An Overview of Systematic Reviews and Meta-Analyses on Acupuncture for Post-Acute Stroke Dysphagia
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Search Strategy for Identification of SRs and Meta Analyses
2.3. Study Selection
2.4. Data Extraction and Synthesis
2.5. Quality Assessment
3. Results
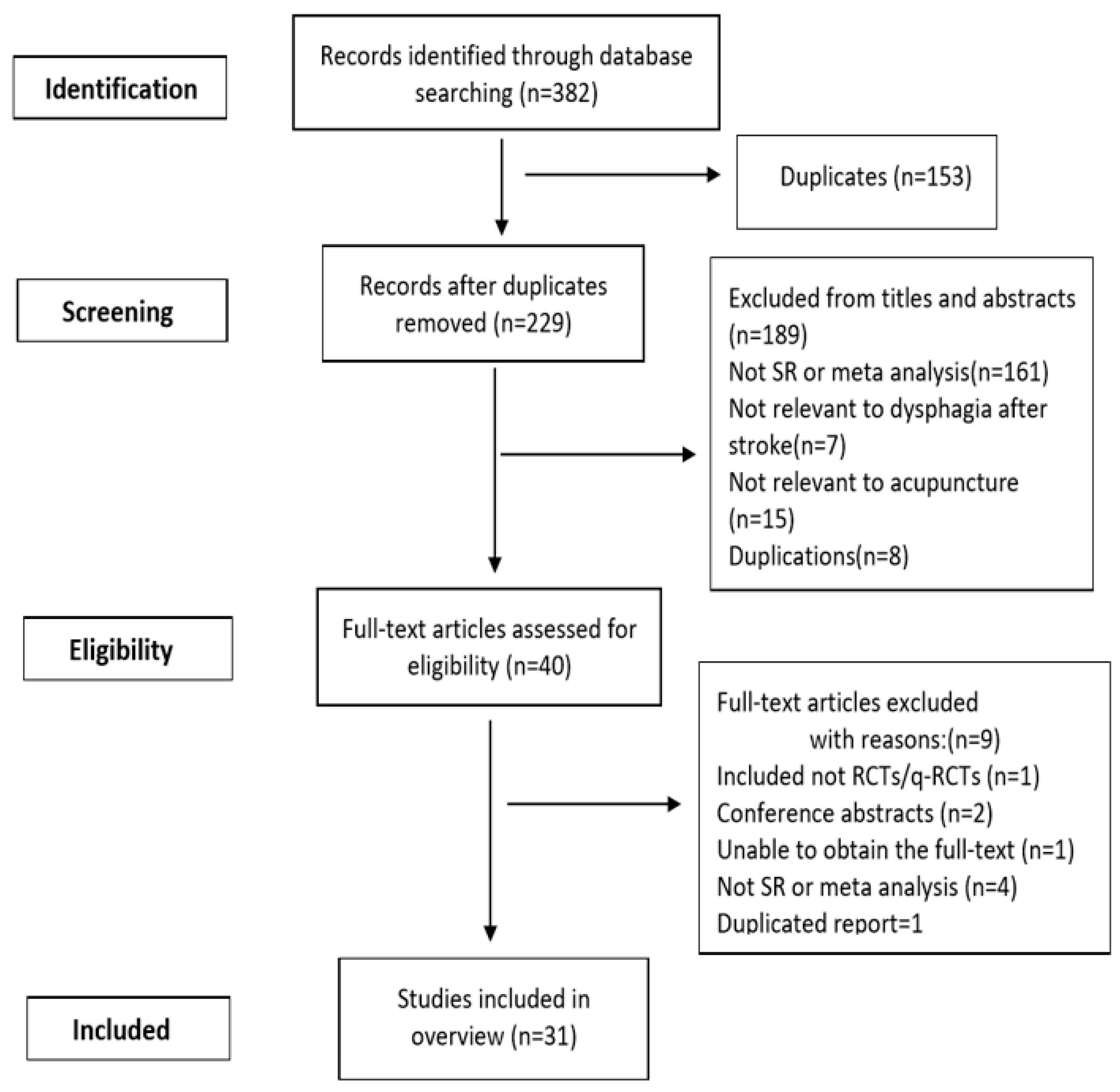
3.1. Selection of the Systematic Reviews and Meta Analyses
3.2. Characteristics of Systematic Reviews
3.3. Quality of the Systematic Reviews
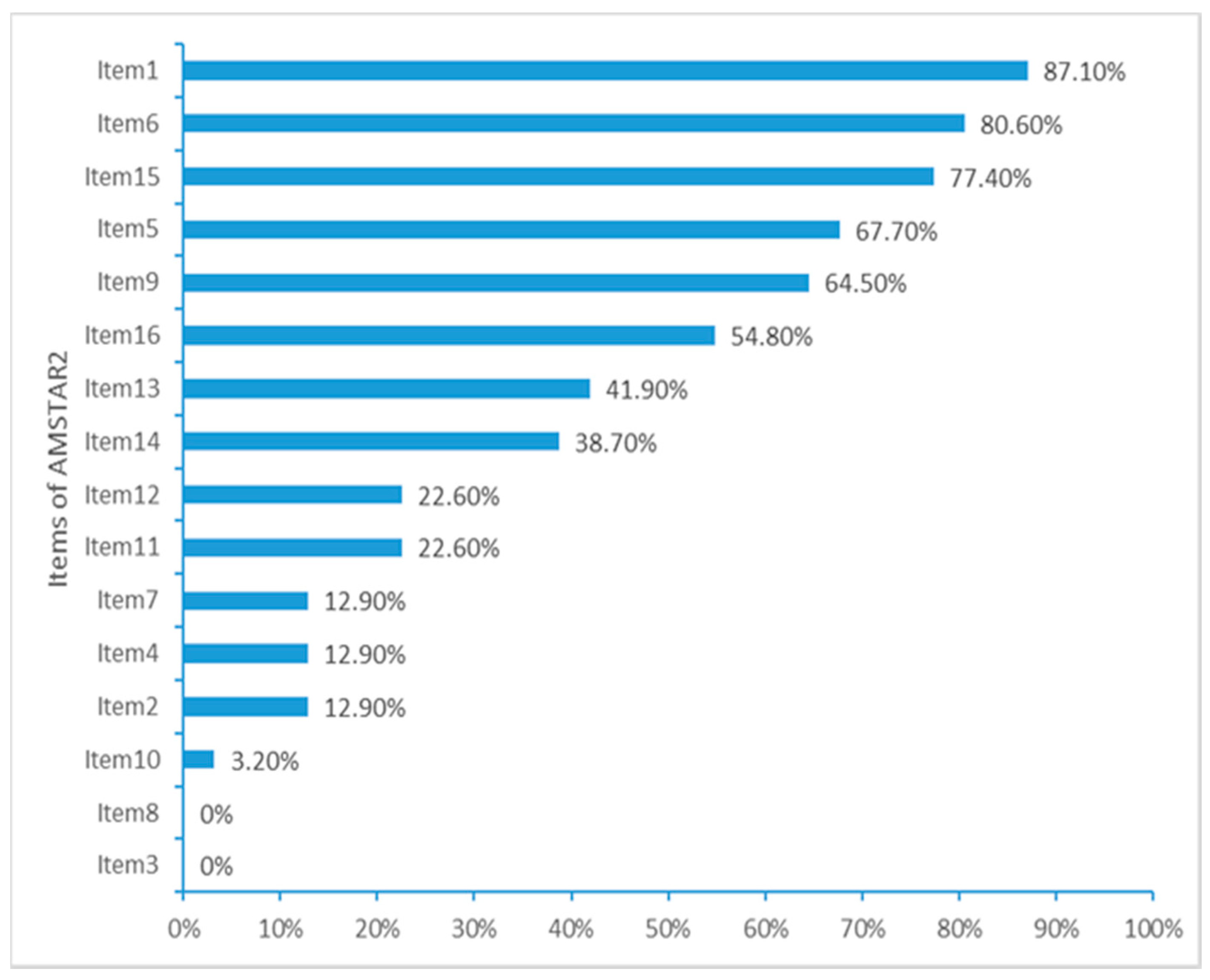
3.3.1. Methodological Quality Assessed by AMSTAR2
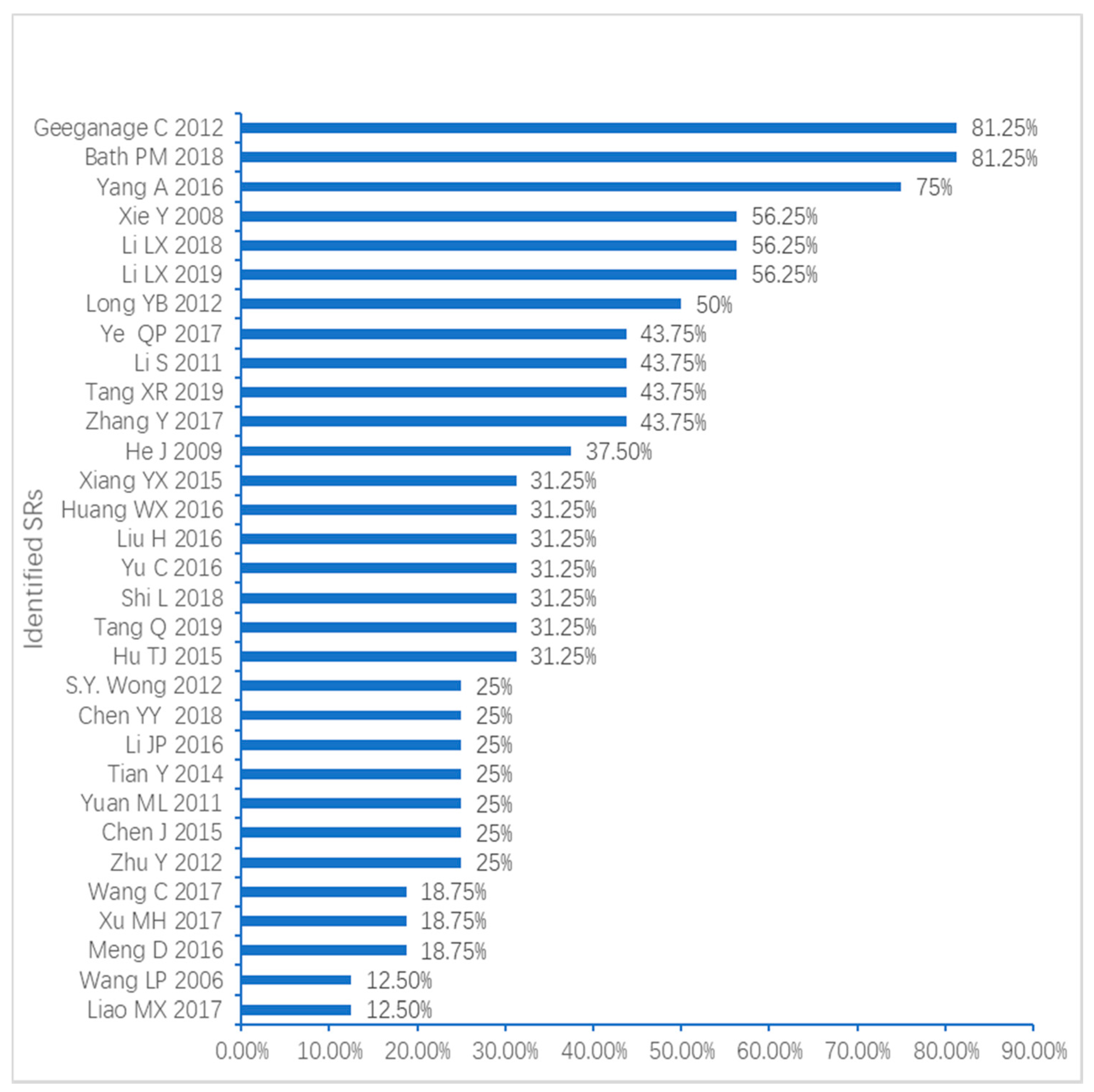
3.3.2. Reporting Quality Assessed by PRISMA
3.4. Comparison Types of Acupuncture
3.4.1. Explanatory RCTs
Acupuncture Versus No Treatment/Sham Acupuncture/Routine Acupuncture
Acupuncture Versus Rehabilitation Training/Western Medicine/Routine Therapy
3.4.2. Pragmatic RCTs
Acupuncture Plus Baseline Treatment/Medicine/Rehabilitation Training Versus Baseline Treatment/Medicine/Rehabilitation Training
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- GBD 2016 Stroke Collaborators. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar] [CrossRef]
- GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- Martino, R.; Foley, N.; Bhogal, S.; Diamant, N.; Speechley, M.; Teasell, R. Dysphagia after stroke: Incidence, diagnosis, and pulmonary complications. Stroke 2005, 36, 2756–2763. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Liesirova, K.; Broeg-Morvay, A.; Meisterernst, J.; Schlager, M.; Mono, M.L.; EI-Koussy, M.; Kagi, G.; Jung, S.; Sarikaya, H. Dysphagia in acute stroke: Incidence, burden and impact on clinical outcome. PLoS ONE 2016, 11, e0148424. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.; Bambakidis, N.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.; Hoh, B.; et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e110. