A National Study of Marital Status Differences in Early Uptake of COVID-19 Vaccine among Older Americans
Abstract
1. Introduction
2. Methods
2.1. Data and Sample
2.2. Measures
2.3. Statistical Analyses
3. Results
3.1. Descriptive Statistics
3.2. Marital Status Differences in COVID-19 Vaccination
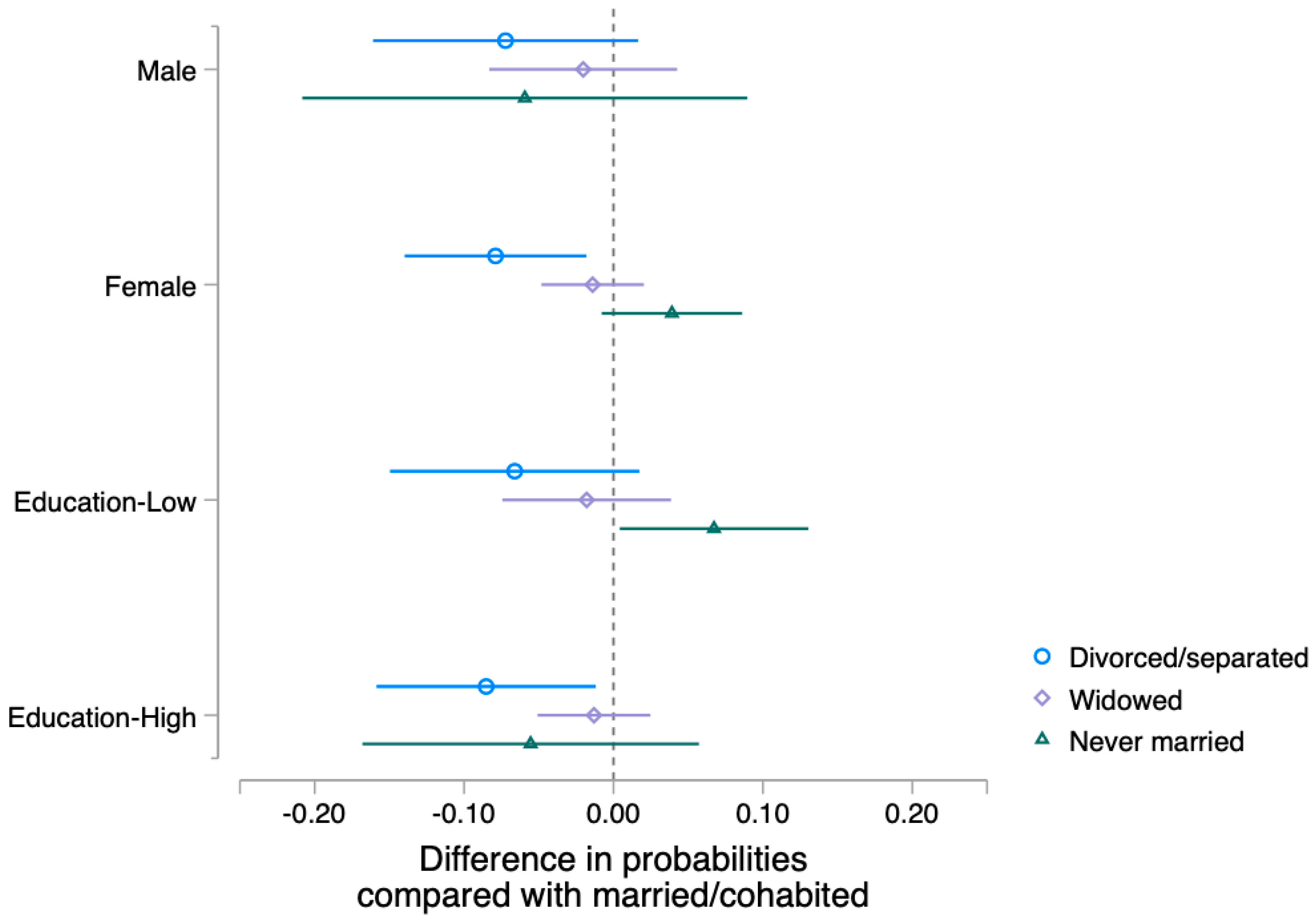
3.3. Gender and Educational Differences
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Center for Immunization and Respiratory Diseases. Background Rationale and Evidence for Public Health Recommendations for Fully Vaccinated People. 2021. Available online: https://stacks.cdc.gov/view/cdc/104739 (accessed on 7 June 2023).
