1. Introduction
As part of a series of studies conducted by the senior author investigating language use in clinical contexts [
1,
2,
3], we conducted a study of healthcare provider (HCP) and caregiver expectations of older adult medical encounters. From their experience, HCPs have considerable understanding of processes that occur during interactions with older patients, but gaps remain in their delineating strategies and tactics to handle different situations. For instance, HCP beliefs about how an interaction should flow may or may not match those of patients or caregivers—with possible consequences regarding compliance with treatment. Similarly, the content or level of detail of the interaction may be perceived differently by HCPs and patients and caregivers depending on the situation. Further exploration of these gaps may inform HCPs on how to improve current patient encounters and improve the training of new HCPs. The focus of this paper is to study these gaps.
To gauge HCPs and caregivers’ expectations, we first conducted a rapid review and narrative synthesis [
4] of the literature on recommended practices for HCPs during interactions with older patients and their families. Informed by that work, we then administered a survey to gauge HCP and caregiver expectations of interactions with older patients.
2. Rapid Review and Narrative Synthesis
The purpose of a synthesis of the literature was to inform the design of the surveys. Following a similar approach to our previous work [
3], the review was intended to identify common elements of an encounter with an older patient and better understand the role of the caregiver. Though not as formal as a systematic review, we strove to consider a range of relevant studies that would allow us to develop realistic and varied scenarios for the survey.
2.1. Methods
We subjected PubMed and Google Scholar to a series of searches. For instance, we ran searches of {healthcare} {interaction} AND {age}, where the bracketed terms were instantiated with specific terminology (e.g., {healthcare} includes “healthcare” and “medical”; {age} includes “elderly patient”, “geriatric patient”, or “older patient”). From the results, we narrowed down the articles to those focused on HCP/older patient/caregiver interaction. We included English-only studies and, when possible, those reflecting more recent work. Our synthesis involved first reviewing abstracts to ensure that papers represented relevant content and then, for selected papers, carefully reading to extract main findings. We identified common themes across papers by noting recurring concepts and sought similarities among findings, especially where the situations presented in the studies differed.
2.2. Results
2.2.1. Elements of the Encounter
Any successful healthcare-related encounter includes elements such as relationship building, information exchange, and empathizing with the patient [
5]. Patients want HCPs to address their concerns, understand the “whole person” and social setting, and be understandable, approachable, and respectful [
6]. Basic competencies (“entrustable professional activities” [
7]) that HCPs need to demonstrate with their older patients include assisting them and their caregivers with medical decision making and providing age-appropriate consultation regarding treatment, medication management, and psychological and social concerns [
8]. Older adult advocates have recently recognized the five “M’s” of age-friendly care, which include a focus on multi-complexity (chronic conditions, advanced illness, complicated biopsychosocial needs), mind, mobility, medications, and what matters most (meaningful health outcome goals and care preferences) [
9].
2.2.2. Influence of Caregivers
The encounters between HCPs and older patients and their caregivers reflect many similar elements to those between HCPs and pediatric patients and their parents [
3]. Unlike pediatrics, though, older patients present with issues of futility, mortality, litigation, and possibly low prestige [
10,
11,
12,
13,
14]. The dynamic is characterized as the “physician–elderly patient–companion triad” in an older adult medical encounter [
15]. The third person in the dialog, generically the companion, but herein referred to as the caregiver [
16], often controls the dialog during encounters and facilitates the conversation [
17,
18]. The caregiver can take on roles such as advocate for the patient, passive participant, or even antagonist [
19,
20]. There are “coalitions” that form naturally during these encounters [
21], all in service of collaboration of care.
The role of the caregiver in an older adult medical encounter varies based on the five “M” patient characteristics [
9]. For example, in settings with dementia patients and presumably also whenever patients are otherwise compromised, caregivers tend to expect HCPs to attend to them [
22]. HCPs tend toward that focus of caregivers as they gain experience [
23], though other tools are also useful in assessing cognitive deficits [
24]. HCPs sharing treatment recommendations with caregivers can promote adherence [
25], but this offer must be made in the context of partnership [
26] and with clear expectations set [
27]. A competency framework has emerged for caregivers that HCPs should support [
28]. Improved triadic communication can result not only from better training of HCP knowledge and skills but also with a focus on the caregiver. For instance, caregivers’ health literacy influences their ability to navigate care for older patients [
29]. For cancer in particular, and likely other disease states and chronic illnesses, as well as end-of-life discussions, there may be “concordance” between caregivers and HCPs and between patients and HCPs [
30,
31]; discord would suggest communication patterns calling for improvement. Preliminary evidence shows that different priorities set by HCPs versus patients and caregivers causes conflicts in treatment decisions [
32] and different perceptions of how well HCPs communicate prognoses [
33]. In all of these studies, there are gaps among expectations and outcomes for different participants in the encounter.
There are roles played by specific diseases (if any) in the relationship between an HCP and caregiver, the focus on informal versus formal caregiving, and legal representation (e.g., guardianship vs. friendship). Further, an HCP may or may not have the legal right to provide medical information to the caregiver, depending on the older patient’s agency. In the work presented below, we treat the relationship as that of a supporter—present to assist the older patient where or when needed and integrated into the healthcare process [
34] but not necessarily to make medical decisions.
2.2.3. Different Providers
“Healthcare provider” is a broad term that includes members of an interprofessional team (physicians, nurses, nursing assistants, pharmacists, specialists, social workers). The form and function of communication with caregivers and patients for each member necessarily differs. A meta-analysis showed that pharmacists’ role in team-based healthcare focuses on safety and adherence to treatment [
35]. Core knowledge, skills, and attitudes (KSAs) may be needed in pharmacists’ training [
36], although full implementation of these competencies may be lagging [
37,
38]. Dentists recognize age-related oral health considerations [
39]. Mental health professionals address geriatric-specific concerns associated with chronic disease and cognitive decline [
40,
41]. Though family care physicians are on the front lines of medical assessment [
42,
43], a team approach is needed to maintain focus on accuracy [
44], to identify cognitive impairment [
45], and to avoid adverse drug events [
46]. Overall, there is a shortage of HCPs; there are too few relative to the growing need [
47,
48].