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.E.; Kent, D.M.; Bulsara, K.R.; Leung, L.Y.; Lichtman, J.H.; Reeves, M.J.; Towfighi, A.; Whiteley, W.N.; Zahuranec, D.B. Effect of Dysphagia Screening Strategies on Clinical Outcomes After Stroke: A Systematic Review for the 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke. Stroke 2018, 49, e123–e128. [Google Scholar] [CrossRef] [PubMed]
- Ouyang, M.; Boaden, E.; Arima, H.; Lavados, P.M.; Billot, L.; Hackett, M.L.; Olavarria, V.V.; Munoz-Venturelli, P.; Song, K.; Rogers, K.; et al. Dysphagia screening and risks of pneumonia and adverse outcomes after acute stroke: An international multicenter study. Int. J. Stroke 2019, 21. [Google Scholar] [CrossRef]
- Yang, A.; Wu, H.M.; Tang, J.L.; Xu, L.; Yang, M.; Liu, G.J. Acupuncture for stroke rehabilitation. Cochrane Database Syst. Rev. 2016, 8. [Google Scholar] [CrossRef]
- Geeganage, C.; Beavan, J.; Ellender, S.; Bath, P.M.W. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Syst. Rev. 2012, 10, CD000323. [Google Scholar] [CrossRef]
- Bath, P.M.; Lee, H.S.; Everton, L.F. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst. Rev. 2018, 10, CD000323. [Google Scholar] [CrossRef]
- Tian, Z.-Y.; Liao, X.; Gao, Y.; Liang, S.-B.; Zhang, C.-Y.; Xu, D.-H.; Liu, J.-P.; Robinson, N. An overview of systematic reviews and meta-analyses of acupuncture for dysphagia post-acute stroke: A protocol. Eur. J. Integr. Med. 2019, 30, 100947. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Henry, D.A. AMSTAR2: A critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both. BMJ 2017. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, X.H.; Chen, Z. Meta-analysis of randomized controlled trials on electro-acupuncture in the treatment of dysphagia after Stroke. J. Clin. Acupunct. Moxibustion 2017, 33, 75–79. [Google Scholar]
- Meng, D.; Shang, Y.; Fu, Y.; Wang, X.-M.; Xu, C.-C.; Tan, Y.-X.; Tang, J.-Q.; Guo, W. Clinical Literature Study of Acupuncture and Moxibustion in the Treatment of Post stroke Dysphagia based on Meta-Analysis. Chin. Med. Mod. Distance Educ. China 2016, 14, 148–152. [Google Scholar]
