The Preoperative Waiting Time on Long-Term Survival Following Elderly Hip Fracture Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Source
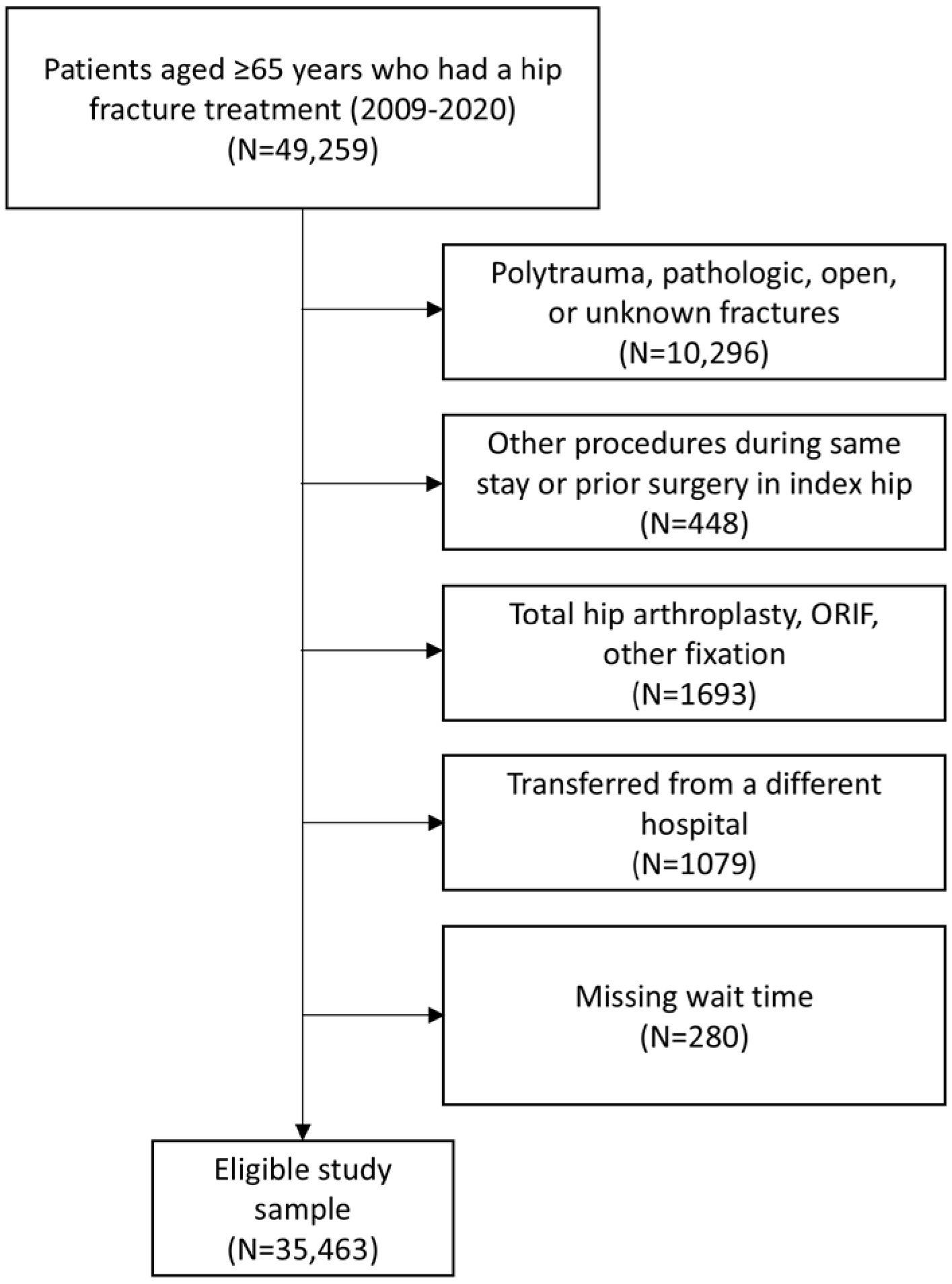
2.2. Inclusion and Exclusion Criteria
2.3. Surgical Wait Time
2.4. Outcomes of Interest
2.5. Anticoagulation Medication Before Surgery Leading to a Delay
2.6. Covariates
2.7. Statistical Analysis
2.8. Sensitivity Analysis
3. Results
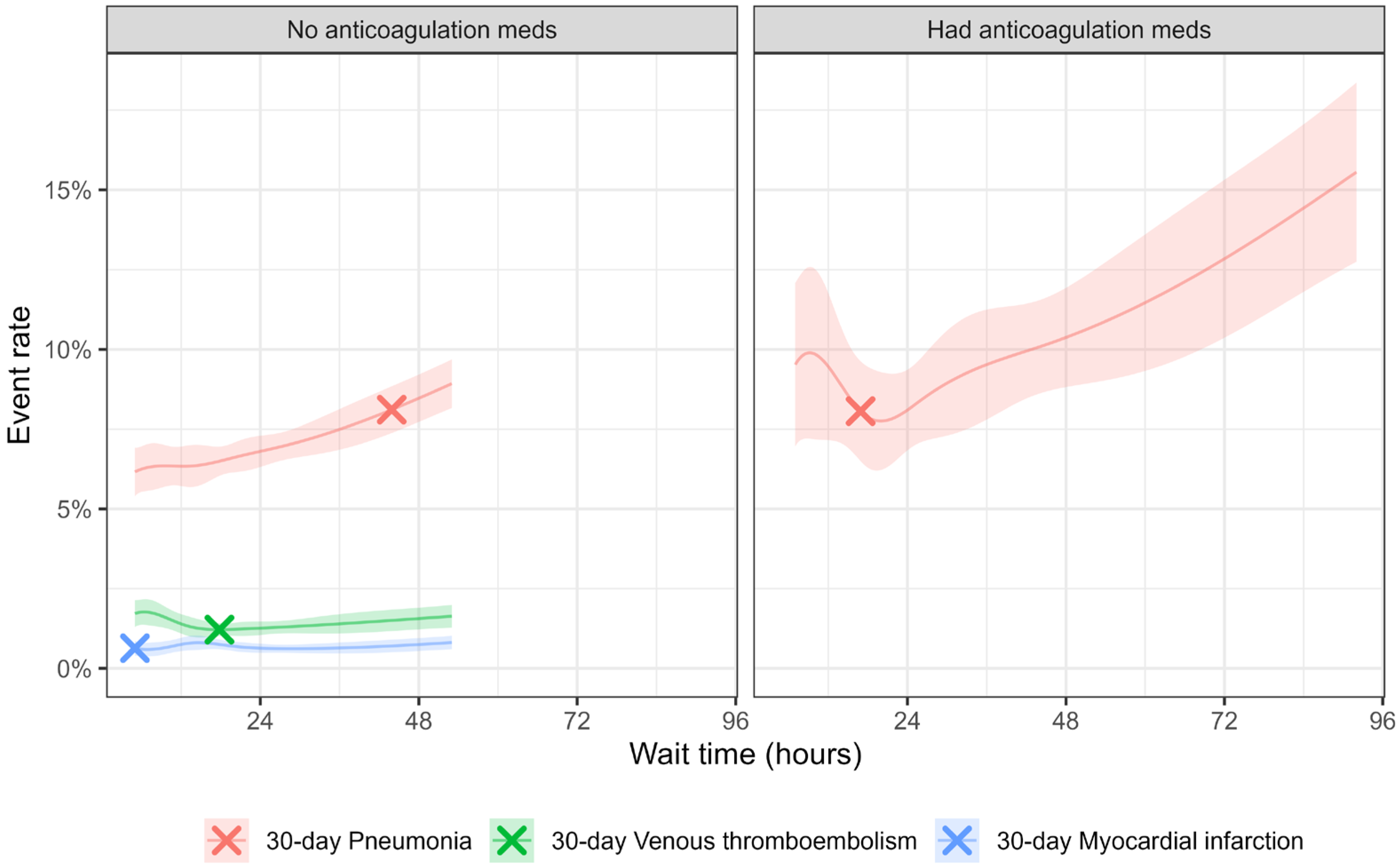
3.1. Patients Without Preoperative Anticoagulation Medications
3.2. Patients with Preoperative Anticoagulation Medications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DOAC | direct oral anticoagulation medications |
| ASA | American Surgical Association |
| OR | odds ratio |
| CI | confidence interval |
| CHF | congestive heart failure |
| BMI | body mass index |
| US | United States |
| AAOS | American Academy of Orthopedic Surgeons |
| ICD-9-CM | International Classification of Diseases, Ninth Revision, Clinical Modification |
| EHR | Electronic health record |
| COVID-19 | coronavirus disease 2019 |
| ORIF | open reduction and internal fixation |
| VTE | venous thromboembolism |
| MI | myocardial infarction |
| DVT | deep venous thrombosis |
| PE | pulmonary embolism |
| AHRQ | Agency for Healthcare Research and Quality |
References
- Cooper, C.; Campion, G.; Melton, L.J., 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef]
- Cooper, C.; Cole, Z.A.; Holroyd, C.R.; Earl, S.C.; Harvey, N.C.; Dennison, E.M.; Melton, L.J.; Cummings, S.R.; Kanis, J.A. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos. Int. 2011, 22, 1277–1288. [Google Scholar] [CrossRef]