2.2.4. HCP Learning
Even a single home visit by novice HCPs, followed by reflection, has been found to lead to improved care [
49]. Other researchers have elaborated on this reflection and found increased awareness of the need for family and community support and a focus on unique aspects of geriatrics, such as mortality and ethical/moral challenges [
50,
51]. Though somewhat dated, studies have found that a learning module helps novice HCPs (such as student providers) to understand issues associated with communication and ageism [
52] and that these individuals can increase their understanding of physical decline and their comfort with eldercare issues [
53]. Specific interventions, such as completing a knowledge test or taking the perspective of someone aging, differently affect novice HCPs’ attitudes and empathy toward older patients [
54]. Some benefit may accrue by having these individuals engage in directed narratives, such as mind maps [
55] or theater [
56]. One literature review identified the potential of KSAs across multiple programs—coursework, mentoring, simulation, and clerkship [
57].
3. Survey
These literature-based findings suggest a range of considerations for HCPs during encounters with older patients. What the studies do not directly address is how closely HCPs and caregivers align in different, often challenging situations, yet their accord can be important for patients’ compliance with treatment. The goal of this part of the study was to identify situations with common understanding between HCPs and caregivers and those with mismatching ideas of how best to proceed with the geriatric encounter, with the intent of deriving best practices that can inform HCPs’ actions.
3.1. Methods
3.1.1. Materials Development
We developed a survey to gauge HCP and caregiver expectations of interactions with older patients. We started by creating scenarios, generated from case studies, the rapid review and narrative synthesis, and the first author’s clinical experience. Based on vignette analyses from medical education [
2], we structured scenarios using the following template:
[Initials] is a [age]-year-old [gender] who presents to [setting] with a chief complaint of [medical condition]. [Sentences about condition and symptoms, controlled or not]. [Statement about HCP imperative in the current situation].
Scenarios involved topics such as required changing of a patient’s long-used medication, pain and dependence on pain medication, new or worsening diagnosis, a necessary complex procedure or surgery, proper adherence to medication therapy, cost of medications and insurance, and disability. We evenly spread ages and genders of patients across scenarios.
A total of 28 scenarios—14 having female patients and a matching 14 having male patients—were targeted toward HCPs (see
Table S1 in Supplementary Materials). We adapted these scenarios into a parallel set for caregivers. First, we kept all details, but replaced descriptions of the patient (“a 66-year-old female”, “presenting to your practice…with his daughter, who is his primary caregiver”) with personal references (“You are a 66 year-old female”; “visiting the practice with your daughter, who takes care of you”). Second, details or terminology that caregivers might not know (“complaint of neuropathic pain”) were replaced with more common language (“shooting pain and tingling in the hands and feet”).
As we developed scenarios, we determined response options. Each pair of scenarios had a goal, determined by the topic. For instance, for the topic of adherence to medication, responses related to educating the patient on the importance of adherence. Similarly, for the topic of presenting a needed complex procedure, the responses related to discussing that need with patients. All responses were given using a sliding scale (slider bars provide visual cues and have been shown to be generally as effective as traditional Likert scales [
58]) from zero to 100, in response to the prompt, “Slide the marker to indicate how strongly you feel (0 = should not happen; 100 = should definitely happen) that ___ should take the action during the examination”, where “___” was “you” for HCP respondents and “the HCP” for caregivers. As was logical, we presented the same response set for each scenario.
We created two non-overlapping surveys, carefully arranging equivalent mixes of scenario types and patient ages and genders between survey variants. To avoid order effects, a given participant answered questions for each of the 14 scenarios, presented in random order; the choice of survey variant was administered was also randomized, as were response options.
3.1.2. Scenario Characteristics
Our intent was to seek expectations from HCPs and from caregivers of older patients about appropriate strategies when HCPs interact with older patients across different situations. We called these situations “scenarios” and characterized them using three overlapping criteria that reflected the content presented by, the tasks inherent in, and those individuals involved in the scenarios [
59]:
Content of scenario itself. We categorized scenarios into seven non-mutually exclusive buckets: those (i) requiring focused discussion or explanation; (ii)–(v) for which patients might be expected to be anxious, embarrassed, sad, upset or frustrated; (vi) for which patients might be trying to avoid medical care; and (vii) involving urgency.
Type of responses being asked of HCP or caregivers. Following our prior work, we derived 15 non-mutually-exclusive buckets (see
Table S2 in Supplementary Materials): those responses that (i) queried about an ability or need for
communication with the older patient in the situation; (ii) involved perceptions of need for
empathy; (iii) addressed
strategies for dealing with the older patient; (iv) addressed
tactics (more low-level actions than the general approach addressed by strategies); (v) focused on HCPs portraying
calm demeanor; (vi) focused on HCPs providing
comfort; (vii) focused on HCPs being
matter-of-fact; (viii) focused on HCPs providing
explanation; (ix) asked about any medical
education; (x) focused on HCPs demonstrating and maintaining
control; (xi) gauged
caregiver engagement; (xii) gauged
patient engagement; (xiii) gauged
reliance on others in the healthcare setting; (xiv) indicated a need for HCPs to
simplify the process; or (xv) indicated a need for HCPs to ensure
thoroughness of the process. We validated the assignments through a convenience group of 28 participants via Mechanical Turk (mTurk); an assignment of a response to a bucket was made only if agreed to by most (defined as greater than the median) participants.
