.; Jouffrey, T.; et al. Implementation of the WHO integrated care for older people (ICOPE) programme in clinical practice: A prospective study. Lancet Healthy Longev. 2022, 3, e394–e404. [Google Scholar] [CrossRef] [PubMed]
- Wainwright, T.W. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2020, 91, 363. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, M. The Burdens of Orthopedic Patients and the Value of the HEPAS Approach (Healthy Eating, Physical Activity, and Sleep Hygiene). Front. Med. 2021, 8, 650947. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, M.; Cordani, C.; Langella, F.; Perazzo, P.; Pregliasco, F.E.; Banfi, G.; Wainwright, T.W. Why Treat Patients with a Major Orthopaedic Surgery Only to Send Them Back to the Vulnerable Conditions That Made Them Sick in the First Place? A Conceptual Scenario to Improve Patient’s Journey. Int. J. Gen. Med. 2023, 16, 4729–4735. [Google Scholar] [CrossRef] [PubMed]
- Ambiado-Lillo, M.M. Presbyphagia: A Conceptual Analysis of Contemporary Proposals and Their Influences on Clinical Diagnosis. Dysphagia 2024, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kazarina, A.; Kuzmicka, J.; Bortkevica, S.; Zayakin, P.; Kimsis, J.; Igumnova, V.; Sadovska, D.; Freimane, L.; Kivrane, A.; Namina, A.; et al. Oral microbiome variations related to ageing: Possible implications beyond oral health. Arch. Microbiol. 2023, 205, 116. [Google Scholar] [CrossRef]
- Jacobson, A.; Green, E.; Murphy, C. Age-related functional changes in gustatory and reward processing regions: An fMRI study. Neuroimage 2010, 53, 602–610. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Birch, L.L. Development of food preferences. Annu. Rev. Nutr. 1999, 19, 41–62. [Google Scholar] [CrossRef] [PubMed]
- Dawes, C.; Pedersen, A.M.; Villa, A.; Ekström, J.; Proctor, G.B.; Vissink, A.; Aframian, D.; McGowan, R.; Aliko, A.; Narayana, N.; et al. The functions of human saliva: A review sponsored by the World Workshop on Oral Medicine VI. Arch. Oral. Biol. 2015, 60, 863–874. [Google Scholar] [CrossRef] [PubMed]
- Müller, F.; Chebib, N.; Maniewicz, S.; Genton, L. The Impact of Xerostomia on Food Choices—A Review with Clinical Recommendations. J. Clin. Med. 2023, 12, 4592. [Google Scholar] [CrossRef] [PubMed]
- Ulm, C.; Kneissel, M.; Schedle, A.; Solar, P.; Matejka, M.; Schneider, B.; Donath, K. Characteristic features of trabecular bone in edentulous maxillae. Clin. Oral Implant. Res. 1999, 10, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Zihni Korkmaz, M.; Yemenoğlu, H.; Günaçar, D.N.; Ustaoğlu, G.; Ateş Yildirim, E. The effects of vitamin D deficiency on mandibular bone structure: A retrospective radiological study. Oral Radiol. 2023, 39, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Walczak, A.; Krenz-Niedbała, M.; Łukasik, S. Insight into age-related changes of the human facial skeleton based on medieval European osteological collection. Sci. Rep. 2023, 13, 20564. [Google Scholar] [CrossRef] [PubMed]
- Boven, G.C.; Raghoebar, G.M.; Vissink, A.; Meijer, H.J. Improving masticatory performance, bite force, nutritional state and patient’s satisfaction with implant overdentures: A systematic review of the literature. J. Oral Rehabil. 2015, 42, 220–233. [Google Scholar] [CrossRef]
- N’gom, P.I.; Woda, A. Influence of impaired mastication on nutrition. J. Prosthet. Dent. 2002, 87, 667–673. [Google Scholar] [CrossRef]
- Rohani, B. Oral manifestations in patients with diabetes mellitus. World J. Diabetes 2019, 10, 485–489. [Google Scholar] [CrossRef]
- Ito, K.; Izumi, N.; Funayama, S.; Nohno, K.; Katsura, K.; Kaneko, N.; Inoue, M. Characteristics of medication-induced xerostomia and effect of treatment. PLoS ONE 2023, 18, e0280224. [Google Scholar] [CrossRef]
- Chandna, S.; Bathla, M. Oral manifestations of thyroid disorders and its management. Indian J. Endocrinol. Metab. 2011, 15, S113–S116. [Google Scholar] [CrossRef]
