Effects of Modified-Otago Exercise Program on Four Components of Actual Balance and Perceived Balance in Healthy Older Adults
Abstract
:1. Introduction
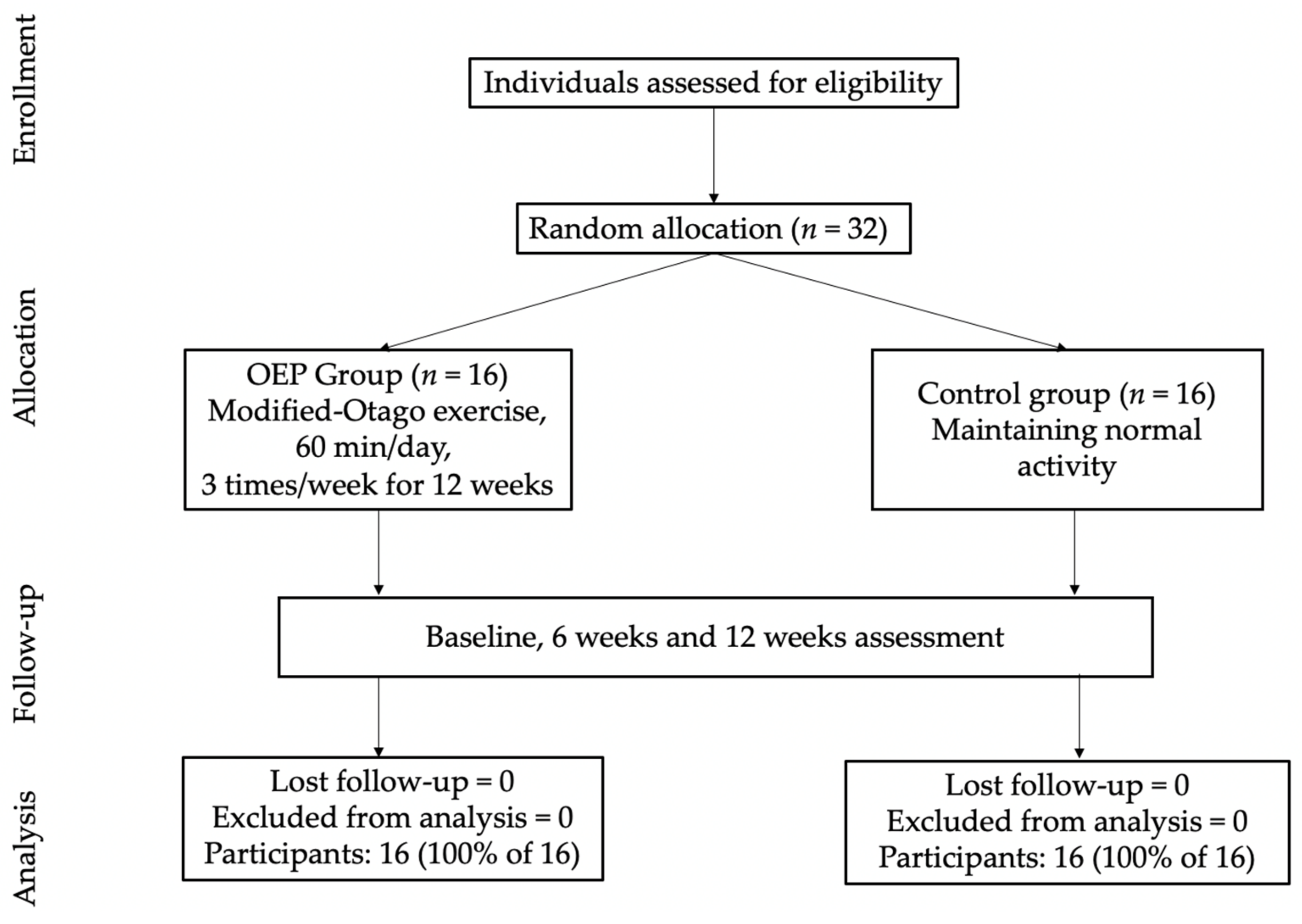
2. Materials and Methods
2.1. Participants
2.2. Intervention
2.3. Outcome Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gill, T.; Taylor, A.W.; Pengelly, A. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology 2005, 51, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P. Fall-Induced Injuries and Deaths Among Older Adults. JAMA 1999, 281, 1895–1899. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z.; Josephson, K.R.; Robbins, A.S. Falls in the nursing home. Ann. Intern Med. 1994, 121, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.K. Imbalanced. Am. J. Phys. Med. Rehabil. 2017, 96, 55–59. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Woollacott, M.H. Motor control: Translating Research into Clinical Practice; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007. [Google Scholar]
- Lin, H.W.; Bhattacharyya, N. Balance disorders in the elderly: Epidemiology and functional impact. Laryngoscope 2012, 122, 1858–1861. [Google Scholar] [CrossRef]
- Cuevas-Trisan, R. Balance Problems and Fall Risks in the Elderly. Clin. Geriatr. Med. 2019, 35, 173–183. [Google Scholar] [CrossRef]
- Campbell, A.; Robertson, M. Otago Exercise Programme to Prevent Falls in Older People: A Home-Based, Individually Tailored Strength and Balance Retraining Program; ACC Thinksafe: Wellington, New Zealand, 2003. [Google Scholar]
- Liu-Ambrose, T.; Donaldson, M.G.; Ahamed, Y.; Graf, P.; Cook, W.L.; Close, J.; Lord, S.R.; Khan, K.M. Otago Home-Based Strength and Balance Retraining Improves Executive Functioning in Older Fallers: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2008, 56, 1821–1830. [Google Scholar] [CrossRef]
- Kocic, M.; Stojanovic, Z.; Nikolic, D.; Lazovic, M.; Grbic, R.; Dimitrijevic, L.; Milenkovic, M. The effectiveness of group Otago exercise program on physical function in nursing home residents older than 65 years: A randomized controlled trial. Arch. Gerontol. Geriatr. 2018, 75, 112–118. [Google Scholar] [CrossRef]
- Bjerk, M.; Brovold, T.; Skelton, D.A.; Liu-Ambrose, T.; Bergland, A. Effects of a falls prevention exercise programme on health-related quality of life in older home care recipients: A randomised controlled trial. Age Ageing 2019, 48, 213–219. [Google Scholar] [CrossRef]
- Thomas, S.; Mackintosh, S.; Halbert, J. Does the ‘Otago exercise programme’ reduce mortality and falls in older adults?: A systematic review and meta-analysis. Age Ageing 2010, 39, 681–687. [Google Scholar] [CrossRef] [Green Version]