Ages of patients in scenarios. Though any cutoff is somewhat arbitrary, patients generally rely more on caregivers as they age. We chose over-65, a common if not universal starting point for older patients, and used ages (i) 66–70, (ii) 71–75, (iii) 76–80, (iv) 81–85, and (v) 86–90.
3.1.3. Procedures
Participants. There were 51 HCPs and 50 caregivers. Participants were recruited using mTurk, an online service allowing enrollment in studies of individuals having self-identified, verified backgrounds. We required individuals to be employed in the healthcare industry when responding to the HCP survey or caring for patients 65 and older when responding to the caregiver survey. There was no age limit or other restriction on caregivers.
Survey Administration. Surveys were administered using Qualtrics (Provo, UT, USA). Each participant who was vetted as an HCP or a caregiver was sent a unique link through the mTurk service, presenting one randomly selected block of scenarios. Within the block, scenarios were presented randomly. Qualtrics automatically collected and labeled participant responses.
Statistical Analyses. Data were downloaded from Qualtrics and analyzed using the R statistical package (
www.r-project.org; accessed 22 May 2022). Aside from descriptive statistics (numbers, means), analyses were conducted using two-way analysis of variance to identify the influence of variables of interest for the particular research question. We report F statistics of differences in population means and consider an individual test to be significant at
p < 0.05.
Ethical Review. The study was reviewed and exempted by an Institutional Review Board at our institution.
3.2. Results
On average, participants required just under ten minutes to complete the survey, suggesting a low burden.
Table 1 and
Table 2 provide summary statistics on respondent characteristics. Though not all participants will have had experience with all scenarios presented, in these analyses, data from all healthcare respondents were pooled, and the same was done for caregivers.
Analysis showed no effect of survey variant on respondent ratings (F(1, 89) < 1, ns) nor any interaction with source of participants (HCPs, caregivers; F(1, 87) < 1, ns), so all responses were pooled.
Planned Research Questions
The ratings scale asked respondents to indicate how strongly they felt that each given response should (100) or should not (0) occur. Overall, the source affected the ratings—HCPs (72.4) versus caregivers (57.8) (F(1, 89) = 16.8,
p < 0.0001)—mirroring our previous findings of higher HCP ratings across scenarios [
3]. However, this average difference changed when planned queries were applied.
To identify how HCPs and caregivers differ in their approach to or expectations of a situation (based on values they assigned to different responses to different scenarios), we queried the data to address a number of research questions.
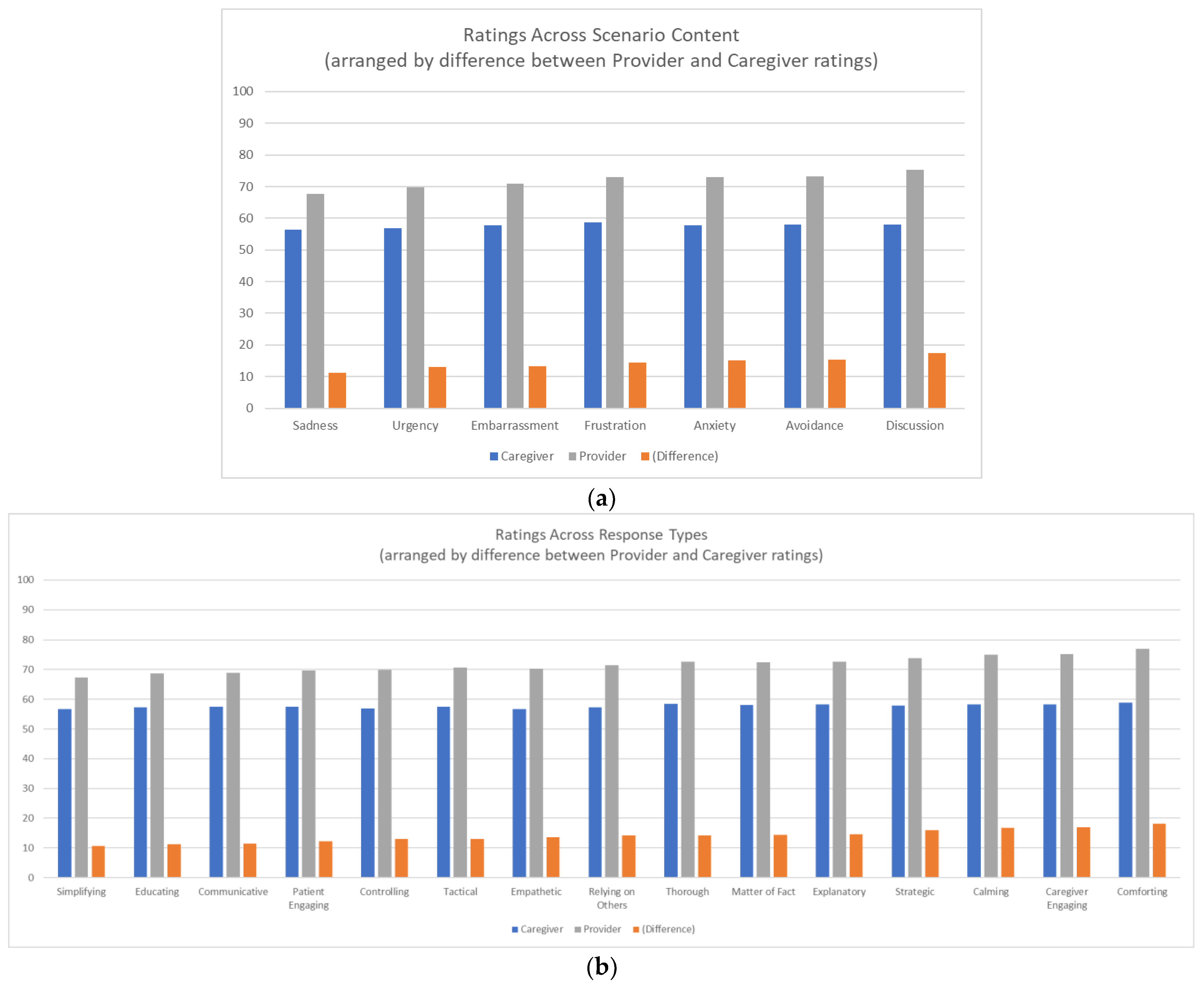
To begin, we asked if HCPs and caregivers differ in how to handle different situations. We found no main effect of content of the scenario; however, there were significant interactions between HCPs and caregivers for all different scenario contents (
Figure 1a) and for all different response types (
Figure 1b). Planned contrasts described next investigated how HCP and caregiver ratings are closer for certain scenario and response combinations than they are for others.