- Panebianco, M.; Marchese-Ragona, R.; Masiero, S.; Restivo, D.A. Dysphagia in neurological diseases: A literature review. Neurol. Sci. 2020, 41, 3067–3073. [Google Scholar] [CrossRef]
- Spencer, H.; Kramer, L.; Norris, C.; Osis, D. Effect of small doses of aluminum-containing antacids on calcium and phosphorus metabolism. Am. J. Clin. Nutr. 1982, 36, 32–40. [Google Scholar] [CrossRef]
- Bell, V.; Rodrigues, A.R.; Antoniadou, M.; Peponis, M.; Varzakas, T.; Fernandes, T. An Update on Drug-Nutrient Interactions and Dental Decay in Older Adults. Nutrients 2023, 15, 4900. [Google Scholar] [CrossRef]
- Beth-Tasdogan, N.H.; Mayer, B.; Hussein, H.; Zolk, O.; Peter, J.U. Interventions for managing medication-related osteonecrosis of the jaw. Cochrane Database Syst. Rev. 2022, 7, CD012432. [Google Scholar] [CrossRef]
- Sheiham, A.; Steele, J. Does the condition of the mouth and teeth affect the ability to eat certain foods, nutrient and dietary intake and nutritional status amongst older people? Public Health Nutr. 2001, 4, 797–803. [Google Scholar] [CrossRef]
- Saleedaeng, P.; Korwanich, N.; Muangpaisan, W.; Korwanich, K. Effect of Dysphagia on the Older Adults’ Nutritional Status and Meal Pattern. J. Prim. Care Community Health 2023, 14, 21501319231158280. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Choi, Y.; Jeong, H.S.; Lee, J.; Sung, J. Effect of different cooking methods on the content of vitamins and true retention in selected vegetables. Food Sci. Biotechnol. 2018, 27, 333–342. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.S.; Chen, T.C.; Verhoeff, M.C.; Lobbezoo, F.; Trulsson, M.; Fuh, J.L. An umbrella review on the association between factors of oral health and cognitive dysfunction. Ageing Res. Rev. 2023, 93, 102128. [Google Scholar] [CrossRef] [PubMed]
- Shimazaki, Y.; Egami, Y.; Matsubara, T.; Koike, G.; Akifusa, S.; Jingu, S.; Yamashita, Y. Relationship between obesity and physical fitness and periodontitis. J. Periodontol. 2010, 81, 1124–1131. [Google Scholar] [CrossRef] [PubMed]
- Inui, A.; Takahashi, I.; Sawada, K.; Naoki, A.; Oyama, T.; Tamura, Y.; Osanai, T.; Satake, A.; Nakaji, S.; Kobayashi, W. Teeth and physical fitness in a community-dwelling 40 to 79-year-old Japanese population. Clin. Interv. Aging 2016, 11, 873–878. [Google Scholar] [CrossRef] [PubMed]
- Anne Marie, U.; Murererehe, J.; Rehman, M.; Chittilla, M.; Uwambaye, P.; Razzaque, M.S. Oral manifestations of iron imbalance. Front. Nutr. 2023, 10, 1272902. [Google Scholar] [CrossRef] [PubMed]
- Tada, A.; Miura, H. The Relationship between Vitamin C and Periodontal Diseases: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 2472. [Google Scholar] [CrossRef]
- Clarke, R.; Grimley Evans, J.; Schneede, J.; Nexo, E.; Bates, C.; Fletcher, A.; Prentice, A.; Johnston, C.; Ueland, P.M.; Refsum, H.; et al. Vitamin B12 and folate deficiency in later life. Age Ageing 2004, 33, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez Gossweiler, A.; Martinez-Mier, E.A. Chapter 6: Vitamins and Oral Health. Monogr. Oral Sci. 2020, 28, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, M.; Sirtori, P.; Mangiavini, L.; Buzzi, S.; Cordani, C.; Zerni, M.F.; Wainwright, T.W.; Ursino, N.; Peretti, G.M.; Banfi, G. How Do Older Patients with End-Stage Osteoarthritis of the Hip Eat Prior to Hip Replacement? A Preliminary Snapshot That Highlights a Poor Diet. Nutrients 2023, 15, 4868. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, M.; Crespi, T.; Mazzocchi, M.; Petrillo, S.; Turco, C.; De Vecchi, E.; Riso, P.; Porrini, M.; Banfi, G.; Romagnoli, S.; et al. Oral iron powder for prehabilitation in hip and knee arthroplasty: A randomized controlled trial to optimize hemoglobin concentration. Nutr. Clin. Métabolisme 2023, 37, 241–246. [Google Scholar] [CrossRef]
- Briguglio, M.; Sirtori, P.; Mangiavini, L.; Wainwright, T.; Peretti, G.; Banfi, G. Undernutrition, sarcopenia, sarcopenic obesity, and sarcopenic undernutrition: A cross-sectional view on patients before total joint arthroplasty. Orthop. Nurs. 2024. [Google Scholar]
