Research of Global Tilt and Functional Independence: Insights into Spinal Health of Older Women
Abstract
1. Introduction
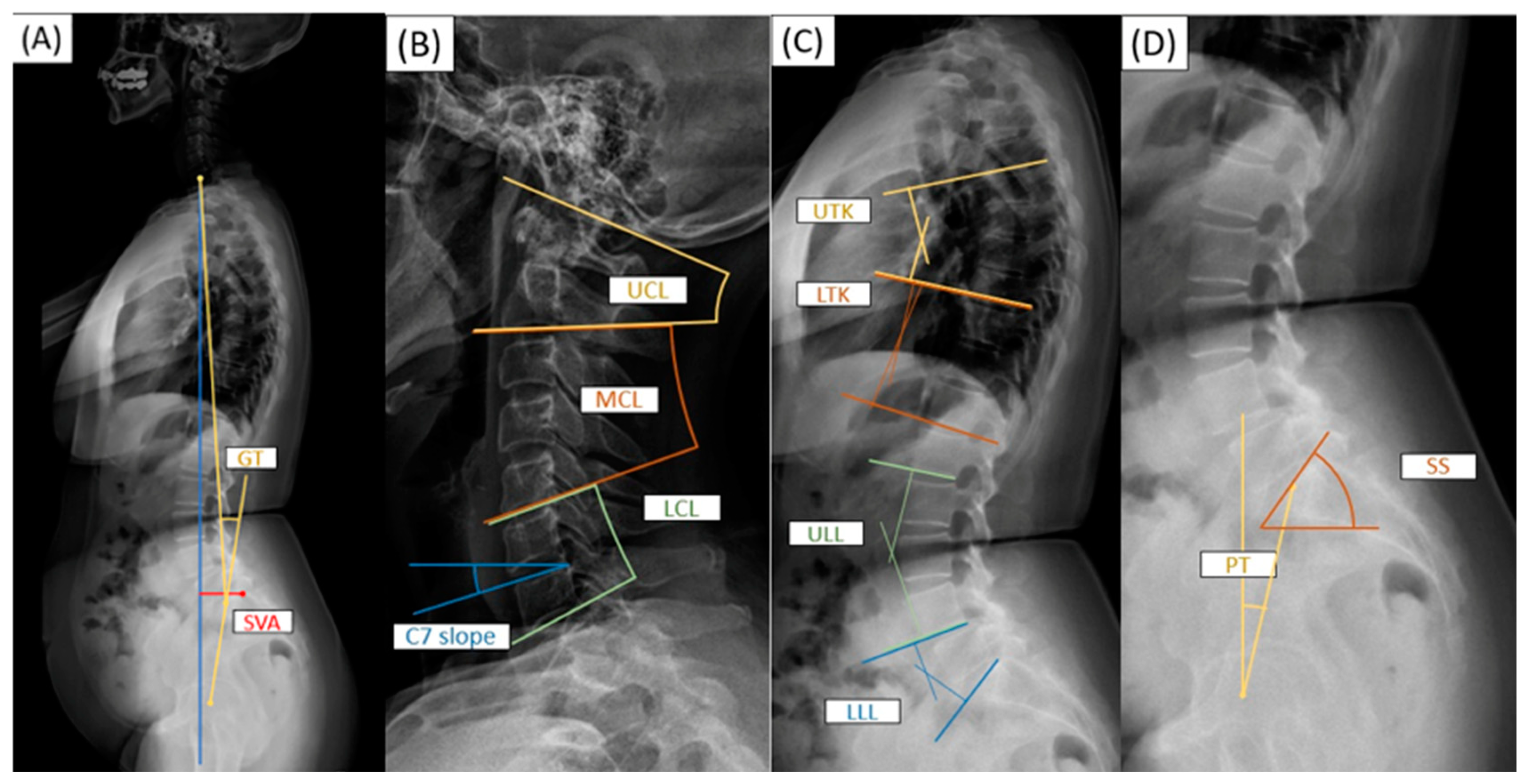
2. Materials and Methods
3. Results
3.1. Demographics of Older Females
3.2. Factors Associated with the Barthel Index
3.3. Factors Associated with GT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Le Huec, J.C.; Thompson, W.; Mohsinaly, Y.; Barrey, C.; Faundez, A. Sagittal balance of the spine. Eur. Spine J. 2019, 28, 1889–1905. [Google Scholar] [CrossRef] [PubMed]
- Sheikh Alshabab, B.; Gupta, M.C.; Lafage, R.; Bess, S.; Shaffrey, C.; Kim, H.J.; Ames, C.P.; Burton, D.C.; Smith, J.S.; Eastlack, R.K.; et al. Does Achieving Global Spinal Alignment Lead to Higher Patient Satisfaction and Lower Disability in Adult Spinal Deformity? Spine 2021, 46, 1105–1110. [Google Scholar] [CrossRef] [PubMed]
- Harroud, A.; Labelle, H.; Joncas, J.; Mac-Thiong, J.M. Global sagittal alignment and health-related quality of life in lumbosacral spondylolisthesis. Eur. Spine J. 2013, 22, 849–856. [Google Scholar] [CrossRef] [PubMed]
- Obeid, I.; Boissière, L.; Yilgor, C.; Larrieu, D.; Pellisé, F.; Alanay, A.; Acaroglu, E.; Perez-Grueso, F.J.; Kleinstück, F.; Vital, J.M.; et al. Global tilt: A single parameter incorporating spinal and pelvic sagittal parameters and least affected by patient positioning. Eur. Spine J. 2016, 25, 3644–3649. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.; Wang, G.; Li, Y.; Kuang, L.; Sun, J.; Lv, G. Predictive model of global tilt (GT) determined by individual thoracic kyphosis, lumbar lordosis and pelvic incidence in the human degenerative spine. Eur. Spine J. 2021, 30, 3191–3199. [Google Scholar] [CrossRef] [PubMed]
- Banno, T.; Togawa, D.; Arima, H.; Hasegawa, T.; Yamato, Y.; Kobayashi, S.; Yasuda, T.; Oe, S.; Hoshino, H.; Matsuyama, Y. The cohort study for the determination of reference values for spinopelvic parameters (T1 pelvic angle and global tilt) in elderly volunteers. Eur. Spine J. 2016, 25, 3687–3693. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, K.; Okamoto, M.; Hatsushikano, S.; Shimoda, H.; Ono, M.; Watanabe, K. Normative values of spino-pelvic sagittal alignment, balance, age, and health-related quality of life in a cohort of healthy adult subjects. Eur. Spine J. 2016, 25, 3675–3686. [Google Scholar] [CrossRef]
- Lee, S.H.; Hyun, S.J.; Jain, A. Cervical Sagittal Alignment: Literature Review and Future Directions. Neurospine 2020, 17, 478–496. [Google Scholar] [CrossRef]