- Liao, M.; Huang, L.; Zeng, F.; He, J. A meta-analysis of Jin’s three acupuncture in the treatment of pseudobulbar palsy after stroke. Li Shizhen Med. Mater. Med Res. 2017, 28, 3023–3030. [Google Scholar]
- Zhu, Y.; Fu, L.; Li, S.; Pan, W. Systematic review of acupuncture for dysphagia caused by pseudobulbar palsy after stroke. Shandong J. Tradit. Chin. Med. 2012, 31, 741–745. [Google Scholar]
- Hu, T.; Wang, X.; Yu, J.; Chen, G.; He, Y. A meta-analysis of the effect of nape acupuncture on post-acute-stroke dysphagia in domestic literature. Shanghai J. Acupunct. Moxibustion 2015, 34, 1250–1254. [Google Scholar]
- Chen, J.; Liang, W.; Liu, Q.; Qin, S.; Hei, S. Sstematic review of the efficacy and safety of acupuncture for treating dysphagia after stroke. J. Guangzhou Univ. Tradit. Chin. Med. 2015, 32, 607–614. [Google Scholar]
- He, J.; Zheng, M.; He, C.; Lan, Q.; Qu, Y.; Gao, Q.; Wang, L.; Yang, Y.; Guan, M. Systematic review of acupoint stimulating therapy for deglutition disorders after apoplexy. Chin. Acupunct. Moxibustion 2009, 29, 66–71. [Google Scholar]
- Yuan, M.; Yang, Z.; Guo, J.; Zhang, X.; Zheng, Q. A meta-analysis of the clinical effect of acupuncture combined with rehabilitation training on dysphagia after stroke. China J. Rehabil. Med. 2011, 26, 467–470. [Google Scholar]
- Tang, Q.; Zhao, X.; Zhu, L. Systematic review and meta-analysis of the effect of acupuncture combined with rehabilitation training on dysphagia after stroke. West China Med J. 2019, 34, 531–538. [Google Scholar]
- Tang, X.; Wang, L.; Huang, P.; Lan, J.; Xu, N. Meta-analysis of acupuncture combined with rehabilitation therapy for dysphagia after stroke. J. Guangzhou Univ. Tradit. Chin. Med. 2019, 36, 514–520. [Google Scholar]