- WHO. Global Oral Health Status Report: Towards Universal Health Coverage for Oral Health by 2030; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Schmalz, G.; Reuschel, F.; Bartl, M.; Schmidt, L.; Runge, J.; Haak, R.; Goralski, S.; Roth, A.; Ziebolz, D. One Third of Patients before Endoprosthesis Implantation Show an Oral Focus as Potential Source of Infectious Complication-The Value of Pre-Operative Dental Risk Stratification in a German Cohort. J. Clin. Med. 2022, 11, 3686. [Google Scholar] [CrossRef]
- Rakow, A.; Perka, C.; Trampuz, A.; Renz, N. Origin and characteristics of haematogenous periprosthetic joint infection. Clin. Microbiol. Infect. 2019, 25, 845–850. [Google Scholar] [CrossRef]
- Fenske, F.; Kujat, B.; Krause, L.; Meyer, S.; Sander, A.K.; Repmann, J.; Neuhaus, M.; Haak, R.; Roth, A.; Lethaus, B.; et al. Preoperative dental screening can reduce periprosthetic infections of hip and knee endoprostheses in the first month after surgery: Results of a cohort study. Infection 2023, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Parahitiyawa, N.B.; Jin, L.J.; Leung, W.K.; Yam, W.C.; Samaranayake, L.P. Microbiology of odontogenic bacteremia: Beyond endocarditis. Clin. Microbiol. Rev. 2009, 22, 46–64. [Google Scholar] [CrossRef]
- Kohler, J.G.; Holte, A.J.; Glass, N.A.; Bedard, N.A.; Brown, T.S. Dental Screening in Elective Total Joint Arthroplasty: Risk Factors for Failure. J. Arthroplast. 2021, 36, 1548–1550. [Google Scholar] [CrossRef] [PubMed]
- De Sam Lazaro, S.L.; Nitschke Durben, A.M.; Kline, J.J. Barriers and Opportunities to Support the Oral Health of Older Adults: A Rapid Review of Health Policy and Systems. Int. J. Aging Hum. Dev. 2023, 96, 51–62. [Google Scholar] [CrossRef]
- Kossioni, A.E. Is Europe prepared to meet the oral health needs of older people? Gerodontology 2012, 29, e1230–e1240. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Ziebolz, D. The hypotheses of oral disease-associated perioprosthetic joint infections to understand the role of oral health for endoprostheses—A narrative review. Spec. Care Dentist 2023, 44, 328–338. [Google Scholar] [CrossRef]
- Briguglio, M.; Crespi, T.; Langella, F.; Riso, P.; Porrini, M.; Scaramuzzo, L.; Bassani, R.; Brayda-Bruno, M.; Berjano, P. Perioperative Anesthesia and Acute Smell Alterations in Spine Surgery: A “Sniffing Impairment” Influencing Refeeding? Front. Surg. 2022, 9, 785676. [Google Scholar] [CrossRef]
- Teramoto, S. The current definition, epidemiology, animal models and a novel therapeutic strategy for aspiration pneumonia. Respir. Investig. 2022, 60, 45–55. [Google Scholar] [CrossRef]
- Schmitter, M.; Essig, M.; Seneadza, V.; Balke, Z.; Schröder, J.; Rammelsberg, P. Prevalence of clinical and radiographic signs of osteoarthrosis of the temporomandibular joint in an older persons community. Dentomaxillofac. Radiol. 2010, 39, 231–234. [Google Scholar] [CrossRef]
- Jockusch, J.; Hahnel, S.; Sobotta, B.B.A.J.; Nitschke, I. The Effect of a Masticatory Muscle Training Program on Chewing Efficiency and Bite Force in People with Dementia. Int. J. Environ. Res. Public Health 2022, 19, 3778. [Google Scholar] [CrossRef] [PubMed]
- Nitschke, I.; Nitschke, S.; Haffner, C.; Sobotta, B.A.J.; Jockusch, J. On the Necessity of a Geriatric Oral Health Care Transition Model: Towards an Inclusive and Resource-Oriented Transition Process. Int. J. Environ. Res. Public Health 2022, 19, 6148. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Lenzen, C.; Reuschel, F.; Fenske, F.; Haak, R.; Goralski, S.; Roth, A.; Ziebolz, D. Lack of oral health awareness and interdisciplinary dental care: A survey in patients prior to endoprosthesis and orthopaedic centres in Germany. BMC Oral Health 2023, 23, 92. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Mobile Technologies for Oral Health: An Implementation Guide; WHO: Geneva, Switzerland, 2021. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).