Geriatric Resource Teams: Equipping Primary Care Practices to Meet the Complex Care Needs of Older Adults
Abstract
:1. Introduction
2. Materials and Methods
3. Results
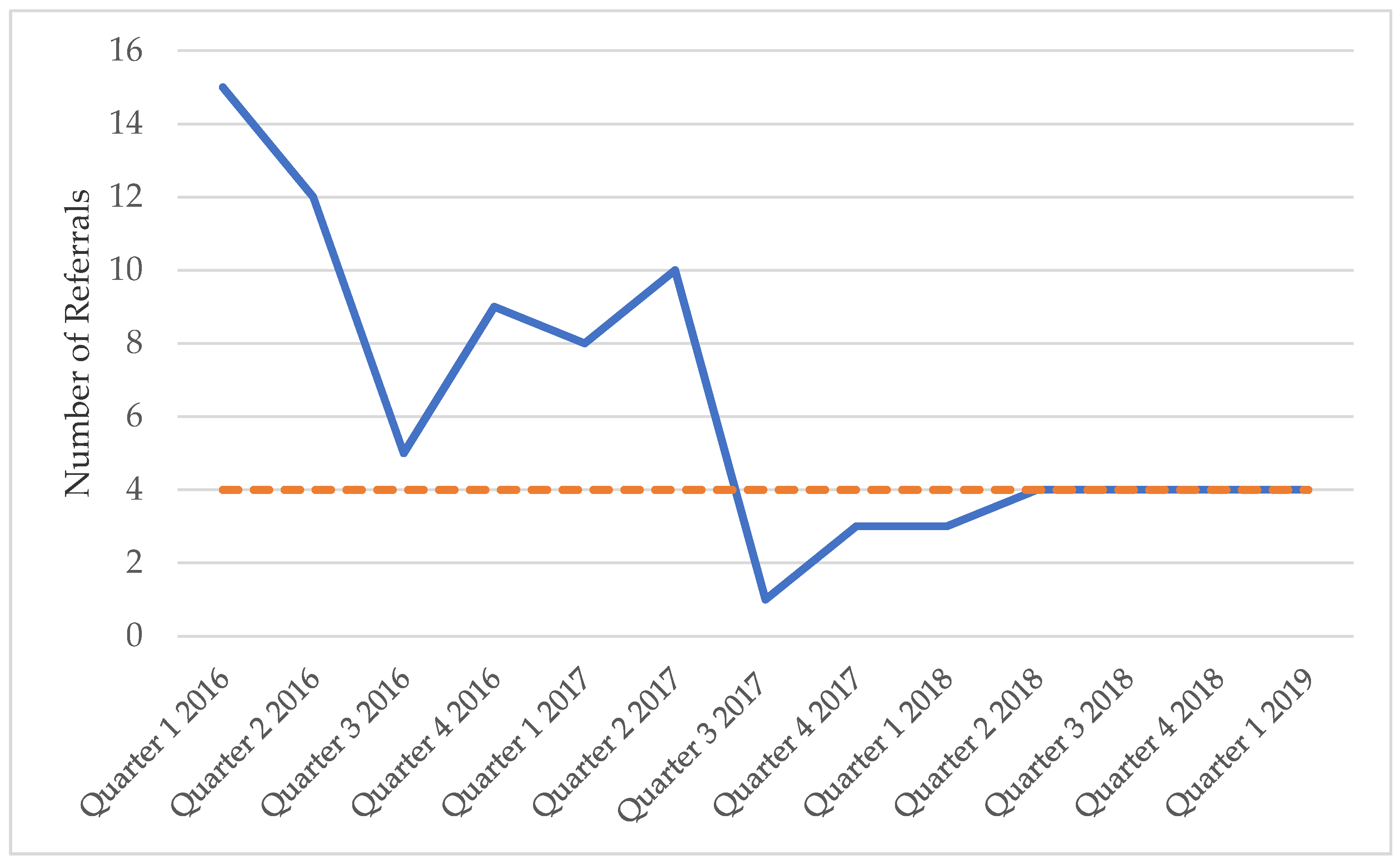
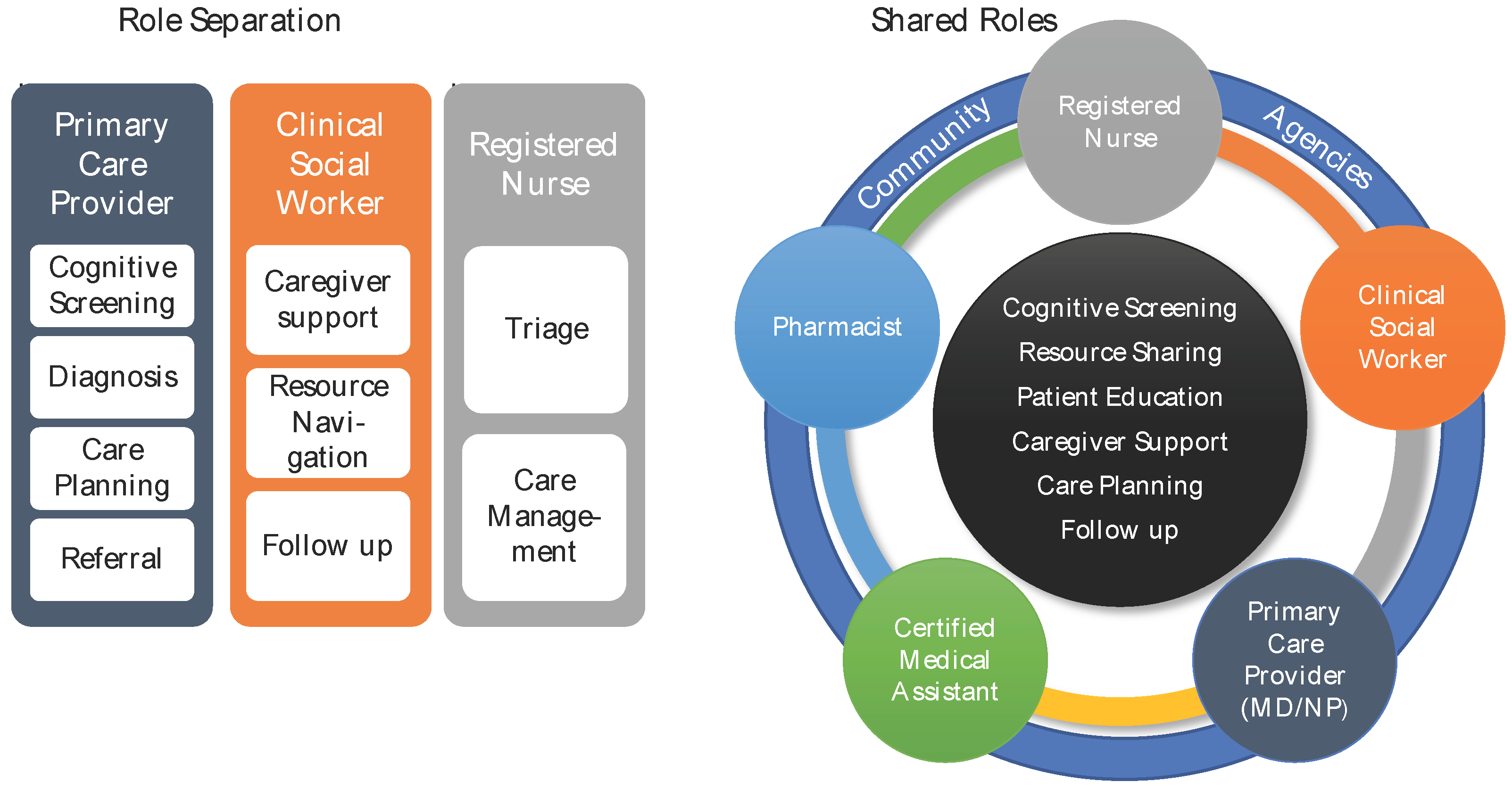
Example GRT at the Duke Outpatient Clinic (DOC)
Case Studies
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Institute of Medicine (IOM). Retooling for an Aging America: Building the Health Care Workforce; The National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- World Health Organization. Age-friendly Primary Health Care Centres Toolkit. 2008. Available online: https://www.who.int/ageing/publications/AF_PHC_Centretoolkit.pdf (accessed on 12 July 2019).
- Age-Friendly Health Systems: Guide to Using the 4Ms in the Care of Older Adults. April 2019. Available online: http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Documents/IHIAgeFriendlyHealthSystems_GuidetoUsing4MsCare.pdf (accessed on 12 July 2019).
- Alzheimer’s Association. 2019 Alzheimer’s Disease Facts and Figures. Alzheimers Dement. 2019, 15, 321–387. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Stuck, A.E.; Siu, A.L.; Wieland, D. Impacts of Geriatric Evaluation and Management Programs on defined Outcomes: Overview of the Evidence. J. Am. Geriat. Soc. 1991, 39, 8S–16S. [Google Scholar] [CrossRef] [PubMed]
- Koch, T.; Iliffe, S.; EVIDEM-ED Project. Rapid appraisal of barriers to the diagnosis and management of patients with dementia in primary care: A systematic review. BMC Fam. Pract. 2010, 11, 52. [Google Scholar] [CrossRef] [PubMed]
- Health Resources and Services Administration. Geriatric Workforce Enhancement Program. 8 November 2018. Available online: https://bhw.hrsa.gov/fundingopportunities/default.aspx?id=4c8ee9ff-617a-495e-ae78-917847db86a9 (accessed on 21 September 2019).
- Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel; Interprofessional Education Collaborative: Washington, DC, USA, 2011. [Google Scholar]
- Ogrinc, G.S.; Headrick, L.A.; Moore, S.M.; Barton, A.J.; Dolansky, M.A.; Madigosky, W.S. Fundamentals of Health Care Improvement: A Guide to Improving Your Patients’ Care, 2nd ed.; The Joint Commission and the Institute for Healthcare Improvement: Oakbrook Terrace, IL, USA, 2012. [Google Scholar]
- Borson, S.; Scanlan, J.; Brush, M.; Vitaliano, P.; Dokmak, A. The Mini-Cog: A cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int. J. Geriatr. Psychiatry 2000, 15, 1021–1027. [Google Scholar] [CrossRef]
- Razak, M.A.; Ahmad, N.A.; Chan, Y.Y.; Kasim, N.M.; Yusof, M.; Ghani, M.A.; Omar, M.; Abd Aziz, F.A.; Jamaluddin, R. Validity of screening tools for dementia and mild cognitive impairment among the elderly in primary health care: A systematic review. Public Health 2019, 169, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Frequently Asked Questions about Billing the Physician Fee Schedule for Advance Care Planning Services. July 2016. Available online: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/Downloads/FAQ-Advance-Care-Planning.pdf (accessed on 3 August 2019).
- Boustani, M.; Alder, C.A.; Solid, C.A.; Reuben, D. An Alternative Payment Model to Support Widespread Use of Collaborative Dementia Care Models. Health Aff. 2019, 38, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Hendrix, C.C.; Matters, L.; West, Y.; Stewart, B.; McConnell, E.S. The Duke-NICHE program: An academic-practice collaboration to enhance geriatric nursing care. Nurs. Outlook 2011, 59, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Giuliante, M.M.; Greenberg, S.A.; McDonald, M.V.; Squires, A.; Moore, R.; Cortes, T.A. Geriatric Interdisciplinary Team Training 2.0: A collaborative team-based approach to delivering care. J. Interprof. Care 2018, 32, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.; Stolee, P.; Boscart, V.; Giangregorio, L.; Heckman, G. Coordinating care for older adults in primary care settings: Understanding the current context. BMC Fam. Pract. 2018, 19, 137. [Google Scholar] [CrossRef] [PubMed]
- Kunik, M.E.; Mills, W.L.; Amspoker, A.B.; Cully, J.A.; Kraus-Schuman, C.; Stanley, M.; Wilson, N.L. Expanding the geriatric mental health workforce through utilization of non-licensed providers. Aging Ment. Health 2017, 21, 954–960. [Google Scholar] [CrossRef] [PubMed]

| Title | Objectives |
|---|---|
| Deprescribing |
|
| Improving Care Transitions |
|
| Improving Skilled Nursing Facility (SNF) to Home Care Transitions |
|
| Dementia: Recognition and Initial Assessment |
|
| Living with Dementia: Safety, Security, and Staying at Home |
|
| Medication Safety: Preventing Adverse Drug Events and Improving Transition of Care |
|
| Accounting for Health Literacy in Primary Care of Older Adults |
|
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buhr, G.; Dixon, C.; Dillard, J.; Nickolopoulos, E.; Bowlby, L.; Canupp, H.; Matters, L.; Konrad, T.; Previll, L.; Heflin, M.; et al. Geriatric Resource Teams: Equipping Primary Care Practices to Meet the Complex Care Needs of Older Adults. Geriatrics 2019, 4, 59. https://doi.org/10.3390/geriatrics4040059
Buhr G, Dixon C, Dillard J, Nickolopoulos E, Bowlby L, Canupp H, Matters L, Konrad T, Previll L, Heflin M, et al. Geriatric Resource Teams: Equipping Primary Care Practices to Meet the Complex Care Needs of Older Adults. Geriatrics. 2019; 4(4):59. https://doi.org/10.3390/geriatrics4040059
Chicago/Turabian StyleBuhr, Gwendolen, Carrissa Dixon, Jan Dillard, Elissa Nickolopoulos, Lynn Bowlby, Holly Canupp, Loretta Matters, Thomas Konrad, Laura Previll, Mitchell Heflin, and et al. 2019. "Geriatric Resource Teams: Equipping Primary Care Practices to Meet the Complex Care Needs of Older Adults" Geriatrics 4, no. 4: 59. https://doi.org/10.3390/geriatrics4040059