- Chiu, H.L.; Yeh, T.T.; Lo, Y.T.; Liang, P.J.; Lee, S.C. The effects of the Otago Exercise Programme on actual and perceived balance in older adults: A meta-analysis. PLoS ONE 2021, 16, e0255780. [Google Scholar] [CrossRef]
- Myers, A.M.; Powell, L.E.; Maki, B.E.; Holliday, P.J.; Brawley, L.R.; Sherk, W. Psychological Indicators of Balance Confidence: Relationship to Actual and Perceived Abilities. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1996, 51A, M37–M43. [Google Scholar] [CrossRef]
- Morris, J.N.; Hardman, A.E. Walking to health. Sports Med. 1997, 23, 306–332. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Brown, W.J.; Clemes, S.A.; De Cocker, K.; Giles-Corti, B.; Hatano, Y.; Inoue, S.; Matsudo, S.M.; Mutrie, N.; et al. How many steps/day are enough? For adults. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 79. [Google Scholar] [CrossRef]
- Marshall, S.J.; Levy, S.S.; Tudor-Locke, C.E.; Kolkhorst, F.W.; Wooten, K.M.; Ji, M.; Macera, C.A.; Ainsworth, B.E. Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 min. Am. J. Prev. Med. 2009, 36, 410–415. [Google Scholar] [CrossRef]
- Okubo, Y.; Osuka, Y.; Jung, S.; Figueroa, R.; Tsujimoto, T.; Aiba, T.; Kim, T.; Tanaka, K. Effects of walking on physical and psychological fall-related factors in community-dwelling older adults: Walking versus balance program. J. Phys. Fit. Sports Med. 2014, 3, 515–524. [Google Scholar] [CrossRef]
- Okubo, Y.; Osuka, Y.; Jung, S.; Rafael, F.; Tsujimoto, T.; Aiba, T.; Kim, T.; Tanaka, K. Walking can be more effective than balance training in fall prevention among community-dwelling older adults. Geriatr. Gerontol. Int. 2016, 16, 118–125. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Macpherson, J.M.; Horak, F.B. Posture. Princ. Neural Sci. 2013, 5, 935–958. [Google Scholar]
- Bergquist, R.; Weber, M.; Schwenk, M.; Ulseth, S.; Helbostad, J.L.; Vereijken, B.; Taraldsen, K. Performance-based clinical tests of balance and muscle strength used in young seniors: A systematic literature review. BMC Geriatr. 2019, 19, 9. [Google Scholar] [CrossRef]
- Berg, K.; Wood-Dauphinee, S.; Williams, J.I. The Balance Scale: Reliability assessment with elderly residents and patients with an acute stroke. Scand. J. Rehabil. Med. 1995, 27, 27–36. [Google Scholar] [PubMed]
- Martins, A.C.; Guia, D.; Saraiva, M.; Pereira, T. Effects of A “Modified” Otago Exercise Program on the Functional Abilities and Social Participation of Older Adults Living in the Community—The AGA@4life Model. Int. J. Environ. Res. Public Health 2020, 17, 1258. [Google Scholar] [CrossRef] [PubMed]
- Harter, R.A.; Pickerill, M.L. Validity and Reliability of Limits-of-Stability Testing: A Comparison of 2 Postural Stability Evaluation Devices. J. Athl. Train. 2011, 46, 600–606. [Google Scholar] [CrossRef]