First we considered if HCPs and caregivers differ for discourse (involving communicative or empathetic response) versus active responses (strategic or tactical actions). The data show a large effect between HCPs and caregivers, where discourse ratings rise more over active ratings for HCPs than for caregivers. A similar pattern holds for which ratings rise more for comforting responses than for controlling responses, for scenarios involving discussion compared to urgency, and for both explanatory and thorough responses over simplifying responses for scenarios requiring focused discourse. Similarly, we considered if HCPs and caregivers differ for scenarios that require communication, for responses that are explanatory, thorough, or simplifying. The data show that HCPs value both explanation and thoroughness over simplification more than caregivers do. Additionally, for scenarios that involve patients avoiding versus not avoiding treatment, the data suggest HCPs value more thorough responses for avoidance scenarios than non-avoidance scenarios than do caregivers, though not for simplified, controlling, explanatory, educating, or matter-of-fact responses.
Next we considered scenarios involving affect. HCPs, relative to caregivers, value thorough responses for worry/anxiety scenarios more so than simplifying responses, compared to those scenarios that do not involve anxiety. HCPs value comforting and more engaging responses, as well as calming responses, more so in scenarios that do not involve sadness than those that do. HCPs value comforting responses for upset/frustration scenarios more so than caregivers compared to scenarios that do not involve upset/frustration. HCPs value simplifying and even more so thorough responses, compared to caregivers, in scenarios that do not involve sadness than scenarios that do. However, HCPs do not value comforting responses for embarrassment scenarios more than caregivers compared to those scenarios that do not involve embarrassment, nor matter-of-fact or calming responses.
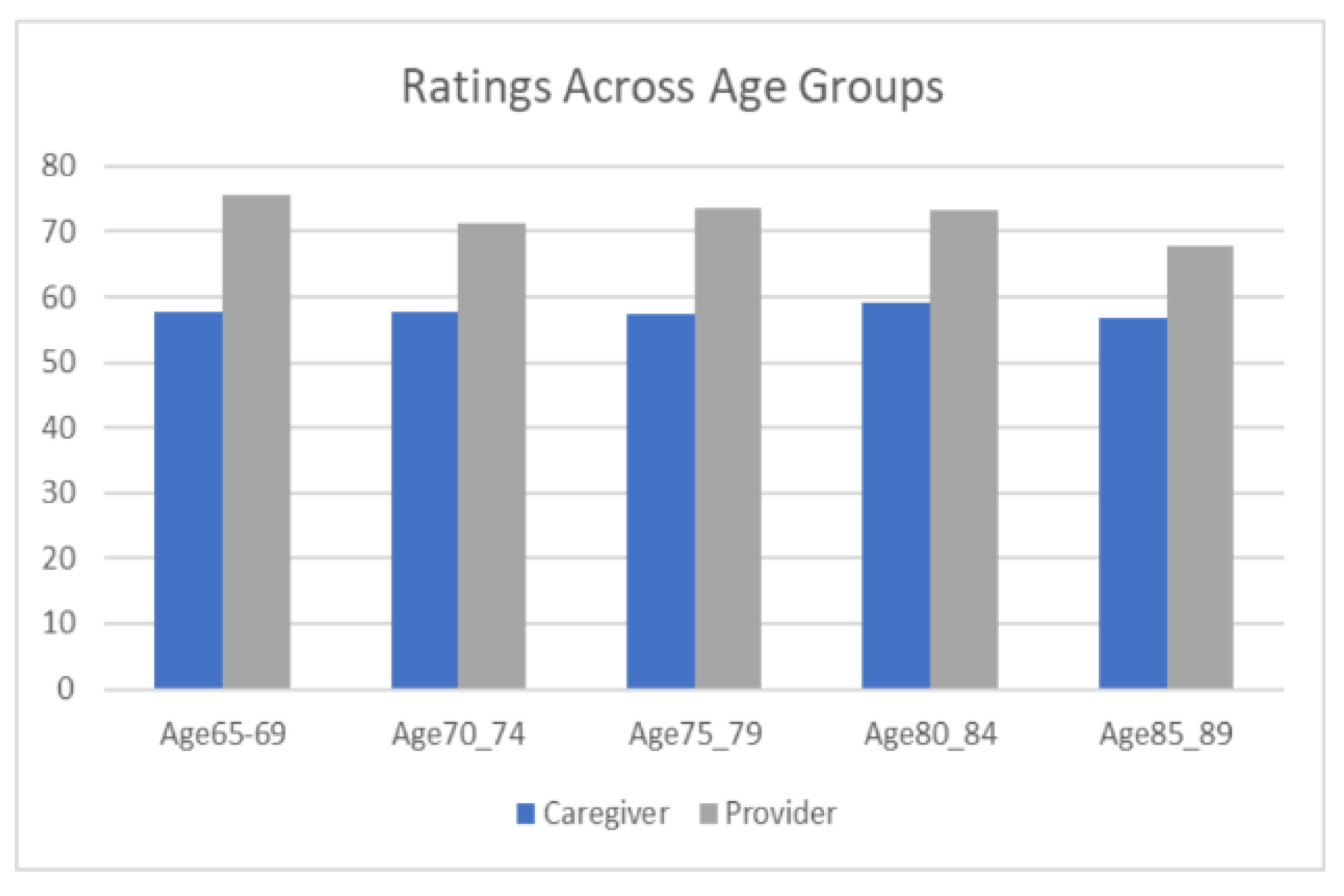
Finally we considered managing patients of different ages. There was no main effect of age of patient in the scenario, but a significant trend toward a narrower gap between HCPs and caregivers (
Figure 2). Specifically for engagement with the youngest (66–70 year old patients) and oldest (86–90) age groups, the data show caregiver ratings are equivalent for both age groups, but HCP ratings are higher for the youngest age group than the oldest. This finding is true for specific response types such as education, thoroughness, and patient engagement, though engagement with the caregiver increases more for the older age group than the younger age group. Relatedly, we considered if HCPs and caregivers differ in how they view participants in the scenario. Caregivers rate caregiver interactions equally with patient interactions, whereas HCPs rate caregiver interactions as more important than patient interactions.