- Hu, Z.; Man, G.C.W.; Kwok, A.K.L.; Law, S.W.; Chu, W.W.C.; Cheung, W.H.; Qiu, Y.; Cheng, J.C.Y. Global sagittal alignment in elderly patients with osteoporosis and its relationship with severity of vertebral fracture and quality of life. Arch. Osteoporos. 2018, 13, 95. [Google Scholar] [CrossRef]
- Shin, S.; Valentine, R.J.; Evans, E.M.; Sosnoff, J.J. Lower extremity muscle quality and gait variability in older adults. Age Ageing 2012, 41, 595–599. [Google Scholar] [CrossRef]
- Peters, B.R.; Sikora, Z.; Timmins, B.H.; Berli, J.U. Nerve morbidity at the radial forearm donor site following gender-affirming phalloplasty. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 3836–3844. [Google Scholar] [CrossRef] [PubMed]
- Holden, M.K.; Gill, K.M.; Magliozzi, M.R.; Nathan, J.; Piehl-Baker, L. Clinical gait assessment in the neurologically impaired. 328 Reliability and meaningfulness. Phys. Ther. 1984, 64, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Sun, Z.; Li, W.; Wang, W.; Su, T.; Du, C.; Li, W. The standing and sitting sagittal spinopelvic alignment of Chinese young and elderly population: Does age influence the differences between the two positions? Eur. Spine J. 2020, 29, 405–412. [Google Scholar] [CrossRef]
- Mi Le, J.R.; Yeh, K.T.; Chen, C.W.; Jaw, F.S.; Yang, S.H.; Wu, W.T. Quantitative evaluation of correlation between lumbosacral lordosis and pelvic incidence in standing position among asymptomatic Asian adults: A prospective study. Sci. Rep. 2022, 12, 18965. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel Index: A simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Obeid, I.; Berjano, P.; Lamartina, C.; Chopin, D.; Boissière, L.; Bourghli, A. Classification of coronal imbalance in adult scoliosis and spine deformity: A treatment-oriented guideline. Eur. Spine J. 2019, 28, 94–113. [Google Scholar] [CrossRef]
- Chen, S.W.; Wu, W.T.; Lee, R.P.; Yu, T.C.; Chen, I.H.; Wang, J.H.; Yeh, K.T. Correlations between Sagittal Parameters and Functional Scores in 65-Year-Old Osteoporotic Females with Vertebral Body Fracture under Low-Energy Mechanism. J. Clin. Med. 2024, 13, 774. [Google Scholar] [CrossRef]
- Sebaaly, A.; Silvestre, C.; Rizkallah, M.; Grobost, P.; Chevillotte, T.; Kharrat, K.; Roussouly, P. Revisiting thoracic kyphosis: A normative description of the thoracic sagittal curve in an asymptomatic population. Eur. Spine J. 2021, 30, 1184–1189. [Google Scholar] [CrossRef]
- Nori, S.; Shiraishi, T.; Aoyama, R.; Ninomiya, K.; Yamane, J.; Kitamura, K.; Ueda, S. Upper cervical lordosis compensates lower cervical kyphosis to maintain whole cervical lordosis after selective laminectomy. J. Clin. Neurosci. 2018, 58, 64–69. [Google Scholar] [CrossRef]