- Centers for Disease Control and Prevention. COVID Data Tracker. 2023. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccination-demographics-trends (accessed on 7 June 2023).
- Ndugga, N.; Hill, L.; Artiga, S.; Parker, N.; Latest Data on COVID-19 Vaccinations by Race/Ethnicity. Kais Family Found 2021. Available online: https://covid-19archive.org/files/original/f90f767bdd1cd10911587853d70a6320f29bf9b7.pdf (accessed on 7 June 2023).
- Liu, H.; Umberson, D.J. The Times They Are a Changin’: Marital Status and Health Differentials from 1972 to 2003. J. Health Soc. Behav. 2008, 49, 239–253. [Google Scholar] [CrossRef] [PubMed]
- Umberson, D.; Crosnoe, R.; Reczek, C. Social Relationships and Health Behavior Across Life Course. Annu. Rev. Sociol. 2010, 36, 139–157. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.M.; Ajilore, O. Can Marriage Reduce Risky Health Behavior for African-Americans? J. Fam. Econ. Issues 2011, 32, 191–203. [Google Scholar] [CrossRef]
- Liu, H.; Waite, L. Bad marriage, broken heart? Age and gender differences in the link between marital quality and cardiovascular risks among older adults. J. Health Soc. Behav. 2014, 55, 403–423. [Google Scholar] [CrossRef]
- Sbarra, D.A. Marriage protects men from clinically meaningful elevations in C-reactive protein: Results from the National Social Life, Health, and Aging Project (NSHAP). Psychosom. Med. 2009, 71, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, J.E.; Gardner, C.O.; Kendler, K.S. Marriage and reductions in men’s alcohol, tobacco, and cannabis use. Psychol. Med. 2020, 50, 2634–2640. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Hayward, M.D. Gender, the Marital Life Course, and Cardiovascular Disease in Late Midlife. J. Marriage Fam. 2006, 68, 639–657. [Google Scholar] [CrossRef]
- Roxburgh, S. Race, Class, and Gender Differences in the Marriage-Health Relationship. Race Gend. Class 2014, 21, 7–31. [Google Scholar]
- Broman, C.L. Marital Quality in Black and White Marriages. J. Fam. Issues 2005, 26, 431–441. [Google Scholar] [CrossRef]
- Waite, L.J.; Gallagher, M. The Case for Marriage: Why Married People Are Happier, Healthier and Better off Financially; Doubleday: New York, NY, USA, 2000. [Google Scholar]
- Williams, K.; Umberson, D. Marital status, marital transitions, and health: A gendered life course perspective. J. Health Soc. Behav. 2004, 45, 81–98. [Google Scholar] [CrossRef]
- Umberson, D.; Thomeer, M.B.; Williams, K. Family Status and Mental Health: Recent Advances and Future Directions. In Handbook of the Sociology of Mental Health; Handbooks of Sociology and Social Research; Aneshensel, C.S., Phelan, J.C., Bierman, A., Eds.; Springer: Dordrecht, The Netherlands, 2013. [Google Scholar] [CrossRef]
- Ernsting, A.; Knoll, N.; Schneider, M.; Schwarzer, R. The enabling effect of social support on vaccination uptake via self-efficacy and planning. Psychol. Health Med. 2015, 20, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Jaspal, R.; Breakwell, G.M. Social support, perceived risk and the likelihood of COVID-19 testing and vaccination: Cross-sectional data from the United Kingdom. Curr. Psychol. 2022, 41, 492–504. [Google Scholar] [CrossRef] [PubMed]
- Nagata, J.M.; Hernández-Ramos, I.; Kurup, A.S.; Albrecht, D.; Vivas-Torrealba, C.; Franco-Paredes, C. Social determinants of health and seasonal influenza vaccination in adults ≥65 years: A systematic review of qualitative and quantitative data. BMC Public Health 2013, 13, 388. [Google Scholar] [CrossRef] [PubMed]
- Abramson, Z.H.; Cohen-Naor, V. Factors associated with performance of influenza immunization among the elderly. Isr. Med. Assoc. J. 2000, 2, 902–907. [Google Scholar]
- Damiani, G.; Federico, B.; Visca, M.; Agostini, F.; Ricciardi, W. The impact of socioeconomic level on influenza vaccination among Italian adults and elderly: A cross-sectional study. Prev. Med. 2007, 45, 373–379. [Google Scholar] [CrossRef]
- Peña-Rey, I.; Pérez-Farinós, N.; Sarría-Santamera, A. Factors associated with influenza vaccination among elderly Spanish women. Public Health 2004, 118, 582–587. [Google Scholar] [CrossRef]
- Sarría-Santamera, A.; Timoner, J. Influenza vaccination in old adults in Spain. Eur. J. Public Health 2003, 13, 133–137. [Google Scholar] [CrossRef]
- Gauthey, L.; Toscani, L.; Chamot, E.; Larequi, T.; Robert, C.F. Influenza vaccination coverage in the geriatric population of the State of Geneva, Switzerland. Eur. J. Public Health 1999, 9, 36–40. [Google Scholar] [CrossRef]
- Nindrea, R.D.; Usman, E.; Katar, Y.; Sari, N.P. Acceptance of COVID-19 vaccination and correlated variables among global populations: A systematic review and meta-analysis. Clin. Epidemiol. Glob. Health 2021, 12, 100899. [Google Scholar] [CrossRef]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef]
- National Health and Aging Trends Study (Rounds 1–11). Johns Hopkins University Bloomberg School of Public Health and the University of Michigan. 2022. Available online: https://www.nhats.org/ (accessed on 7 June 2023).
