Walking All over COVID-19: The Rapid Development of STRIDE in Your Room, an Innovative Approach to Enhance a Hospital-Based Walking Program during the Pandemic
Abstract
:1. Introduction
2. Methods and Materials
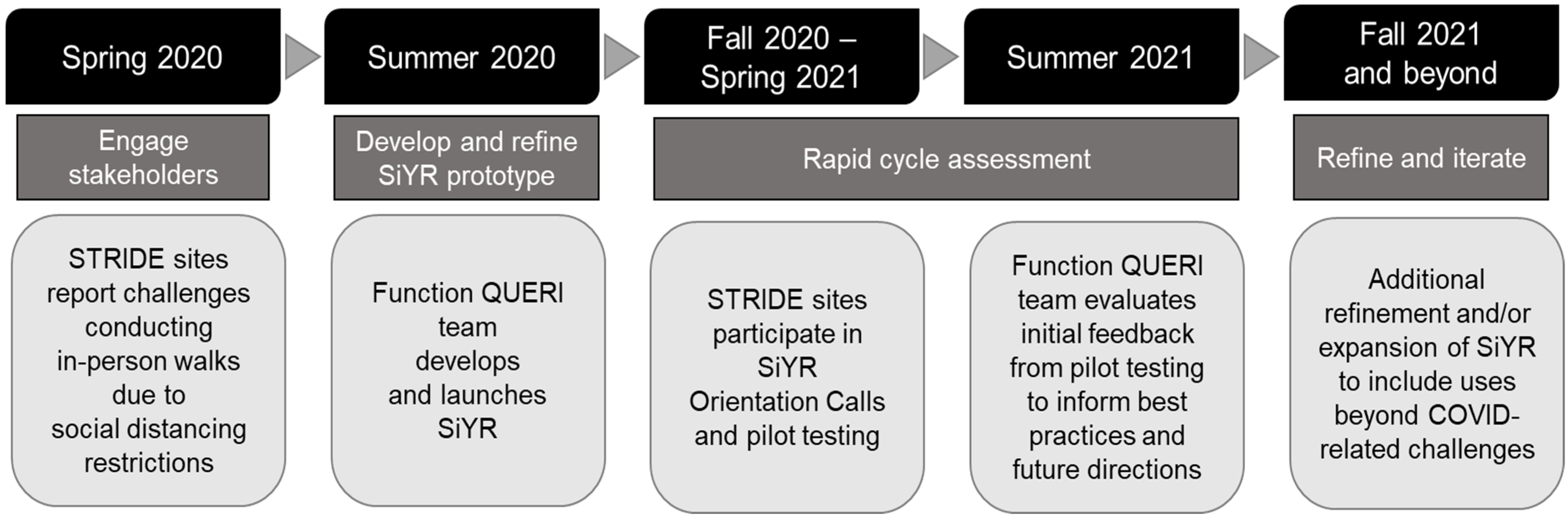
2.1. Application of Implementation Science Principles
2.2. Engage Stakeholders to Understand the Impact of the COVID-19 on Hospital-Based Mobility
2.3. Develop and Refine a Prototype
2.3.1. Responding to Stakeholder Feedback
- Social distancing requirements: At some sites, patients were instructed to remain in their rooms and STRIDE staff were prohibited from supervising face-to-face walks in the facility hallways.
- Rehabilitation support for COVID-positive patients: Patients hospitalized for COVID-19 were challenged by both respiratory symptoms of the virus and physical deconditioning.
- Supplemental tools for STRIDE: Providing patients and STRIDE teams with self-guided exercise could benefit teams during staffing shortages and/or could supplement existing walks for motivated patients who expressed an interest in additional activity.
- Support patients upon hospital discharge: At the height of the pandemic, admission to a rehabilitation and/or skilled nursing facility was complicated by a number of factors. First, some facilities had reduced capacity. Second, facilities often had extended waitlists due to requirements that potential admissions have one or more negative COVID-19 screens. Third, some patients and families preferred to be discharged home out of caution that residential and/or congregate settings may carry increased risk for COVID-19 exposure.