- Bonett, D.G.; Wright, T.A. Sample size requirements for multiple regression interval estimation. J. Organ. Behav. 2011, 32, 822–830. [Google Scholar] [CrossRef]
- Bohannon, R.W. Grip Strength: An Indispensable Biomarker for Older Adults. Clin. Interv. Aging 2019, 14, 1681–1691. [Google Scholar] [CrossRef] [PubMed]
- Glassman, S.D.; Berven, S.; Bridwell, K.; Horton, W.; Dimar, J.R. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 2005, 30, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Lafage, V.; Schwab, F.; Patel, A.; Hawkinson, N.; Farcy, J.P. Pelvic tilt and truncal inclination: Two key radiographic parameters in the setting of adults with spinal deformity. Spine 2009, 34, E599–E606. [Google Scholar] [CrossRef] [PubMed]
- Terran, J.; Schwab, F.; Shaffrey, C.I.; Smith, J.S.; Devos, P.; Ames, C.P.; Fu, K.M.; Burton, D.; Hostin, R.; Klineberg, E.; et al. The SRS-Schwab adult spinal deformity classification: Assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 2013, 73, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Bao, H.; Zhu, F.; Liu, Z.; Zhu, Z.; He, S.; Ding, Y.; Qiu, Y. Coronal curvature and spinal imbalance in degenerative lumbar scoliosis: Disc degeneration is associated. Spine 2014, 39, E1441–E1447. [Google Scholar] [CrossRef]
- Charles, Y.P.; Bauduin, E.; Pesenti, S.; Ilharreborde, B.; Prost, S.; Laouissat, F.; Riouallon, G.; Wolff, S.; Challier, V.; Obeid, I.; et al. Variation of Global Sagittal Alignment Parameters According to Gender, Pelvic Incidence, and Age. Clin. Spine Surg. 2022, 35, E610–E620. [Google Scholar] [CrossRef] [PubMed]
- Boissière, L.; Takemoto, M.; Bourghli, A.; Vital, J.M.; Pellisé, F.; Alanay, A.; Yilgor, C.; Acaroglu, E.; Perez-Grueso, F.J.; Kleinstück, F.; et al. Global tilt and lumbar lordosis index: Two parameters correlating with health-related quality of life scores-but how do they truly impact disability? Spine J. 2017, 17, 480–488. [Google Scholar] [CrossRef] [PubMed]
- Kweon, S.H.; Park, J.S.; Park, B.H. Sarcopenia and Its Association with Change of Bone Mineral Density and Functional Outcome in Old-Aged Hip Arthroplasty Patients. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221092880. [Google Scholar] [CrossRef]
- Reiss, J.; Iglseder, B.; Alzner, R.; Mayr-Pirker, B.; Pirich, C.; Kässmann, H.; Kreutzer, M.; Dovjak, P.; Reiter, R. Sarcopenia and osteoporosis are interrelated in geriatric inpatients. Z. Gerontol. Geriatr. 2019, 52, 688–693. [Google Scholar] [CrossRef]