- Shi, L. Acupuncture combined with rehabilitation training on treatment of post-acute-stroke dysphagia: An evidence-based medicine study. J. Clin. Acupunct. Moxibustion 2018, 34, 62–66. [Google Scholar]
- Xu, M. Meta-analysis of effect of acupuncture on dysphagia after stroke. J. Med. Sci. Yanbian Univ. 2017, 40, 113–115. [Google Scholar]
- Li, S.; Fu, L.-X.; Huang, X.-D.; Zhao, R. Systematic review of acupuncture for treatment of pseudobulbar palsy due to stroke. J. Clin. Acupunct. Moxibustion 2011, 27, 1–6. [Google Scholar]
- Wang, C.; Chai, T.; Wang, W.; Xiang, Q. The efficacy of acupuncture for post-acute-stroke dysphagia: A systematic review and meta-analysis. Guid. J. Tradit. Chin. Med. Pharm. 2017, 23, 72–76. [Google Scholar]
- Tian, Y.; Wang, J.; Song, Z.; Kang, L.; Wang, H. A meta-analysis of acupuncture combined with swallowing training on the treatment of dysphagia after stroke. Zhong Hua Zhong Yi Yao 2014, 244–249. [Google Scholar]
- Yu, C.; Shen, B.; Xu, S. Systematic review of acupuncture-moxibustion for deglutition disorders after cerebral stroke. Shanghai J. Acupunct. Moxibustion 2016, 35, 1126–1129. [Google Scholar]
- Wang, L.; Xie, Y. Systematic review on acupuncture and moxibustion for treatment of dysphagia after stroke. Chin. Acupunct. Moxibustion 2006, 2, 141–146. [Google Scholar]
- Li, J. Systematic Review of Randomized Controlled Trials of Jin’s Three Acupuncture Therapy in the Treatment of Stroke; Guangzhou University of Chinese Medicine: Guangzhou, China, 2016. [Google Scholar]
- Liu, H. Effect Evaluation of Acupuncture on Dysphagia After Apoplexy; Chengdu University of Chinese Medicine: Chengdu, China, 2016. [Google Scholar]
- Huang, W. The Literature Study and Clinical Research on Acupuncture Treatment Combined with Rehabilitation Training of Dysphagia after Stroke; Guangzhou University of Chinese Medicine: Guangzhou, China, 2016. [Google Scholar]
- Chen, Y. Meta-Analysis of Acupuncture Treatment for Dysphagia After Stroke; Changchun University of Chinese Medicine: Changchun, China, 2018. [Google Scholar]