- Brown, S.L.; Lin, I.-F. The Gray Divorce Revolution: Rising Divorce among Middle-Aged and Older Adults, 1990–2010. J. Gerontol. Ser. B 2012, 67, 731–741. [Google Scholar] [CrossRef] [PubMed]
- Gurrentz, B.; Mayol-Garcia, Y. Marriage, Divorce, Widowhood Remain Prevalent among Older Populations. US Census. 2021. Available online: https://www.census.gov/library/stories/2021/04/love-and-loss-among-older-adults.html (accessed on 7 June 2023).
- Freedman, V.A.; Hu, M.; Kasper, J.D. Changes in Older Adults’ Social Contact during the COVID-19 Pandemic. J. Gerontol. Ser. B 2022, 77, e160–e166. [Google Scholar] [CrossRef]
- King, V.; Scott, M.E. A comparison of cohabiting relationships among older and younger adults. J. Marriage Fam. 2005, 67, 271–285. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a Two-Item Depression Screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Friedman, B.; Conwell, Y.; Fiscella, K. Validity of the Patient Health Questionnaire 2 (PHQ-2) in Identifying Major Depression in Older People. J. Am. Geriatr. Soc. 2007, 55, 596–602. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef]
- Mize, T.D. Best practices for estimating, interpreting, and presenting nonlinear interaction effects. Sociol. Sci. 2019, 6, 81–117. [Google Scholar] [CrossRef]
- U.S. Census Bureau. American Community Survey 1-Year Estimates. 2023. Available online: https://data.census.gov/ (accessed on 7 June 2023).
- National Center for Immunization and Respiratory Diseases. 5 Reasons It Is Important for Adults to Get Vaccinated. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/vaccines/adults/reasons-to-vaccinate.html (accessed on 7 June 2023).
- Dolby, T.; Finning, K.; Baker, A.; Fowler-Dowd, L.; Khunti, K.; Razieh, C.; Yates, T.; Nafilyan, V. Monitoring sociodemographic inequality in COVID-19 vaccination uptake in England: A national linked data study. J. Epidemiol. Community Health 2022, 76, 646–652. [Google Scholar] [CrossRef]
- Robinson, E.; Jones, A.; Lesser, I.; Daly, M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine 2021, 39, 2024–2034. [Google Scholar] [CrossRef]
- National Center for Immunization and Respiratory Diseases. Benefits of Getting A COVID-19 Vaccine. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/vaccine-benefits.html (accessed on 7 June 2023).