- Morri, M.; Ambrosi, E.; Chiari, P.; Magli, A.O.; Gazineo, D.; Alessandro, F.D.; Forni, C. One-year mortality after hip fracture surgery and prognostic factors: A prospective cohort study. Sci. Rep. 2019, 9, 18718. [Google Scholar] [CrossRef] [PubMed]
- Bhatti, U.F.; Shah, A.A.; Williams, A.M.; Biesterveld, B.E.; Okafor, C.; Ilahi, O.N.; Alam, H.B. Delay in Hip Fracture Repair in the Elderly: A Missed Opportunity Towards Achieving Better Outcomes. J. Surg. Res. 2021, 266, 142–147. [Google Scholar] [CrossRef]
- Van Voorden, T.A.; Hartog, D.D.; Soesman, N.M.; Jakma, T.S.; Waleboer, M.; Staarink, M.; Bruijninckx, M.M.; Nijman, F.; Knops, S.P.; Van Lieshout, E.M.; et al. Effect of the Dutch Hip Fracture Audit implementation on mortality, length of hospital stay and time until surgery in elderly hip fracture patients; a multi-center cohort study. Injury 2020, 51, 1038–1044. [Google Scholar] [CrossRef] [PubMed]
- Viamont-Guerra, M.-R.; Guimarães, R.; Bridges, C.; Antonioli, E.; Lenza, M. Ultra-early versus early surgery for hip fracture. Cochrane Database Syst. Rev. 2024, 2024, CD015697. [Google Scholar] [CrossRef]
- O’COnnor, M.I.; Switzer, J.A. AAOS Clinical Practice Guideline Summary: Management of Hip Fractures in Older Adults. J. Am. Acad. Orthop. Surg. 2022, 30, e1291–e1296. [Google Scholar] [CrossRef] [PubMed]
- Klestil, T.; Röder, C.; Stotter, C.; Winkler, B.; Nehrer, S.; Lutz, M.; Klerings, I.; Wagner, G.; Gartlehner, G.; Nussbaumer-Streit, B. Impact of timing of surgery in elderly hip fracture patients: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 13933. [Google Scholar] [CrossRef]
- Bhandari, M.; Swiontkowski, M. Management of Acute Hip Fracture. N. Engl. J. Med. 2017, 377, 2053–2062. Available online: https://pubmed.ncbi.nlm.nih.gov/29166235/ (accessed on 2 March 2022). [CrossRef]