- Xiang, Y. Acupuncture for Dysphagia After Stroke: A Systematic Review; Chengdu University of Chinese Medicine: Chengdu, China, 2015. [Google Scholar]
- Li, L.X.; Deng, K. Acupuncture combined with swallowing training for post-acute stroke dysphagia: A meta-analysis of randomized controlled trials. Acupunct. Med. 2019, 37, 81–90. [Google Scholar] [PubMed]
- Ye, Q.; Xie, Y.; Shi, J.-H.; Xu, Z.-H.; Ou, A.; Xu, N.-G. Systematic review on acupuncture for treatment of dysphagia after stroke. Evid. Based Complementary Altern. Med. 2017, 2017, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Wu, X. A meta-analysis of the efficacy of acupuncture for dysphagia after stroke. Acupunct. Med. 2012, 30, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Wong, I.S.Y.; Ng, K.F.; Tsang, H.W.H. Acupuncture for dysphagia following stroke: A systematic review. Eur. J. Integr. Med. 2012, 4, e141–e150. [Google Scholar] [CrossRef]
- Li, L.X.; Deng, K.; Qu, Y. Acupuncture treatment for post-acute-stroke dysphagia: An update meta-analysis of randomized controlled trials. Chin. J. Integr. Med. 2018, 24, 686–695. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Wang, L.; He, J.; Wu, T. Acupuncture for dysphagia in acute stroke. Cochrane Database Syst. Rev. 2008, 3, CD006076. [Google Scholar] [CrossRef]
- Xing, B.F.; Zhou, X.; Deng, X.Q. Effect of “Tongdu Tiaoshen” needling combined with swallowing training on dysphagia, cerebral blood flow and serum BDNF and NGF levels in ischemic stroke patients. Zhen Ci Yan Jiu 2019, 25, 506–511. [Google Scholar] [CrossRef]
- Becker, L.A.; Oxman, A.D. Chapter 22: Overviews of reviews. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; Higgins, J.P.T., Green, S., Eds.; The Cochrane Collaboration, 2011. Available online: http://handbook.cochrane.org/chapter_22/22_overviews_of_reviews.htm (accessed on 27 February 2015).
