Lifesaving Treatment for DISH Syndrome in the Tenth Decade of Patient’s Life
Abstract
1. Introduction
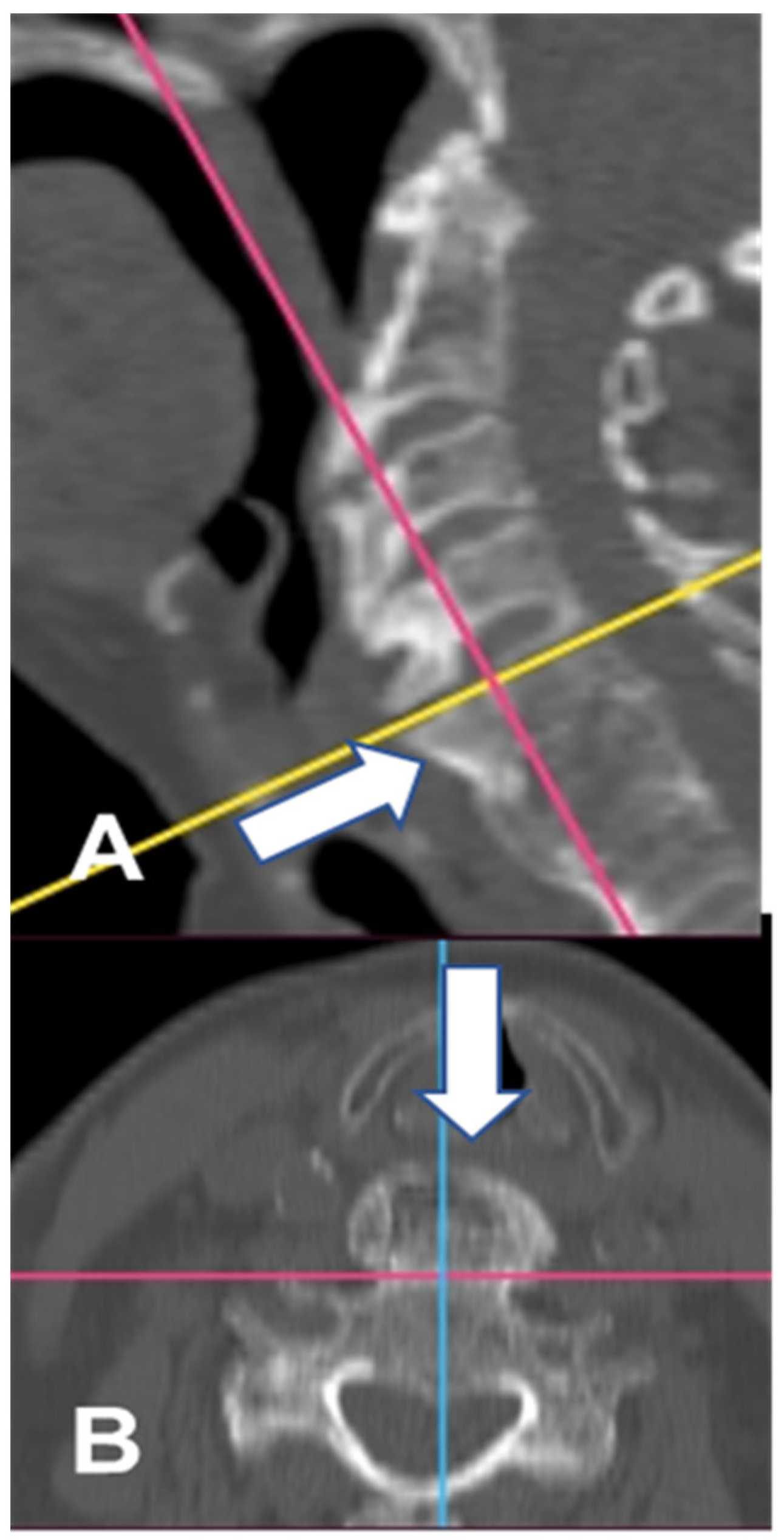
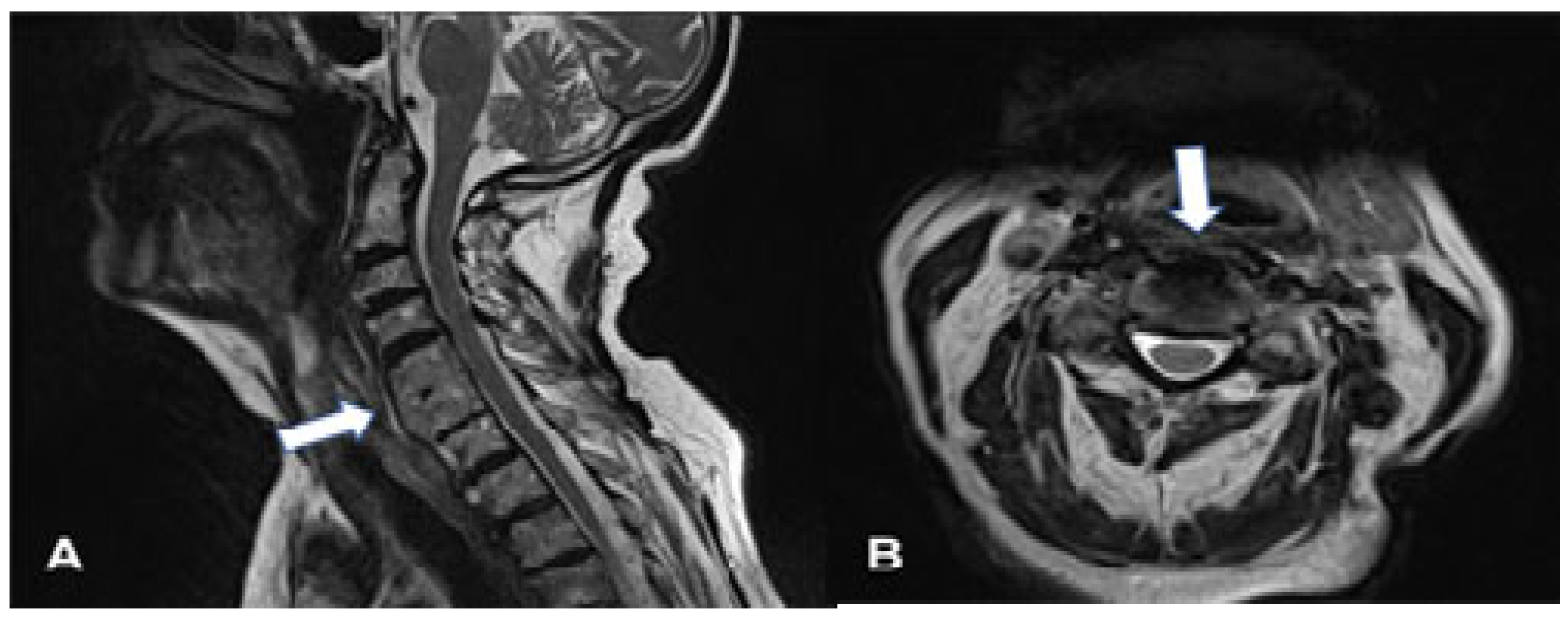
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| DISH | Diffuse idiopathic skeleton hyperostosis |
References
- Forestier, J.; Rotes-Querol, J. Senile ankylosing hyperostosis of the spine. Ann. Rheum. Dis. 1950, 9, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Belanger, T.A.; Rowe, D.E. Diffuse idiopathic skeletal hyperostosis: Musculoskeletal manifestations. J. Am. Acad. Orthop. Surg. 2001, 9, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Kmucha, S.T.; Cravens, R.B., Jr. DISHsyndrome and its role in dysphagia. Otolaryngol. Head Neck Surg. 1994, 110, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Resnick, D.; Niwayama, G. Radiographic and Pathologic Features of Spinal Involvement in Diffuse Idiopathic Skeletal Hyperostosis (DISH). Radiology 1976, 119, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Kuperus, J.S.; Hoesein, F.A.A.M.; de Jong, P.A.; Verlaan, J.J. Diffuse idiopathic skeletal hyperostosis: Etiology and clinical relevance. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101527. [Google Scholar] [PubMed]
- Mader, R.; Verlaan, J.J.; Buskila, D. Diffuse idiopathic skeletal hyperostosis: Clinical features and pathogenic mechanisms. Nat. Rev. Rheumatol. 2013, 9, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Mader, R.; Baraliakos, X.; Eshed, I.; Novofastovski, I.; Bieber, A.; Verlaan, J.J.; Kiefer, D.; Pappone, N.; Atzeni, F. Imaging of diffuse idiopathic skeletal hyperostosis (DISH). RMD Open 2020, 6, e001151. [Google Scholar] [CrossRef] [PubMed]