- Lin, H.-S.; McBride, R.L.; Hubbard, R. Frailty and anesthesia—risks during and post-surgery. Local Reg. Anesth. 2018, 11, 61–73. [Google Scholar] [CrossRef]
- Levack, A.E.M.; Moore, H.G.B.; Stephan, S.R.; Jo, S.; Schroeder, I.G.; Garlich, J.M.; Hadad, A.B.; Little, M.T.M.; Miller, A.N.; Lyman, S.; et al. Chronic Warfarin Anticoagulation in Hip Fracture Patients Delays Surgery and Is Associated With Increased Risk of Postoperative Complications: A Multicenter Propensity-Score–Matched Analysis. J. Orthop. Trauma 2023, 37, 57–63. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Jakobs, S.; Halim, N.; Seymour, H.; Tarrant, S. Synthesis of the evidence on the impact of pre-operative direct oral anticoagulants on patient health outcomes after hip fracture surgery: Rapid systematic review. Eur. J. Trauma Emerg. Surg. 2022, 48, 2567–2587. [Google Scholar] [CrossRef] [PubMed]
- You, D.; Xu, Y.; Ponich, B.; Ronksley, P.; Skeith, L.; Korley, R.; Carrier, M.; Schneider, P.S. Effect of oral anticoagulant use on surgical delay and mortality in hip fracture. Bone Jt. J. 2021, 103-B, 222–233. [Google Scholar] [CrossRef]
- Bruckbauer, M.; Prexl, O.; Voelckel, W.; Ziegler, B.; Grottke, O.; Maegele, M.; Schöchl, H. Impact of Direct Oral Anticoagulants in Patients With Hip Fractures. J. Orthop. Trauma 2019, 33, e8–e13. [Google Scholar] [CrossRef] [PubMed]
- Meinig, R.; Jarvis, S.; Orlando, A.; Nwafo, N.; Banerjee, R.; McNair, P.; Woods, B.; Harrison, P.; Nentwig, M.; Kelly, M.; et al. Is anticoagulation reversal necessary prior to surgical treatment of geriatric hip fractures? J. Clin. Orthop. Trauma 2020, 11, S93–S99. [Google Scholar] [CrossRef]