| SRs | Country (First Author) | No. of Primary Studies (Patients) | Age | Adverse Effects | Study Types | Intervention Measures | Primary Outcome(s) | Evidence Quality Evaluation Tool | Main Conclusions | |
|---|---|---|---|---|---|---|---|---|---|---|
| Treatment Group | Control Group | |||||||||
| 1 Zhang Y 2017 | China | 12/824 | Not mentioned | No | RCT | 1*, 2* | 3* | ER/WST | Cochrane risk of bias tool | Electro acupuncture was an effective treatment for post stroke dysphagia but still need more high quality RCTs to support this conclusion. |
| 2 Meng D 2016 | China | 48/4785 | Not Mentioned | No | RCT | 1, 2 | 3 | ER/WST/SSA | Jadad score | Both acupuncture treatment and acupuncture combined with swallowing function rehabilitation training are more effective in treating post stroke dysphagia (compared to other therapies). |
| 3 Liao MX 2017 | China | 42/3268 | Not Mentioned | No | RCT/q-RCT | 1, 2 | no limitation | ER/WST | Cochrane risk of bias tool | Jin’s three-needle alone or combined with other therapies can effectively improve the efficacy of pseudo-bulbar paralysis after stroke, but more RCTs with high-quality and large-sample size are needed. |
| 4 Zhu Y 2012 | China | 7/701 | Not Mentioned | No | RCT/q-RCT | 1, 2 | 3 | ER/SFA | Cochrane risk of bias tool + Jadad score | Acupuncture can effectively improve the efficacy of pseudo-bulbar paralysis after stroke, but more RCTs with high-quality and large-sample size are needed. |
| 5 Hu TJ 2015 | China | 17/1158 | Not Mentioned | No | RCT | 1, 2 | 3 | ER | Jadad score | Acupuncture with points on neck was an effective treatment for post stroke dysphagia but more high quality RCTs to support this conclusion is still needed. |
| 6 Chen J 2015 | China | 8/766 | 49–78yrs | No | RCT | 2 | 3 or 4* | ER | Cochrane risk of bias tool | Acupuncture combined with conventional therapy (swallowing function training, medical treatment) benefits swallowing function recovery on patients with dysphagia after stroke. The evaluation of the timing, treatment, and concurrent treatment of dysphagia after stroke still requires well designed RCTs with large-scale and high-quality. |
| 7 He J 2009 | China | 37/3697 | Not mentioned | No | RCT/q-RCT | 1 | 3 | ER | Cochrane risk of bias tool | The therapeutic effect of acupoint stimulating therapy on post stroke dysphagia is better than that the control group, but more well designed randomized, are needed to support this conclusion. |
| 8 Yuan ML 2011 | China | 13/962 | Not mentioned | No | RCT/q-RCT | 2 | 3 | ER | Jadad score | Acupuncture combined with rehabilitation training is beneficial to the recovery of swallowing function for patients with post stroke dysphagia. However, more well-designed RCTs are needed to support this conclusion. |
| 9 Tang Q 2019 | China | 22/1987 | 46–76 yrs | No | RCT | 2 | 3 or 4 | ER/VFSS/SFA/WST | Jadad score | Acupuncture combined with rehabilitation training is effective for post stroke dysphagia and the combined effect is better than rehabilitation training alone. However, due to the small size and low quality of included RCTs, well designed RCTs with large-scale and high-quality are still required. |
| 10 Tang XR 2019 | China | 16/1780 | Not mentioned | pain, ecchymosis and hematoma | RCT | 2 | 3 | ER/WST/ SSA | Cochrane risk of bias tool + Jadad score | Acupuncture combined with rehabilitation therapy was an effective treatment for post stroke dysphagia but still need more high quality RCTs to support this conclusion. |
| 11 Shi L 2018 | China | 12/1015 | 38–78yrs | No | RCT | 2 | 3 | ER/WST | Cochrane risk of bias tool | Acupuncture combined with rehabilitation training increased the efficacy and reduced the degree of dysphagia in post stroke patients but still more high quality RCTs needed to support this conclusion. |
| 12 Xu MH 2017 | China | 11/907 | Not mentioned | No | RCT | 1 | 3 | ER/ SSA | Cochrane risk of bias tool | Acupuncture therapy had better effects on post stroke dysphagia. |
| 13 Li S 2011 | China | 7/1187 | Not mentioned | No | RCT | 2 | 3 | ER | Cochrane risk of bias tool | Acupuncture therapy for pseudobulbar palsy is effective, but more high-quality RCTs are required to support this conclusion. |