- Iliffe, S.; Kendrick, D.; Morris, R.; Griffin, M.; Haworth, D.; Carpenter, H.; Masud, T.; Skelton, D.A.; Dinan-Young, S.; Bowling, A.; et al. Promoting physical activity in older people in general practice: ProAct65+ cluster randomised controlled trial. Br. J. Gen. Pract. 2015, 65, e731–e738. [Google Scholar] [CrossRef]
- Rejeski, W.J.; Brubaker, P.H.; Goff, D.C., Jr.; Bearon, L.B.; McClelland, J.W.; Perri, M.G.; Ambrosius, W.T. Translating weight loss and physical activity programs into the community to preserve mobility in older, obese adults in poor cardiovascular health. Arch. Intern. Med. 2011, 171, 880–886. [Google Scholar] [CrossRef]
- Leem, S.-H.; Kim, J.-H.; Lee, B.-H. Effects of Otago exercise combined with action observation training on balance and gait in the old people. J. Exerc. Rehabil. 2019, 15, 848–854. [Google Scholar] [CrossRef]
- Liew, L.K.; Tan, M.P.; Tan, P.J.; Mat, S.; Majid, L.A.; Hill, K.D.; Mazlan, M. The Modified Otago Exercises Prevent Grip Strength Deterioration Among Older Fallers in the Malaysian Falls Assessment and Intervention Trial (MyFAIT). J. Geriatr. Phys. Ther. 2019, 42, 123–129. [Google Scholar] [CrossRef]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta- analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef]
- Faraldo-García, A.; Santos-Pérez, S.; Rossi-Izquierdo, M.; Lirola-Delgado, A.; Vaamonde-Sánchez-Andrade, I.; del-Río-Valeiras, M.; Soto-Varela, A. Posturographic limits of stability can predict the increased risk of falls in elderly patients with instability? Acta Oto-Laryngol. 2016, 136, 1125–1129. [Google Scholar] [CrossRef]
- Melzer, I. Postural stability in the elderly: A comparison between fallers and non-fallers. Age Ageing 2004, 33, 602–607. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Richman, D.; Powell, L. Falls Efficacy as a Measure of Fear of Falling. J. Gerontol. 1990, 45, P239–P243. [Google Scholar] [CrossRef]
- French, D.P.; Sutton, S. Reactivity of measurement in health psychology: How much of a problem is it? What can be done about it? Br. J. Health Psychol. 2010, 15, 453–468. [Google Scholar] [CrossRef]
- Waters, L.; Reeves, M.; Fjeldsoe, B.; Eakin, E. Control Group Improvements in Physical Activity Intervention Trials and Possible Explanatory Factors: A Systematic Review. J. Phys. Act. Health 2012, 9, 884–895. [Google Scholar] [CrossRef]
- Granacher, U.; Bridenbaugh, S.A.; Muehlbauer, T.; Wehrle, A.; Kressig, R.W. Age-Related Effects on Postural Control under Multi-Task Conditions. Gerontology 2011, 57, 247–255. [Google Scholar] [CrossRef]
- Muehlbauer, T.; Besemer, C.; Wehrle, A.; Gollhofer, A.; Granacher, U. Relationship between Strength, Power and Balance Performance in Seniors. Gerontology 2012, 58, 504–512. [Google Scholar] [CrossRef]