- Tang, N.; Zhang, J.; Liu, X.; Yao, D.; Zhang, X.; Ye, P.; Liu, T.; Liang, J.; Yang, W.; Armstrong, E.; et al. Effects of pre-operative continuing oral anticoagulants or antiplatelets on health outcomes among older patients with hip fracture: A systematic review and meta-analysis. Osteoporos. Int. 2025, 36, 1347–1357. [Google Scholar] [CrossRef]
- Borges, F.K.; Bhandari, M.; Guerra-Farfan, E.; Patel, A.; Sigamani, A.; Umer, M.; Tiboni, M.E.; Villar-Casares, M.d.M.; Tandon, V.; Tomas-Hernandez, J.; et al. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): An international, randomised, controlled trial. Lancet 2020, 395, 698–708. [Google Scholar] [CrossRef]
- Sarkies, M.; Testa, L.; Taylor, M.E.; Ivers, R.; Close, J.C.T.; Cameron, I.D.; Harvey, L.A. Interventions to improve hip fracture guideline adherence for time to surgery and early mobilization: A systematic review and meta-analysis. BMC Geriatr. 2025, 25, 803. [Google Scholar] [CrossRef]
- Winfield, J.; McNicoll, L.; Moppett, I.K. Epidemiology, patient outcome and complications after non-operative management of hip fracture: A systematic review. Anaesthesia 2025, 80, 1397–1413. [Google Scholar] [CrossRef]
- Inacio, M.C.S.; Weiss, J.M.; Miric, A.; Hunt, J.J.; Zohman, G.L.; Paxton, E.W. A Community-Based Hip Fracture Registry: Population, Methods, and Outcomes. Perm. J. 2015, 19, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Okike, K.; Chan, P.H.; Navarro, R.A.; Khatod, M.X.; Paxton, E.W.; Prentice, H.A. Hip Fracture Surgery Volumes Among Individuals 65 Years and Older During the COVID-19 Pandemic. JAMA 2021, 327, 387–388. [Google Scholar] [CrossRef]
- Agency for Healthcare Research and Quality. AHRQ Quality Indicators Final Report-Inpatient Quality Indicators Composite Measure Workgroup. 2008. Available online: https://qualityindicators.ahrq.gov/Downloads/Modules/IQI/AHRQ_IQI_Workgroup_Final.pdf (accessed on 10 November 2025).