| 14 Wang C 2017 | China | 32/NR | Not mentioned | No | RCT | 2 | 3 | ER | Jadad score | Acupuncture treatment for post stroke dysphagia shows better clinical efficacy. Multi-center and large-sample RCTs are still needed to support this conclusion. |
| 15 Tian Y 2014 | China | 15/1229 | Not mentioned | No | RCT | 2 | 3 | ER/WST/ VFSS | Cochrane risk of bias tool | Acupuncture combined with swallowing training has obvious effect for post stroke dysphagia. The swallowing function of patients improved more obviously than that of the control group at the same time. |
| 16 Yu C 2016 | China | 9/577 | Not mentioned | No | RCT | 1, 2 | 3 | ER/WST | Cochrane risk of bias tool | Acupuncture was efficacious in treating post stroke dysphagia, but still high-quality and large-sample-size RCTs are required to support this conclusion. |
| 17 Wang LP 2006 | China | 7/506 | Not mentioned | Subcutaneous hemorrhage at local point | RCT/q-RCT | 1, 2 | 3 | ER, VFSS, death | Cochrane risk of bias tool | A reliable conclusion cannot be drawn from the present data because of the low methodological quality, especially because of the lack of data on long-term outcomes. A tendency that acupuncture can improve dysphagia after stroke in short--term with no adverse effect id demonstrated. Therefore, it is necessary to conduct more multi-central RCTs with high quality in future. |
| 18 Li JP 2016 | China | 47/NR | Not mentioned | Mention-ed | RCT | 1, 2 | no limitation | ER/WST | Cochrane risk of bias tool | Jin’s three-needle was more effective than other therapies for post stroke dysphagia. |
| 19 Liu H 2016 | China | 14/1155 | Not mentioned | Subcutaneous hemorrhage at local point | RCT | 1, 2 | 3 | ER/WST/VFSS | Cochrane risk of bias tool | Conventional treatment plus acupuncture was more effective for some outcomes than conventional treatment alone, but RCTs with higher quality in the future may produce new evidence. |
| 20 Huang WX 2016 | China | 12/1172 | Not mentioned | Pain occurred after electro-acupuncture | RCT | 2 | 3 | ER/WST/ VFSS | Cochrane risk of bias tool | Acupuncture and moxibustion can improve the swallowing function of patients with post stroke dysphagia (better than rehabilitation training alone). |
| 21 Chen YY 2018 | China | 4/425 | Not mentioned | No | RCT/q-RCT | 1, 2 | 3 | WST | Cochrane risk of bias tool | Compared with the conventional rehabilitation treatment group, the acupuncture treatment group had better improvements for post stroke dysphagia according to the WST, but still requires high-quality and large-sample-size RCTs to support this conclusion. |
| 22 Xiang YX 2015 | China | 17/1440 | 40–85yrs | Subcutaneous hemorrhage at local point | RCT | 1, 2 | 3 | ER/WST/ SSA/VFSS | Cochrane risk of bias tool | Acupuncture combined with drugs is better than simple drugs assessed by VFSS scores. Acupuncture combined with drugs and rehabilitation training is better than drugs combined with rehabilitation assessed by SSA and VFSS scores. Acupuncture has a positive effect on improving the WST, SSA and VFSS score. However, it has not been proven that acupuncture combined with drugs and rehabilitation training can reduce the incidence of aspiration pneumonia. Acupuncture combined with rehabilitation is better than rehabilitation training alone but acupuncture and rehabilitation training have the same effect on the treatment of patients with post stroke dysphagia. However, the long-term effect of acupuncture on post stroke dysphagia is better than rehabilitation training. |
| 23 Li LX 2019 | China | 17/1479 | 27–78yrs | Mentioned | RCT | 2 | 3 | ER, SFA, IA, QOL | Cochrane risk of bias tool | Acupuncture combined with swallowing training can improve the ER, SFA and IAs of daily life in patients with post stroke dysphagia compared with swallowing training alone. However, further RCTs with large sample sizes and high quality are required to support this conclusion. |
| 24 Ye QP 2017 | China | 71/6010 | 42–82yrs | Mention-ed | RCT | 1, 2 | 3 | WST, SSA, ER | Cochrane risk of bias tool | Acupuncture was better than conventional therapies in terms of efficacy rate of post stroke dysphagia. However, further RCTs with large sample sizes and high quality are required to support this conclusion. |
| 25 Long YB 2012 | China | 72/6134 | Not mentioned | No | RCT | 2 | 3 | ER | Jadad score | Acupuncture may be beneficial in rehabilitation of patients with post stroke dysphagia. Further high-quality RCTs are still needed. |