- Sbarra, D.A. Divorce and health: Current trends and future directions. Psychosom. Med. 2015, 77, 227. [Google Scholar] [CrossRef]
- South, S.J. The Geographic Context of Divorce: Do Neighborhoods Matter? J. Marriage Fam. 2004, 63, 755–766. [Google Scholar] [CrossRef]
- Sarkisian, N.; Gerstel, N. Does singlehood isolate or integrate? Examining the link between marital status and ties to kin, friends, and neighbors. J. Soc. Pers. Relatsh. 2016, 33, 361–384. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef]
- Guay, M.; Maquiling, A.; Chen, R.; Lavergne, V.; Baysac, D.-J.; Racine, A.; Dubé, E.; MacDonald, S.E.; Gilbert, N.L. Measuring inequalities in COVID-19 vaccination uptake and intent: Results from the Canadian Community Health Survey 2021. BMC Public Health 2022, 22, 1708. [Google Scholar] [CrossRef] [PubMed]

| Unweighted N (Weighted %) | 95% Confidence Interval | U.S. Elderly Population Reference (65 and Older) a | ||
|---|---|---|---|---|
| Vaccinated | 2867 (90.4%) | (88.5% | 92.0%) | 94.2% e |
| Marital Status | ||||
| Married | 1374 (50.4%) | (48.2% | 52.6%) | 31,490,252 (56.31%) |
| Cohabited | 63 (2.4%) | (1.8% | 3.3%) | N.A. b |
| Divorced/separated | 451 (14.1%) | (12.9% | 15.5%) | 9,072,576 (16.22%) |
| Widowed | 1177 (29.8%) | (27.9% | 31.7%) | 11,743,430 (21.00%) |
| Never married | 115 (3.3%) | (2.6% | 4.1%) | 3,616,455 (6.47%) |
| Gender | ||||
| Male | 1334 (44.3%) | (42.0% | 46.7%) | 25,191,742 (45.07%) |
| Female | 1846 (55.7%) | (53.3% | 58.0%) | 30,700,272 (54.93%) |
| Education | ||||
| Less than high school | 498 (12.8%) | (11.1% | 14.6%) | 7,015,917 (12.55%) |
| High school diploma | 1032 (31.0%) | (28.3% | 33.8%) | 16,801,639 (30.06%) |
| Some college or Bachelor’s degree | 653 (22.3%) | (20.5% | 24.2%) | 24,432,134 (43.71%) |
| Graduate or prof. degree | 997 (34.0%) | (30.7% | 37.4%) | 7,642,324 (13.67%) |
| Age | ||||
| 65 to 69 | N/A | N/A | N/A | 18,351,785 (32.83%) |
| 70 to 74 | 430 (28.9%) | (26.8% | 31.1%) | 15,426,419 (27.60%) |
| 75 to 79 | 950 (32.8%) | 30.6% | 35.1%) | 9,872,768 (17.66%) |
| 80 to 84 | 796 (20.1%) | (18.5% | 21.8%) | 6,278,369 (11.23%) |
| 85 to 89 | 576 (11.5%) | (10.5% | 12.5%) | 5,962,673 (10.67%) |
| 90+ | 428 (6.7%) | (6.0% | 7.4%) | N.A. c |
| Race-ethnicity | ||||
| Non-Hispanic White | 2296 (80.7%) | (77.9% | 83.2%) | 41,494,577 (74.24%) |
| Non-Hispanic Black | 648 (8.1%) | (7.1% | 9.3%) | 5,138,453 (9.19%) |
| Hispanic | 162 (7.6%) | (5.8% | 9.9%) | 5,045,939 (9.03%) d |
| Other or multiple | 74 (3.6%) | (2.6% | 4.9%) | 4,213,045 (7.54%) |
| Region | ||||
| South | 1274 (40.1%) | (36.8% | 41.6%) | |
| Northeast | 486 (15.3%) | (15.4% | 19.6%) | |
| Midwest | 831 (26.1%) | (20.4% | 24.4%) | |
| West | 589 (18.5%) | (19.7% | 22.6%) | |
| Importance of religious services | ||||
| Not so important | 916 (28.8%) | (30.5% | 35.4%) | |
| Somewhat important | 626 (19.7%) | (18.6% | 22.5%) | |
| Very important | 1638 (51.5%) | (43.5% | 49.7%) | |
| Walking as mode of transportation | ||||
| No | 1630 (51.3%) | (43.6% | 49.0%) | |
| Yes | 1550 (48.7%) | (51.0% | 56.4%) | |
| Depression (PHQ2 ≥ 3) | 387 (10.3%) | (9.1% | 11.8%) | |
| Anxiety (GAD2 ≥ 3) | 310 (9.0%) | (7.7% | 10.5%) | |
| Self-rated physical health | ||||
| Poor | 142 (3.9%) | (3.1% | 4.8%) | |
| Fair | 603 (16.5%) | (15.0% | 18.1%) | |
| Good | 1215 (37.6%) | (35.6% | 39.6%) | |