2.3.2. Developing and Refining the SiYR Kit
2.4. Initial Dissemination and Rapid Cycle Assessment with National STRIDE Sites
3. Results
4. Discussion
4.1. Lessons Learned
4.1.1. Dissemination and Implementation
4.1.2. Optimizing the Kit for Patient Use
4.1.3. Innovation for Rapid Translation
4.2. Future Directions: Iterative Refinement and Expansion of SiYR
4.2.1. Identify Additional Uses of SiYR Kits
4.2.2. Supplement SiYR Kit with Additional Tools to Support Self-Guided Activity
4.2.3. Partner with Other VA Program and Operations Partners
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Covinsky, K.E.; Peirluissi, E.; Johnson, C.B. Hospitalization-Associated Disability: “She Was Probably Able to Ambulate, but I’m Not Sure”. JAMA 2011, 306, 1782–1932. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.M.; Allore, H.G.; Holford, T.R.; Guo, Z. Hospitalization, Restricted Activity, and the Development of Disability among Older Persons. JAMA 2004, 292, 2115–2124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hastings, S.N.; Sloane, R.; Morey, M.C.; Pavon, J.M.; Hoenig, H. Assisted early mobility for hospitalized older veterans: Preliminary data from the STRIDE program. J. Am. Geriatr. Soc. 2014, 62, 2180–2184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hastings, S.N.; Choate, A.L.; Mahanna, E.P.; Floegel, T.A.; Allen, K.D.; Van Houtven, C.H.; Wang, V. Early Mobility in the Hospital: Lessons Learned from the STRIDE Program. Geriatrics 2018, 3, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hastings, S.N.; Stechuchak, K.M.; Choate, A.; Mahanna, E.P.; Van Houtven, C.; Allen, K.D.; Wang, V.; Sperber, N.; Zullig, L.; Bosworth, H.B.; et al. Implementation of a stepped wedge cluster randomized trial to evaluate a hospital mobility program. Trials 2020, 21, 863. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.S.; Kirchner, J. Implementation science: What is it and why should I care? Psychiatry Res. 2020, 283, 112376. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.A. Considering the intersection between implementation science and COVID-19. Implement. Res. Pract. 2020, 1. [Google Scholar] [CrossRef]
- Department of Veterans Affairs. Department of Defense Health Resources Sharing and Emergency Operations Act. Pub. L 1982, 97–174. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. Facilities Staffing Requirements for the Veterans Health Administration–Resource Planning and Methodology for the Future; National Academy of Sciences: Washington, DC, USA, 2020. [Google Scholar]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 65–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mate, K.S.; Berman, A.; Laderman, M.; Kabcenell, A.; Fulmer, T. Creating Age-Friendly Health Systems—A vision for better care of older adults. Healthcare 2018, 6, 4–6. [Google Scholar] [CrossRef] [PubMed]
| Component | Description and/or Purpose |
|---|---|
| Guided Exercises | Self-guided exercises to address weakness, injury, or illness that make it difficult to perform daily tasks. Exercises included those to target large muscle groups, balance, and stability. |
| Activity Log | Simple log to track daily activity, including minutes of walking, balance activities, strengthening exercise, and/or use of TheraBands or other light exercise equipment. |
| TheraBands | Three levels of latex-free elastic bands ranging from light to heavy strength (resistance). TheraBands can be used in place of weights for some strength exercises. |
| Stress Ball | A stress ball can help improve function for picking up items, holding on to objects, and/or performing daily tasks (e.g., eating). |
| Foam Block | The foam block can be pinched, squeezed, twisted, and moved to improve grip strength and rebuild finger and hand strength. |
| Pedometer | Pedometers, or step counters, can be helpful in setting goals and tracking daily activity. |
| Other | Tote bag, pen, STRIDE magnet, hand sanitizer |
| Domain | Question |
|---|---|
| Use | What was your main purpose of the SiYR kit? |
| Recruiting patients | How did you identify appropriate patients? What criteria did you use? |
| Introducing SiYR to patients | How did you orient patients to the SiYR kit? |
| Kit components | Which components of the kit were used most frequently? |
| Successes * | What worked well with the SiYR program? |
| Challenges * | What challenges did you have? |
| Suggestions for improvement * | What, if any, suggestions do you have to improve SiYR? |
| Documentation * | How did you document use of the kit? |