- Abdel-Qadir, H.; Austin, P.C.; Pang, A.; Fang, J.; Udell, J.A.; Geerts, W.H.; McNaughton, C.D.; Jackevicius, C.A.; Kwong, J.C.; Yeh, C.H.; et al. The association between anticoagulation and adverse outcomes after a positive SARS-CoV-2 test among older outpatients: A population-based cohort study. Thromb. Res. 2021, 211, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Tanskanen, A.; Taipale, H.; Koponen, M.; Tolppanen, A.-M.; Hartikainen, S.; Ahonen, R.; Tiihonen, J. Drug exposure in register-based research—An expert-opinion based evaluation of methods. PLOS ONE 2017, 12, e0184070. [Google Scholar] [CrossRef] [PubMed]
- Harrell, F.E., Jr. Regression Modeling Strategies with Applications to Linear Models, Logistic and Ordinal Regression and Survival Analysis, 2nd ed.; Springer: New York, NY, USA, 2001. [Google Scholar]
- Davies, R.B. Hypothesis testing when a nuisance parameter is present only under the alternative. Biometrika 1987, 74, 33–43. [Google Scholar] [CrossRef] [PubMed]

| Characteristics, n (%) Unless Specified | No Anticoagulation Medication N = 30,902 | Had Anticoagulation Medication N = 4561 |
|---|---|---|
| Patient factors | ||
| Age, years. Median (IQR) Male | 83 (77–89) 9092 (29.4%) | 84 (78–88) 1620 (35.5%) |
| ASA: III/IV/V | 21,551 (74.0%) | 3794 (89.7%) |
| BMI, kg/m2 Median (IQR) Smoking status | 23.3 (20.6–26.5) | 23.7 (21.0–27.0) |
| Never | 16,264 (53.6%) | 2215 (49.0%) |
| Quit smokers | 12,110 (39.9%) | 2060 (45.6%) |
| Current smokers | 1946 (6.4%) | 246 (5.4%) |
| 90-day preop acute MI | 191 (0.6%) | 251 (5.5%) |
| Diabetes | 8583 (27.8%) | 1599 (35.1%) |
| Chronic pulmonary disease | 7718 (25.0%) | 1458 (32.0%) |
| Congestive heart failure | 5032 (16.3%) | 1640 (36.0%) |
| Hypertension | 23,941 (77.5%) | 3939 (86.4%) |
| Psychoses | 4280 (13.9%) | 827 (18.1%) |
| Renal failure | 9965 (32.3%) | 1921 (42.1%) |
| Surgical factors | ||
| Anesthesia type | ||
| General | 16,734 (54.4%) | 2895 (63.9%) |
| Neuraxial | 13,214 (42.9%) | 1509 (33.3%) |
| Converted to general | 473 (1.5%) | 59 (1.3%) |
| Monitored anesthesia care (MAC) | 216 (0.7%) | 48 (1.1%) |
| Regional only | 132 (0.4%) | 23 (0.5%) |
| Procedure | ||
| Nail fixation | 12,679 (41.0%) | 1776 (38.9%) |
| Pinning fixation | 3825 (12.4%) | 622 (13.6%) |
| Slidescrew fixation | 2392 (7.7%) | 347 (7.6%) |
| Hemi-arthroplasty | 12,006 (38.9%) | 1816 (39.8%) |
| Hospital volume | ||
| Low ≤ 125 cases/year | 8365 (27.1%) | 1300 (28.5%) |
| Medium 126–187 cases/year | 8892 (28.8%) | 1309 (28.7%) |
| High > 187 cases/year | 13,645 (44.2%) | 1952 (42.8%) |