| Very good | 944 (31.6%) | (29.5% | 33.8%) | |
| Excellent | 276 (10.5%) | (9.0% | 12.1%) | |
| Health prevented attendance of religious services | ||||
| No | 2822 (88.7%) | (89.9% | 92.5%) | |
| Yes | 358 (11.3%) | (7.5% | 10.1%) | |
| Number of chronic conditions | Weighted Mean (SE) | |||
| 2.76 (0.02) | (2.72 | 2.81) | ||
| Not Vaccinated | Vaccinated | p-Value a | |
|---|---|---|---|
| Weighted % | Weighted % | ||
| Marital status | 0.003 | ||
| Married/cohabited | 41.9% | 54.0% | |
| Divorced/separated | 22.8% | 13.2% | |
| Widowed | 32.3% | 29.5% | |
| Never married | 2.9% | 3.3% | |
| Gender | 0.325 | ||
| Male | 40.8% | 44.7% | |
| Female | 59.2% | 55.3% | |
| Education b | <0.001 | ||
| Less than high school | 19.0% | 12.1% | |
| High school diploma | 38.6% | 30.2% | |
| Some college or Bachelor’s degree | 23.1% | 22.2% | |
| Graduate or prof. degree | 19.3% | 35.5% | |
| Age | 0.434 | ||
| 70 to 74 | 25.1% | 29.3% | |
| 75 to 79 | 36.2% | 32.4% | |
| 80 to 84 | 19.5% | 20.2% | |
| 85 to 89 | 11.0% | 11.5% | |
| 90+ | 8.2% | 6.5% | |
| Race | 0.390 | ||
| White | 77.1% | 81.1% | |
| Black | 8.5% | 8.1% | |
| Hispanic | 9.2% | 7.4% | |
| Other or multiple | 5.3% | 3.4% | |
| Region | |||
| South | 44.6% | 38.6% | 0.408 |
| Northeast | 13.3% | 17.9% | |
| Midwest | 20.5% | 22.5% | |
| West | 21.5% | 21.0% | |
| Importance of religious services | |||
| Not so important | 26.9% | 33.6% | 0.004 |
| Somewhat important | 15.7% | 21.0% | |
| Very important | 57.4% | 45.4% | |
| Walking as a mode of transportation | |||
| No | 54.2% | 45.4% | 0.029 |
| Yes | 45.8% | 54.6% | |
| Depression (PHQ2 ≥ 3) | 17.4% | 9.6% | <0.001 |
| Anxiety (GAD2 ≥ 3) | 10.9% | 8.8% | 0.320 |
| Self-rated physical health | 0.039 | ||
| Poor | 4.1% | 3.9% | |
| Fair | 17.6% | 16.4% | |
| Good | 43.6% | 36.9% | |
| Very Good | 22.0% | 32.6% | |
| Excellent | 12.7% | 10.2% | |
| Health prevented attendance of religious services | |||
| No | 86.8% | 91.7% | 0.011 |
| Yes | 13.2% | 8.3% | |
| Number of chronic conditions | Mean (SE) | Mean (SE) | |
| 2.78 (0.12) | 2.76 (0.02) | 0.907 | |
| Marital Status | Unadjusted OR (95% CI) a | Adjusted OR (95% CI) b |
|---|---|---|
| Married/cohabiting Ref. | ||
| Divorced/separated | 0.45 (0.28–0.72) | 0.45 (0.27–0.77) |
| Widowed | 0.71 (0.49–1.02) | 0.80 (0.53–1.21) |
| Never married | 0.88 (0.33–2.35) | 0.93 (0.33–2.60) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.; Nowak, G.R., III; Wang, J.; Luo, Z. A National Study of Marital Status Differences in Early Uptake of COVID-19 Vaccine among Older Americans. Geriatrics 2023, 8, 69. https://doi.org/10.3390/geriatrics8040069
Liu H, Nowak GR III, Wang J, Luo Z. A National Study of Marital Status Differences in Early Uptake of COVID-19 Vaccine among Older Americans. Geriatrics. 2023; 8(4):69. https://doi.org/10.3390/geriatrics8040069
Chicago/Turabian StyleLiu, Hui, Gerald Roman Nowak, III, Juwen Wang, and Zhehui Luo. 2023. "A National Study of Marital Status Differences in Early Uptake of COVID-19 Vaccine among Older Americans" Geriatrics 8, no. 4: 69. https://doi.org/10.3390/geriatrics8040069
APA StyleLiu, H., Nowak, G. R., III, Wang, J., & Luo, Z. (2023). A National Study of Marital Status Differences in Early Uptake of COVID-19 Vaccine among Older Americans. Geriatrics, 8(4), 69. https://doi.org/10.3390/geriatrics8040069