- González Silva, Y.; Abad Manteca, L.; de la Red Gallego, H.; Álvarez Muñoz, M.; Rodríguez Carbajo, M.; Murcia Casado, T.; Ausín Pérez, L.; Abadía Otero, J.; Pérez-Castrillón, J.L. Relationship between the FRAX index and physical and cognitive functioning in older people. Ann. Med. 2018, 50, 538–543. [Google Scholar] [CrossRef]
- Norman, K.; Stobäus, N.; Gonzalez, M.C.; Schulzke, J.D.; Pirlich, M. Hand grip strength: Outcome predictor and marker of nutritional status. Clin. Nutr. 2011, 30, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Porto, J.M.; Nakaishi, A.P.M.; Cangussu-Oliveira, L.M.; Freire Júnior, R.C.; Spilla, S.B.; Abreu, D.C.C. Relationship between grip strength and global muscle strength in commu nity-dwelling older people. Arch. Gerontol. Geriatr. 2019, 82, 273–278. [Google Scholar] [CrossRef]
- Wang, Y.C.; Bohannon, R.W.; Li, X.; Sindhu, B.; Kapellusch, J. Hand-Grip Strength: Normative Reference Values and Equations for Indiv iduals 18 to 85 Years of Age Residing in the United States. J. Orthop. Sports Phys. Ther. 2018, 48, 685–693. [Google Scholar] [CrossRef]
- Inoue, H.; Hayashi, Y.; Watanabe, H.; Sawamura, H.; Shiraishi, Y.; Sugawara, R.; Kimura, A.; Masubuchi, M.; Takeshita, K. Handgrip strength is correlated with activities of daily living, balance, and body composition in patients with thoracolumbar compression fracture. Medicine 2023, 102, e33141. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.M.; Straker, L.M.; Burnett, A.F.; Wark, J.D. Chronic low back pain is associated with reduced vertebral bone mineral measures in community-dwelling adults. BMC Musculoskelet. Disord. 2012, 13, 49. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.Z.; Lee, J.H. Effect of Brace to Osteoporotic Vertebral Fracture: A Meta-Analysis. J. Korean Med. Sci. 2016, 31, 1641–1649. [Google Scholar] [CrossRef] [PubMed]
- Grazioso, S.; Selvaggio, M.; Caporaso, T.; Di Gironimo, G. A Digital Photogrammetric Method to Enhance the Fabrication of Custom-Made Spinal Orthoses. J. Prosthet. Orthot. 2019, 31, 133–139. [Google Scholar] [CrossRef]
- Weiss, H.R.; Werkmann, M. Treatment of chronic low back pain in patients with spinal deformities using a sagittal re-alignment brace. Scoliosis 2009, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Yilgor, C.; Sogunmez, N.; Boissiere, L.; Yavuz, Y.; Obeid, I.; Kleinstück, F.; Pérez-Grueso, F.J.S.; Acaroglu, E.; Haddad, S.; Mannion, A.F.; et al. Global Alignment and Proportion (GAP) Score: Development and Validation of a New Method of Analyzing Spinopelvic Alignment to Predict Mechanical Complications After Adult Spinal Deformity Surgery. J. Bone Jt. Surg. Am. 2017, 99, 1661–1672. [Google Scholar] [CrossRef]