4. Discussion
The results suggest that HCPs understand or are willing to provide additional support to patients, in comparison to caregivers, in situations (such as anxiety scenarios) where simplifying responses are important or for situations (such as embarrassment) where matter-of-factness is needed. Different situations call for greater focus on specific responses, whether comfort, calming, or explanation. We reasoned HCPs should be more aware of scenario-specific needs than caregivers. The data bear this reasoning out; there is a difference between HCPs and caregivers for different scenarios where specific types of responses are warranted.
Regarding a difference between HCPs and caregivers, across all scenarios, for specific types of responses, we reasoned HCPs would tend to value more detailed and matter-of-fact information exchange, given their greater medical knowledge, and caregivers less detailed and more explanatory or comforting information. The data show, however, that HCPs valued comforting responses over control responses, suggesting that they are aware of the needs of caregivers. Further, we expected HCPs and caregivers to value calming, comforting, and empathetic responses equally. The data show this expectation mostly holds, though HCPs rate calming, comforting, and empathetic responses less relevant for urgent scenarios, whereas caregivers show no differences among scenarios. In contrast, for explanatory, matter-of-fact, and thorough responses, there are few differences for HCPs across scenarios, in line with caregiver ratings.
Finally, regarding managing patients of different ages, we identified a trend toward a narrower gap between HCPs and caregivers, suggesting they are more in line with each other as patients age. HCP ratings generally declined as patients in the scenarios aged, although this finding may be a consequence of the content of those scenarios, with older patients experiencing worse medical situations. Nevertheless, the pattern did not hold for all types of responses; matter-of-fact and empathetic responses, for instance, were rated by HCPs about the same across patient age groups. We also looked specifically at engagement with the youngest and oldest age groups; we reasoned HCPs and caregivers would be more in line with a younger age group and differ in perceived needs from an older age group. The data support this reasoning. For scenarios that involve patients aged 86–90, we expected HCPs to see the same need to engage with caregivers as caregivers do, but a greater need to engage with patients. The data suggest HCPs significantly value engagement with patients for this age group more than caregivers. However, HCPs and caregivers value engagement with caregivers equally.
Limitations
There is a range of roles for caregivers that are not fully addressed in this work, including supportive tasks like medication monitoring, transportation, and providing companionship. There are also differing views of division of responsibilities for those roles between HCPs and caregivers [
60]. Further, our sampling method using mTurk likely did not lead to a representative sample of all types of HCPs or caregivers. In particular, in line with other studies [
61], physicians under-participated in this survey (
Table 1), and as well we note that fewer caregivers of the most elderly patients responded (
Table 2). Additional series of scenarios with a wider array of participants may identify other differences in expectations between HCPs and caregivers. Finally, to allow for parallel methodology with our pediatric study [
3], patients were not surveyed in this study, so their opinions on their own care were not directly taken into account.
5. Conclusions
HCPs and caregivers are not so different in how they perceive the geriatric encounter, with some exceptions. HCPs’ overall ratings were higher than caregivers, but this finding might be due to HCPs being more focused on the interaction with older patients than caregivers, or to a different interpretation of the instructions given. However, differences for specific situations are informative.
HCPs value being calm throughout an interaction, even more so than caregivers. HCPs value providing simple explanations when warranted, more so than caregivers, as in situations where patients are hesitant toward or avoid treatment or where they are embarrassed or anxious. HCPs are more attuned than caregivers to situations involving “younger” older patients, but HCPs and caregivers align as patients in the situations age. Even in those situations with much older patients, HCPs place greater value on addressing patients than do caregivers, though HCPs and caregivers place equal emphasis on addressing caregivers.
Practical Implications
HCPs, patients, and caregivers all value participation in research endeavors, though they bring different perspectives of application [
62]. There is thus reason to believe education and training following this work will have value. Training involves presenting situations for students to engage in; the more realistic the assessment of performance in those situations, the better transfer that is expected [
63]. A goal is to develop a suite of geriatric cases to allow students to hone their KSAs to meet expectations of their older patients and their caregivers. We also expect there are other unique populations to be considered, including people with special needs and underserved communities, to identify gaps in how interactions are perceived by HCPs and those patients and their caregivers.
Supplementary Materials
The following supporting information can be downloaded at:
https://www.mdpi.com/article/10.3390/geriatrics7050101/s1, Table S1: Scenarios. (Listed by content, but presented to participants in random order). Table S2: Response options and their mappings. (Alphabetical, but presented to participants in random order).