- Ansdell, P.; Thomas, K.; Hicks, K.M.; Hunter, S.K.; Howatson, G.; Goodall, S. Physiological sex differences affect the integrative response to exercise: Acute and chronic implications. Exp. Physiol. 2020, 105, 2007–2021. [Google Scholar] [CrossRef]
- Schwartz, J.; Katz, S.A.; Fegley, R.W.; Tockman, M.S. Sex and race differences in the development of lung function. Am. Rev. Respir Dis 1988, 138, 1415–1421. [Google Scholar] [CrossRef]
- Martins, A.C.; Santos, C.; Silva, C.; Baltazar, D.; Moreira, J.; Tavares, N. Does modified Otago Exercise Program improves balance in older people? A systematic review. Prev. Med. Rep. 2018, 11, 231–239. [Google Scholar] [CrossRef]
- Cheng, S.-J.; Yang, Y.-R.; Cheng, F.-Y.; Chen, I.H.; Wang, R.-Y. The Changes of Muscle Strength and Functional Activities During Aging in Male and Female Populations. Int. J. Gerontol. 2014, 8, 197–202. [Google Scholar] [CrossRef]
- Nolan, M.; Nitz, J.; Choy, N.L.; Illing, S. Age-related changes in musculoskeletal function, balance and mobility measures in men aged 30–80 years. Aging Male 2010, 13, 194–201. [Google Scholar] [CrossRef]
| Variables | OEP (n = 16) | CT (n = 16) | p-Value | ||
|---|---|---|---|---|---|
| Mean | Std. Deviation | Mean | Std. Deviation | ||
| Age, years | 69.81 | 6.65 | 69.75 | 7.84 | 0.434 |
| Gender | |||||
| Female, % (n) | 93.75(15) | 87.5(14) | 0.544 | ||
| Male, % (n) | 6.25(1) | 12.5(2) | |||
| Height (cm) | 155.44 | 6.77 | 156.81 | 6.12 | 0.729 |
| Weight (kg) | 56.31 | 11.98 | 57.25 | 9.60 | 0.855 |
| BMI | 23.24 | 3.50 | 23.28 | 3.44 | 0.842 |
| Program | Activity | Intensity | Progressions | Duration | Frequency | ||
|---|---|---|---|---|---|---|---|
| Modified-OEP (this study) | Walking | Walking with correct pattern by physical therapist suggestion in the training room | Self-selected pace | - | Fifteen minutes | Three times a week (before original OEP 30 min) | |
| Original OEP [8] | Strengthening | Five leg muscle strengthening exercises; four levels of difficulty | Moderate; 8–10 repetitions before fatigue | Increase from one to two sets. Increased amount of ankle weight after 2 sets of 10 | Approximately 30 min total for exercises; exercises can be divided up over the day | At least three times a week | |
| Balance | Twelve balance retraining exercises; four levels of difficulty | Moderate; Each exercise at a level that the individual can safely perform unsupervised | Supported exercise to unsupported exercise | ||||
| (Optional) Walking | Advice about walking | Usual pace with usual walking aid | Walk indoors. Advance to walk outdoors when strength and balance improved | Thirty minutes; can be split into three ten-minute walks throughout the day | At least twice a week | ||
| Walking | Walking with correct pattern by physical therapist suggestion in the training room. | Self-selected pace | - | Fifteen minutes | Three times a week (after original OEP 30 min) | ||