- Pariente-Rodrigo, E.; Sgaramella, G.A.; Olmos-Martínez, J.M.; Pini-Valdivieso, S.F.; Landeras-Alvaro, R.; Hernández-Hernández, J.L. Relationship between diffuse idiopathic skeletal hyperostosis, abdominal aortic calcification and associated metabolic disorders: Data from the Camargo Cohort. Med. Clin. 2017, 149, 196–202. [Google Scholar] [CrossRef] [PubMed]
- von der Hoeh, N.H.; Voelker, A.; Jarvers, J.S.; Gulow, J.; Heyde, C.E. Results after the surgical treatment of anterior cervical hyperostosis causing dysphagia. Eur. Spine 2015, 24 (Suppl. 4), 489–493. [Google Scholar] [CrossRef] [PubMed]
- Scholz, C.; Naseri, Y.; Hohenhaus, M.; Hubbe, U.; Klingle, J.-H. Long-term results after surgical treatment of diffuse idiopathic skeletal hyperostosis (DISH) causing dysphagia. J. Clin. Neurosci. 2019, 67, 151–155. [Google Scholar] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krolicki, B.; Mandat, V.; Mandat, T.S. Lifesaving Treatment for DISH Syndrome in the Tenth Decade of Patient’s Life. Geriatrics 2025, 10, 92. https://doi.org/10.3390/geriatrics10040092
Krolicki B, Mandat V, Mandat TS. Lifesaving Treatment for DISH Syndrome in the Tenth Decade of Patient’s Life. Geriatrics. 2025; 10(4):92. https://doi.org/10.3390/geriatrics10040092
Chicago/Turabian StyleKrolicki, Bartosz, Victor Mandat, and Tomasz S. Mandat. 2025. "Lifesaving Treatment for DISH Syndrome in the Tenth Decade of Patient’s Life" Geriatrics 10, no. 4: 92. https://doi.org/10.3390/geriatrics10040092
APA StyleKrolicki, B., Mandat, V., & Mandat, T. S. (2025). Lifesaving Treatment for DISH Syndrome in the Tenth Decade of Patient’s Life. Geriatrics, 10(4), 92. https://doi.org/10.3390/geriatrics10040092