| Surgical wait time, hours Mean ± SD Percentile: 5%, 25%, 50%, 75%, 95% | 23.8 ± 20.0 5.1, 13.2, 20.3, 27.4, 53.3 | 35.7 ± 33.3 6.9, 17.9, 26.2, 44.3, 91.7 |
| Outcome | Frequency (%) | Breakpoint Wait Time in Hours | Before Breakpoint Slope (95%CI) | After Breakpoint Slope (95%CI) |
|---|---|---|---|---|
| Patients with no pre-op anticoagulation medications (N = 30,902) | ||||
| 30 days mortality | 1500 (5.1%) | 15.5 | −0.58 (−3.38, 2.22) | 0.97 (0.30, 1.64) |
| 90 days mortality | 3309 (10.7%) | 43.4 | 1.17 (0.74, 1.61) | −2.64 (−8.03, 2.75) |
| 1 year mortality | 6428 (20.8%) | 6.1 | 8.01 (−3.67, 19.69) | 0.87 (0.57, 1.16) |
| 30 days pneumonia | 2519 (8.2%) | 43.9 | 0.69 (0.21, 1.17) | −0.47 (−7.03, 6.09) |
| 90 days VTE | 771 (2.5%) | 15.3 | −1.84 (−5.44, 1.76) | 0.44 (−0.55, 1.43) |
| 90 days MI | 506 (1.6%) | 14.3 | 2.59 (−3.35, 8.53) | −0.77 (−2.00, 0.45) |
| Patients with pre-op anticoagulation medications (N = 4561) | ||||
| 30 days mortality | 378 (8.3%) | 20.5 | −1.90 (−5.79, 1.99) | 0.50 (−0.30, 1.31) |
| 90 days mortality | 742 (16.3%) | 22.4 | −1.18 (−3.60, 1.24) | 0.50 (−0.16, 1.15) |
| 1 year mortality | 1390 (30.5%) | 28.5 | −0.55 (−1.90, 0.79) | 0.47 (−0.23, 1.18) |
| 30 days pneumonia | 449 (10.9%) | 16.9 | −1.42 (−6.51, 3.67) | 0.77 (0.13, 1.41) |
| 90 days VTE | 87 (1.9%) | 68.7 | −0.36 (−1.86, 1.14) | 7.42 (−3.31, 18.15) |
| 90 days MI | 169 (3.7%) | 16.2 | −4.70 (−14.64, 5.24) | 0.62 (−0.53, 1.78) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qiu, C.X.; Chan, P.H.; Royse, K.E.; Navarro, R.A.; Diekmann, G.R.; Yamaguchi, K.T.; Paxton, E.W.; Desai, V. The Preoperative Waiting Time on Long-Term Survival Following Elderly Hip Fracture Surgery. Geriatrics 2025, 10, 153. https://doi.org/10.3390/geriatrics10060153
Qiu CX, Chan PH, Royse KE, Navarro RA, Diekmann GR, Yamaguchi KT, Paxton EW, Desai V. The Preoperative Waiting Time on Long-Term Survival Following Elderly Hip Fracture Surgery. Geriatrics. 2025; 10(6):153. https://doi.org/10.3390/geriatrics10060153
Chicago/Turabian StyleQiu, Chunyuan X., Priscilla H. Chan, Kathryn E. Royse, Ronald A. Navarro, Glenn R. Diekmann, Kent T. Yamaguchi, Elizabeth W. Paxton, and Vimal Desai. 2025. "The Preoperative Waiting Time on Long-Term Survival Following Elderly Hip Fracture Surgery" Geriatrics 10, no. 6: 153. https://doi.org/10.3390/geriatrics10060153
APA StyleQiu, C. X., Chan, P. H., Royse, K. E., Navarro, R. A., Diekmann, G. R., Yamaguchi, K. T., Paxton, E. W., & Desai, V. (2025). The Preoperative Waiting Time on Long-Term Survival Following Elderly Hip Fracture Surgery. Geriatrics, 10(6), 153. https://doi.org/10.3390/geriatrics10060153