Author Contributions
Conceptualization, R.H.; methodology, P.S., K.D. and R.H.; software, P.S., K.D. and R.H.; validation, P.S.; formal analysis, R.H.; writing—original draft preparation, R.H.; writing—review and editing, P.S. and K.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the UNC Eshelman School of Pharmacy.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Biomedical Institutional Review Board of the University of North Carolina (protocol codes 17-2369, 18 September 2017; 20-1506, 2 June 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hubal, R.C.; Day, R.S. Informed consent procedures: An experimental test using a virtual character in a dialog systems training application. J. Biomed. Inform. 2006, 39, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Hubal, R.; McLaughlin, J.E. Vignette element analysis for automated generation of vignettes in pharmacy education. Educ. Health Prof. 2020, 3, 22–26. [Google Scholar] [CrossRef]
- Shah, P.; Donovan, K.; Rexrode, L.; Hubal, R. Pediatric patient interaction: Provider vs. parent expectations. J. Commun. Healthc. Strateg. Media Engagem. Glob. Health 2020, 13, 289–300. [Google Scholar] [CrossRef]
- Khangura, S.; Konnyu, K.; Cushman, R.; Grimshaw, J.; Moher, D. Evidence summaries: The evolution of a rapid review approach. Syst. Rev. 2012, 1, 10. [Google Scholar] [CrossRef]
- de Haes, H.; Bensing, J. Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient Educ. Couns. 2009, 74, 287–294. [Google Scholar] [CrossRef]
- King, A.; Hoppe, R.B. “Best practice” for patient-centered communication: A narrative review. J. Grad. Med. Educ. 2013, 5, 385–393. [Google Scholar] [CrossRef]
- Ten Cate, O. Nuts and bolts of entrustable professional activities. J. Grad. Med. Educ. 2013, 5, 157–178. [Google Scholar] [CrossRef]
- Leipzig, R.M.; Sauvigné, K.; Granville, L.J.; Harper, G.M.; Kirk, L.M.; Levine, S.A.; Mosqueda, L.; Parks, S.M.; Fernandez, H.M. What is a geriatrician? American Geriatrics Society and Association of Directors of Geriatric Academic Programs end-of-training entrustable professional activities for geriatric medicine. J. Am. Geriatr. Soc. 2014, 62, 924–929. [Google Scholar] [CrossRef]
- Wershof Schwartz, A.; Hawley, C.E.; Strong, J.V.; Phillips, S.C.; Amir, O.; Ludwin, B.M.; Ngoc Phung, E.T.; Moye, J. A workshop for interprofessional trainees using the geriatrics 5Ms framework. J. Am. Geriatr. Soc. 2020, 68, 1857–1863. [Google Scholar] [CrossRef]
- Album, D.; Westin, S. Do diseases have a prestige hierarchy? A survey among physicians and medical students. Soc. Sci. Med. 2008, 66, 182–188. [Google Scholar] [CrossRef]
- Bagri, A.S.; Tiberius, R. Medical student perspectives on geriatrics and geriatric education. J. Am. Geriatr. Soc. 2010, 58, 1994–1999. [Google Scholar] [CrossRef] [PubMed]
- King, B.J.; Roberts, T.J.; Bowers, B.J. Nursing student attitudes toward and preferences for working with older adults. Gerontol. Geriatr. Educ. 2013, 34, 272–291. [Google Scholar] [CrossRef] [PubMed]
- Riffin, C.; Wolff, J.L.; Estill, M.; Prabhu, S.; Pillemer, K.A. Caregiver needs assessment in primary care: Views of clinicians, staff, patients, and caregivers. J. Am. Geriatr. Soc. 2020, 68, 1262–1270. [Google Scholar] [CrossRef] [PubMed]
- Robbins, T.D.; Crocker-Buque, T.; Forrester-Paton, C.; Cantlay, A.; Gladman, J.R.F.; Gordon, A.L. Geriatrics is rewarding but lacks earning potential and prestige: Responses from the national medical student survey of attitudes to and perceptions of geriatric medicine. Age Ageing 2011, 40, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Adelman, R.D.; Greene, M.G.; Charon, R. The physician-elderly patient-companion triad in the medical encounter: The development of a conceptual framework and research agenda. Gerontologist 1987, 27, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Laidsaar-Powell, R.C.; Butow, P.N.; Bu, S.; Charles, C.; Gafni, A.; Lam, W.W.T.; Jansen, J.; McCaffery, K.J.; Shepherd, H.L.; Tattersall, M.H.N.; et al. Physician–patient–companion communication and decision-making: A systematic review of triadic medical consultations. Patient Educ. Couns. 2013, 91, 3–13. [Google Scholar] [CrossRef]
- Clayman, M.L.; Roter, D.; Wissow, L.S.; Bandeen-Roche, K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc. Sci. Med. 2005, 60, 1583–1591. [Google Scholar] [CrossRef]
- Hasselkus, B.R. Physician and family caregiver in the medical setting: Negotiation of care? J. Aging Stud. 1992, 6, 67–80. [Google Scholar] [CrossRef]
- Ishikawa, H.; Roter, D.L.; Yamazaki, Y.; Takayama, T. Physician–elderly patient–companion communication and roles of companions in Japanese geriatric encounters. Soc. Sci. Med. 2005, 60, 2307–2320. [Google Scholar] [CrossRef]
- Beisecker, A.E. The influence of a companion on the doctor-elderly patient interaction. Health Commun. 1989, 1, 55–70. [Google Scholar] [CrossRef]