| Site | Region | Facility Complexity Level 1 | Date STRIDE Program Launched 2 | Impact(s) of COVID on STRIDE and/or Overall Facility 3 | Date SiYR Program Launched 4 | Number of SiYR Kits Requested for Distribution |
|---|---|---|---|---|---|---|
| 1 | East North Central | 1b—High complexity | Spring 2019 | STRIDE on hold | September 2020 | 9 |
| 2 | South Atlantic | 1b—High complexity | Spring 2019 | Hallways restricted | September 2020 | 9 |
| 3 | East South Central | 1b—High complexity | Winter 2018 | Reduced census | October 2020 | 9 |
| 4 | South Atlantic | 1c—High complexity | Spring 2019 | - | February 2021 | 8 |
| 5 | West North Central | 2—Medium complexity | Spring 2019 | Reduced census | February 2021 | 8 |
| 6 | East North Central | 1a—High complexity | Spring 2020 | Reduced census | February 2021 | 8 |
| 7 | West North Central | 1a—High complexity | Spring 2018 | - | February 2021 † | 8 |
| 8 | South Atlantic | 1c—High complexity | Spring 2019 | - | February 2021 | 8 |
| 9 | South Atlantic | 1a—High complexity | Winter 2019 | STRIDE on hold | March 2021 | 8 |
| 10 | West North Central | 1c—High complexity | Fall 2020 | - | May 2021 † | 10 |
| 11 | West North Central | 1c—High complexity | Fall 2020 | - | May 2021 † | 10 |
| 12 | South Atlantic | 1c—High complexity | Spring 2019 | - | June 2021 | 20 |
| 13 | West North Central | 3—Low complexity | Fall 2020 | - | June 2021 | 10 |
| Domain | Question |
|---|---|
| Use | Support COVID+ patients |
| Provide safe alternative to exercise when social distancing recommendations are in place | |
| Supplement scheduled STRIDE walks | |
| Provide additional support upon discharge | |
| Recruiting patients | Able to ambulate independently |
| Able to transfer independently | |
| Cognitively intact | |
| High motivation | |
| Patients who may use the kit upon discharge | |
| Introducing the kit to patients | Explain components of kit, demonstrate exercises |
| Kit components used most frequently | Exercise equipment (TheraBand, foam block) |
| Exercise booklet | |
| Successes | STRIDE staff and patients both appreciated the kits |
| Kits left with physical therapists (PTs) on COVID unit | |
| STRIDE PTs instructed other facility PTs on how to use SiYR kits | |
| Challenges | Some patients are too frail to exercise independently |
| Higher functioning patients may benefit from more exercises and/or more difficult exercises | |
| Pedometers were difficult for older patients (e.g., text size too small) | |
| Low patient compliance after kit was issued | |
| Exercise log may be overwhelming for some patients | |
| Suggestions for improvement | Guidance on documentation |
| Guided exercises for TheraBand and foam block | |
| More variability in exercises (i.e., option to adapt exercises to patient’s functional abilities) | |
| Documentation | Distribution of kits tracked in external spreadsheet |
| Progress note entered into patient medical record |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hughes, J.M.; Bartle, J.T.; Choate, A.L.; Mahanna, E.P.; Meyer, C.L.; Tucker, M.C.; Wang, V.; Allen, K.D.; Van Houtven, C.H.; Hastings, S.N. Walking All over COVID-19: The Rapid Development of STRIDE in Your Room, an Innovative Approach to Enhance a Hospital-Based Walking Program during the Pandemic. Geriatrics 2021, 6, 109. https://doi.org/10.3390/geriatrics6040109
Hughes JM, Bartle JT, Choate AL, Mahanna EP, Meyer CL, Tucker MC, Wang V, Allen KD, Van Houtven CH, Hastings SN. Walking All over COVID-19: The Rapid Development of STRIDE in Your Room, an Innovative Approach to Enhance a Hospital-Based Walking Program during the Pandemic. Geriatrics. 2021; 6(4):109. https://doi.org/10.3390/geriatrics6040109
Chicago/Turabian StyleHughes, Jaime M., John T. Bartle, Ashley L. Choate, Elizabeth P. Mahanna, Cassie L. Meyer, Matthew C. Tucker, Virginia Wang, Kelli D. Allen, Courtney H. Van Houtven, and Susan Nicole Hastings. 2021. "Walking All over COVID-19: The Rapid Development of STRIDE in Your Room, an Innovative Approach to Enhance a Hospital-Based Walking Program during the Pandemic" Geriatrics 6, no. 4: 109. https://doi.org/10.3390/geriatrics6040109
APA StyleHughes, J. M., Bartle, J. T., Choate, A. L., Mahanna, E. P., Meyer, C. L., Tucker, M. C., Wang, V., Allen, K. D., Van Houtven, C. H., & Hastings, S. N. (2021). Walking All over COVID-19: The Rapid Development of STRIDE in Your Room, an Innovative Approach to Enhance a Hospital-Based Walking Program during the Pandemic. Geriatrics, 6(4), 109. https://doi.org/10.3390/geriatrics6040109