| Balance Components | Assessment | OEP (n = 16) | CT (n = 16) | Effect Size | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Mid-Test | Post-Test | Pre-Test | Mid-Test | Post-Test | ANOVA Analysis p Value | ||||||||||||
| Mean | Std. Deviation | Mean | Std. Deviation | Mean | Std. Deviation | Mean | Std. Deviation | Mean | Std. Deviation | Mean | Std. Deviation | Time | Group | Time × Group | ||||
| Static | SLS | 1.64 | 0.89 | 0.93 a* | 0.33 | 0.62 bc* | 0.17 | 1.63 | 0.68 | 1.38 | 0.54 | 1.23 b | 0.55 | 0.000 | 0.028 | 0.029 | 0.111 | |
| mCTSIB | EO-firm | 0.63 | 0.27 | 0.47 a* | 0.09 | 0.47 b* | 0.12 | 0.58 | 0.26 | 0.64 | 0.27 | 0.69 | 0.36 | 0.579 | 0.111 | 0.009 | 0.146 | |
| EC-firm | 1.17 | 0.36 | 1.03 | 0.32 | 0.88 b* | 0.26 | 1.01 | 0.36 | 1.1 | 0.36 | 1.19 | 0.55 | 0.783 | 0.418 | 0.021 | 0.121 | ||
| EO-foam | 1.09 | 0.4 | 0.86 | 0.16 | 0.75 bc* | 0.2 | 1.04 | 0.42 | 1.03 | 0.38 | 1.15 | 0.64 | 0.095 | 0.155 | 0.003 | 0.182 | ||
| EC-foam | 2.74 | 0.58 | 2.51 | 0.54 | 2.05 bc* | 0.5 | 2.85 | 1 | 2.95 | 1.13 | 2.91 | 1.18 | 0.087 | 0.079 | 0.044 | 0.102 | ||
| Dynamic | BBS | 49.25 | 2.86 | 50.19 | 2.88 | 52.13 bc | 2.66 | 50.38 | 3.32 | 50.44 | 3.61 | 50.23 | 3.28 | 0.008 | 0.864 | 0.003 | 0.196 | |
| Proactive | TUG | 10.83 | 1.54 | 9.48 a* | 1.36 | 8.99 bc* | 1.09 | 11.19 | 1.57 | 11.30 | 1.65 | 10.91 | 1.17 | 0.000 | 0.005 | 0.000 | 0.282 | |
| Reactive | LOS | 26.31 | 7.48 | 41.81 a* | 8.8 | 59.31 bc* | 12.38 | 33.75 | 13.42 | 30.19 | 15.71 | 37.04 c | 12.63 | 0.000 | 0.022 | 0.000 | 0.510 | |
| Perceived | FES-I | 24.25 | 5.47 | 21.75 a | 4.59 | 19.0 bc* | 3.39 | 22.87 | 6.84 | 24.13 | 5.41 | 24.79 | 6.43 | 0.110 | 0.201 | 0.001 | 0.275 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khumpaneid, N.; Phoka, T.; Khongprasert, S. Effects of Modified-Otago Exercise Program on Four Components of Actual Balance and Perceived Balance in Healthy Older Adults. Geriatrics 2022, 7, 88. https://doi.org/10.3390/geriatrics7050088
Khumpaneid N, Phoka T, Khongprasert S. Effects of Modified-Otago Exercise Program on Four Components of Actual Balance and Perceived Balance in Healthy Older Adults. Geriatrics. 2022; 7(5):88. https://doi.org/10.3390/geriatrics7050088
Chicago/Turabian StyleKhumpaneid, Nichapa, Theerapat Phoka, and Surasa Khongprasert. 2022. "Effects of Modified-Otago Exercise Program on Four Components of Actual Balance and Perceived Balance in Healthy Older Adults" Geriatrics 7, no. 5: 88. https://doi.org/10.3390/geriatrics7050088
APA StyleKhumpaneid, N., Phoka, T., & Khongprasert, S. (2022). Effects of Modified-Otago Exercise Program on Four Components of Actual Balance and Perceived Balance in Healthy Older Adults. Geriatrics, 7(5), 88. https://doi.org/10.3390/geriatrics7050088