- Dalton, J. Client–caregiver–nurse coalition formation in decision-making situations during home visits. J. Adv. Nurs. 2005, 53, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Glasser, M.; Miller, B. Caregiver and physician perspectives of medical encounters involving dementia patients. Am. J. Alzheimer’s Dis. Other Dement. 1998, 13, 70–80. [Google Scholar] [CrossRef]
- Werner, P.; Gafni, A.; Kitai, E. Examining physician-patient-caregiver encounters: The case of Alzheimer’s disease patients and family physicians in Israel. Aging Ment. Health 2004, 8, 498–504. [Google Scholar] [CrossRef]
- Arlt, S.; Hornung, J.; Eichenlaub, M.; Jahn, H.; Bullinger, M.; Petersen, C. The patient with dementia, the caregiver and the doctor: Cognition, depression and quality of life from three perspectives. Geriatr. Psychiatry 2008, 23, 604–610. [Google Scholar] [CrossRef]
- Bogardus, S.T.; Bradley, E.H.; Williams, C.S.; Maciejewski, P.K.; Gallo, W.T.; Inouye, S.K. Achieving goals in geriatric assessment: Role of caregiver agreement and adherence to recommendations. J. Am. Geriatr. Soc. 2004, 52, 99–105. [Google Scholar] [CrossRef]
- Morgan, D.L.; Zhao, P.Z. The doctor-caregiver relationship: Managing the care of family members with Alzheimer’s disease. Qual. Health Res. 1993, 3, 133–164. [Google Scholar] [CrossRef]
- Jones, C.D.; Jones, J.; Bowles, K.H.; Schroeder, S.; Masoudi, F.A.; Coleman, E.A.; Falvey, J.; Levy, C.R.; Boxer, R.S. Patient, caregiver, and clinician perspectives on expectations for home healthcare after discharge: A qualitative case study. J. Hosp. Med. 2019, 14, 90–95. [Google Scholar] [CrossRef]
- Parmar, J.; Anderson, S.; Duggleby, W.; Holroyd-Leduc, J.; Pollard, C.; Brémault-Phillips, S. Developing person-centred care competencies for the healthcare workforce to support family caregivers: Caregiver centred care. Health Soc. Care Community 2021, 29, 1327–1338. [Google Scholar] [CrossRef]
- Fields, B.; Rodakowski, J.; James, A.E.; Beach, S. Caregiver health literacy predicting healthcare communication and system navigation difficulty. Fam. Syst. Health 2018, 36, 482–492. [Google Scholar] [CrossRef]
- Reblin, M.; Clayton, M.F.; Xu, J.; Hulett, J.M.; Latimer, S.; Donaldson, G.W.; Ellington, L. Caregiver, patient, and nurse visit communication patterns in cancer home hospice. Psycho-Oncology 2017, 26, 2285–2293. [Google Scholar] [CrossRef]
- Shin, D.W.; Cho, J.; Kim, S.Y.; Yang, H.K.; Park, K.; Kweon, S.S.; Koh, D.H.; Nam, H.S.; Park, J.H. Patients’ and family caregivers’ understanding of the cancer stage, treatment goal, and chance of cure: A study with patient-caregiver-physician triad. Psycho-Oncology 2018, 27, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Pozzar, R.; Baldwin, L.M.; Goff, B.A.; Berry, D.L. Patient, physician, and caregiver perspectives on ovarian cancer treatment decision making: Lessons from a qualitative pilot study. Pilot Feasibility Stud. 2018, 4, 91. [Google Scholar] [CrossRef] [PubMed]
- Fried, T.R.; Bradley, E.H.; O’Leary, J. Prognosis communication in serious illness: Perceptions of older patients, caregivers, and clinicians. J. Am. Geriatr. Soc. 2003, 51, 1398–1403. [Google Scholar] [CrossRef]
- Raj, M.; Platt, J.E.; Anthony, D.; Fitzgerald, J.T.; Lee, S.Y.D. What does “patient-centered” mean? Qualitative perspectives from older adults and family caregivers. Gerontol. Geriatr. Med. 2021, 7, 23337214211017608. [Google Scholar] [CrossRef]
- Lee, J.K.; Slack, M.K.; Martin, J.; Ehrman, C.; Chisholm-Burns, M. Geriatric patient care by U.S. pharmacists in healthcare teams: Systematic review and meta-analyses. J. Am. Geriatr. Soc. 2013, 61, 1119–1127. [Google Scholar] [CrossRef]
- Odegard, P.S.; Breslow, R.M.; Koronkowski, M.J.; Williams, B.R.; Hudgins, G.A. Geriatric pharmacy education: A strategic plan for the future. Am. J. Pharm. Educ. 2007, 71, 47. [Google Scholar] [CrossRef] [PubMed]
- Bardach, S.H.; Rowles, G.D. Geriatric education in the health professions: Are we making progress? Gerontologist 2012, 52, 607–618. [Google Scholar] [CrossRef]
- Roller, R.E.; Petermans, J. Education and training in geriatrics in the 21st century—Where do we come from—Where do we go? Eur. Geriatr. Med. 2015, 6, 205–257. [Google Scholar] [CrossRef]
- Razak, P.A.; Richard, K.M.; Thankachan, R.P.; Hafiz, K.A.; Kumar, K.N.; Sameer, K.M. Geriatric oral health: A review article. J. Int. Oral Health 2014, 6, 110–116. [Google Scholar]
- Kennedy, G.J.; Castro, J.; Chang, M.; Chauhan-James, J.; Fishman, M. Psychiatric and medical comorbidity in the primary care geriatric patient—An update. Curr. Psychiatry Rep. 2016, 18, 62. [Google Scholar] [CrossRef]
- Moye, J.; Harris, G.; Kube, E.; Hicken, B.; Adjognon, O.; Shay, K.; Sullivan, J.L. Mental health integration in geriatric patient-aligned care teams in the department of veterans affairs. Am. J. Geriatr. Psychiatry 2019, 27, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Elsawy, B.; Higgins, K.E. The geriatric assessment. Am. Fam. Physician 2011, 83, 48–56. [Google Scholar] [PubMed]