| 26 S.Y. Wong 2012 | China (Hong Kong) | 9/783 | 40–88yrs | No | RCT | 1, 2 | 3 | SSA/VFSS/FEES | Cochrane risk of bias tool, PEDro scale | Definitive conclusions on acupuncture with conventional rehabilitation therapy for post stroke dysphagia cannot be made due to the low-quality evidence, but this combination approach appears to be promising. We recommend that acupuncture may still be used as combination use by qualified practitioners as it is relatively safe without much negative effect |
| 27 Li LX 2018 | China | 29/2190 | Not mentioned | Mention-ed | RCT | 1 | 3 | WST, KSA, FDS, VFSS, CSA | CONSORT, STRICTA | Acupuncture is an effective and safe alternative therapy for treatment to post-stroke dysphagia, although the beneficial effect from acupuncture is possibly overvalued due to the low methodology quality of the included RCTs. More high-quality and large-scale research studies are needed. |
| 28 Xie Y 2008 | China | 1/66 | No Limitation | No | RCT | 2 | 3 | Resolution of dysphagia (defined as recovery of normal feeding, which includes solid food and water, but does not include pureed food) | Cochrane risk of bias tool | There is not enough evidence to make any conclusion about the therapeutic effect of acupuncture for dysphagia after acute stroke. High quality and large scale randomized controlled trials are needed |
| 29 Yang A 2016 | China | 4/NR | 24–95 | No | RCT | 2 | 3 + 4 | Death or dependency at the end of follow-up | GRADE | From the available evidence, acupuncture may have beneficial effects on improving dependency, global neurological deficiency, and some specific neurological impairments for people with stroke in the convalescent stage, with no obvious serious adverse events. However, most included trials were of inadequate quality and size. There is, therefore, inadequate evidence to draw any conclusions about its routine use. Rigorously designed, randomized, multi-center, large sample trials of acupuncture for stroke are needed to further assess its effects. |
| 30 Bath PM 2018 | UK | 11/998 | mean 67.8 yrs | Mentioned | RCT | 1 | 4 | Death or dependency/disability | GRADE | Moderate and low-quality evidence suggests that swallowing therapy did not have a significant effect on the outcomes of death or dependency/disability, case fatality at the end of the trial, or penetration aspiration score. However, swallowing therapy may have reduced length of hospital stay, dysphagia, and chest infections, and may have improved swallowing ability. However, these results are based on evidence of variable quality, involving a variety of interventions (including acupuncture). Further high-quality trials are needed to test whether specific interventions are effective. |
| 31 Geeganage C 2012 | Sri Lanka | 4/256 | Average age of patients across the studies was 71 years | No | RCT | 1 | 4 | Death or dependency, or death or disability | Cochrane risk of bias tool | Acupuncture and behavioral therapy may reduce dysphagia, although the effective components for each remain unclear. Further research is needed to discover which components of swallowing therapy, including acupuncture, are beneficial. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tian, Z.-Y.; Liao, X.; Gao, Y.; Liang, S.-B.; Zhang, C.-Y.; Xu, D.-H.; Liu, J.-P.; Robinson, N. An Overview of Systematic Reviews and Meta-Analyses on Acupuncture for Post-Acute Stroke Dysphagia. Geriatrics 2019, 4, 68. https://doi.org/10.3390/geriatrics4040068
Tian Z-Y, Liao X, Gao Y, Liang S-B, Zhang C-Y, Xu D-H, Liu J-P, Robinson N. An Overview of Systematic Reviews and Meta-Analyses on Acupuncture for Post-Acute Stroke Dysphagia. Geriatrics. 2019; 4(4):68. https://doi.org/10.3390/geriatrics4040068
Chicago/Turabian StyleTian, Zi-Yu, Xing Liao, Ying Gao, Shi-Bing Liang, Chong-Yang Zhang, De-Hao Xu, Jian-Ping Liu, and Nicola Robinson. 2019. "An Overview of Systematic Reviews and Meta-Analyses on Acupuncture for Post-Acute Stroke Dysphagia" Geriatrics 4, no. 4: 68. https://doi.org/10.3390/geriatrics4040068
APA StyleTian, Z.-Y., Liao, X., Gao, Y., Liang, S.-B., Zhang, C.-Y., Xu, D.-H., Liu, J.-P., & Robinson, N. (2019). An Overview of Systematic Reviews and Meta-Analyses on Acupuncture for Post-Acute Stroke Dysphagia. Geriatrics, 4(4), 68. https://doi.org/10.3390/geriatrics4040068