- Tatum, P.E.; Talebreza, S.; Ross, J.S. Geriatric assessment: An office-based approach. Am. Fam. Physician 2018, 97, 776–784. [Google Scholar]
- Tran, H.P.T.; Leonard, S.D. Geriatric assessment for primary care providers. Prim. Care Clin. Off. Pract. 2017, 44, 399–411. [Google Scholar] [CrossRef]
- Perry, W.; Lacritz, L.; Roebuck-Spencer, T.; Silver, C.; Denney, R.L.; Meyers, J.; McConnel, C.E.; Pliskin, N.; Adler, D.; Alban, C.; et al. Population health solutions for assessing cognitive impairment in geriatric patients. Innov. Aging 2018, 2, igy025. [Google Scholar] [CrossRef]
- Petrovic, M.; Somers, A.; Onder, G. Optimization of geriatric pharmacotherapy: Role of multifaceted cooperation in the hospital setting. Drugs Aging 2016, 33, 179–188. [Google Scholar] [CrossRef]
- Juul, D.; Colenda, C.C.; Lyness, J.M.; Dunn, L.B.; Hargrave, R.; Faulkner, L.R. Subspecialty training and certification in geriatric psychiatry: A 25-year overview. Am. J. Geriatr. Psychiatry 2017, 25, 445–453. [Google Scholar] [CrossRef]
- Meiboom, A.A.; de Vries, H.; Hertogh, C.M.P.M.; Scheele, F. Why medical students do not choose a career in geriatrics: A systematic review. BMC Med. Educ. 2015, 15, 101. [Google Scholar] [CrossRef]
- Denton, G.D.; Rodriguez, R.; Hemmer, P.A.; Harder, J.; Short, P.; Hanson, J.L. A prospective controlled trial of the influence of a geriatrics home visit program on medical student knowledge, skills, and attitudes towards care of the elderly. J. Gen. Intern. Med. 2009, 24, 599–605. [Google Scholar] [CrossRef]
- Camp, M.E.; Jeon-Slaughter, H.; Johnson, A.E.; Sadler, J.Z. Medical student reflections on geriatrics: Moral distress, empathy, ethics and end of life. Gerontol. Geriatr. Educ. 2018, 39, 235–248. [Google Scholar] [CrossRef]
- O’Donnell, L.; Carson, L.; Forciea, M.A.; Kinosian, B.; Shea, J.; Yudin, J.; Miller, R.K. What students experienced: A narrative analysis of essays written by first-year medical students participating in a geriatrics home visit. J. Am. Geriatr. Soc. 2013, 61, 1592–1597. [Google Scholar] [CrossRef]
- Adelman, R.D.; Capello, C.F.; LoFaso, V.; Greene, M.G.; Konopasek, L.; Marzuk, P.M. Introduction to the older patient: A “first exposure” to geriatrics for medical students. J. Am. Geriatr. Soc. 2007, 55, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- Alford, C.L.; Miles, T.; Palmer, R.; Espino, D. An introduction to geriatrics for first-year medical students. J. Am. Geriatr. Soc. 2001, 49, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Lucchetti, A.L.G.; Lucchetti, G.; de Oliveira, I.N.; Moreira-Almeida, A.; da Silva Ezequiel, O. Experiencing aging or demystifying myths?—Impact of different “geriatrics and gerontology” teaching strategies in first year medical students. BMC Med. Educ. Vol. 2017, 17, 35. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Russell, M.L.; Carr, A.H.; Kieran, K. Using mind mapping in family meetings to support shared decision making with pediatric and geriatric patients. Patient 2020, 13, 709–717. [Google Scholar] [CrossRef]
- Shapiro, J.; Cho, B. Medical readers’ theater: Relevance to geriatrics medical education. Gerontol. Geriatr. Educ. 2011, 32, 350–366. [Google Scholar] [CrossRef][Green Version]
- Tullo, E.S.; Spencer, J.; Allan, L. Systematic review: Helping the young to understand the old. Teaching interventions in geriatrics to improve the knowledge, skills, and attitudes of undergraduate medical students. J. Am. Geriatr. Soc. 2010, 58, 1987–1993. [Google Scholar] [CrossRef]
- Simms, L.J.; Zelazny, K.; Williams, T.F.; Bernstein, L. Does the number of response options matter? Psychometric properties using personality questionnaire data. Psychol. Assess. 2019, 31, 557–566. [Google Scholar] [CrossRef]
- Hubal, R.; Pina, J. Serious assessments in serious games. Int. J. Gaming Comput.-Mediat. Simul. 2012, 4, 49–64. [Google Scholar] [CrossRef]
- Wittenberg, Y.; Kwekkeboom, R.; Staaks, J.; Verhoeff, A.; de Boer, A. Informal caregivers’ views on the division of responsibilities between themselves and professionals: A scoping review. Health Soc. Care 2018, 26, e460–e473. [Google Scholar] [CrossRef]
- Flanigan, T.S.; McFarlane, E.; Cook, S. Conducting survey research among physicians and other medical professionals—A review of current literature. In Proceedings of the American Association for Public Opinion Research Annual Conference, Section on Survey Research Methods, New Orleans, LA, USA, 15–18 May 2008; Volume 63, pp. 4136–4147. [Google Scholar]
- Forsythe, L.P.; Frank, L.B.; Workman, T.A.; Hilliard, T.; Harwell, D.; Fayish, L. Patient, caregiver and clinician views on engagement in comparative effectiveness research. J. Comp. Eff. Res. 2017, 6, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.; Clarebout, G.; Diemers, A.; Delvaux, N.; Verburgh, A.; Aertgeerts, B.; Roex, A. Enhancing the connection between the classroom and the clinical workplace: A systematic review. Perspect. Med. Educ. 2017, 6, 148–157. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).