- Noh, S.H.; Lee, H.S.; Park, G.E.; Ha, Y.; Park, J.Y.; Kuh, S.U.; Chin, D.K.; Kim, K.S.; Cho, Y.E.; Kim, S.H.; et al. Predicting Mechanical Complications After Adult Spinal Deformity Operation Using a Machine Learning Based on Modified Global Alignment and Proportion Scoring with Body Mass Index and Bone Mineral Density. Neurospine 2023, 20, 265–274. [Google Scholar] [CrossRef]
- Diebo, B.G.; Challier, V.; Shah, N.V.; Kim, D.; Murray, D.P.; Kelly, J.J.; Lafage, R.; Paulino, C.B.; Passias, P.G.; Schwab, F.J.; et al. The Dubousset Functional Test is a Novel Assessment of Physical Function and Balance. Clin. Orthop. Relat. Res. 2019, 477, 2307–2315. [Google Scholar] [CrossRef] [PubMed]
| Item | Barthel Index | |||
|---|---|---|---|---|
| ≤80 | >80 | Total | p Value | |
| n | 55 | 134 | 189 | |
| Age | 70.63 ± 8.09 | 68.90 ± 6.91 | 69.41 ± 7.29 | 0.140 |
| Postmenopausal period | 19.63 ± 7.00 | 19.56 ± 8.48 | 19.58 ± 8.06 | 0.956 |
| BMI | 23.82 ± 3.28 | 24.48 ± 3.74 | 24.28 ± 3.62 | 0.255 |
| Grip strength | 16.66 ± 4.61 | 20.01 ± 4.29 | 19.04 ± 4.63 | <0.001 * |
| Average T score | −2.10 ± 1.00 | −1.67 ± 0.65 | −1.79 ± 0.79 | 0.002 * |
| Coronal malalignment | 17 (30.9%) | 34 (25.4%) | 51 (27.0%) | 0.436 |
| Sagittal Parameters | ||||
| GT | 24.80 ± 9.16 | 19.25 ± 9.08 | 20.87 ± 9.42 | <0.001 * |
| SVA | 45.99 ± 30.44 | 33.43 ± 24.46 | 37.09 ± 26.87 | 0.003 * |
| UCL | 36.11 ± 6.13 | 36.56 ± 8.86 | 36.43 ± 8.14 | 0.734 |
| MCL | 3.48 ± 7.65 | 4.26 ± 7.20 | 4.03 ± 7.33 | 0.509 |
| LCL | 6.80 ± 7.06 | 6.47 ± 7.20 | 6.57 ± 7.14 | 0.776 |
| C7 slope | 25.61 ± 8.87 | 24.31 ± 7.71 | 24.69 ± 8.06 | 0.319 |
| UTK | −18.43 ± 6.60 | −17.99 ± 8.29 | −18.12 ± 7.82 | 0.729 |
| LTK | −5.89 ± 5.69 | −6.48 ± 7.16 | −6.31 ± 6.75 | 0.586 |
| ULL | 14.35 ± 13.54 | 16.28 ± 12.54 | 15.72 ± 12.84 | 0.349 |
| LLL | 28.15 ± 8.00 | 29.08 ± 9.86 | 28.81 ± 9.34 | 0.535 |
| SS | 30.61 ± 9.40 | 33.63 ± 9.88 | 32.75 ± 9.81 | 0.055 |
| PT | 21.92 ± 7.37 | 17.36 ± 7.29 | 18.69 ± 7.59 | <0.001 * |
| Item | Crude | Adjusted | ||
|---|---|---|---|---|
| β (95% CI) | p Value | β (95% CI) | p Value | |
| Postmenopausal period | −0.09 (−0.21, 0.03) | 0.140 | ||
| BMI | 0.17 (−0.09, 0.44) | 0.194 | ||
| Grip strength | 0.68 (0.50, 0.86) | <0.001 * | 0.53 (0.35, 0.71) | <0.001 * |
| Average T score | 2.58 (1.57, 3.60) | <0.001 * | 1.49 (0.56, 2.43) | 0.002 * |
| Global tilt angle | −0.25 (−0.35, −0.16) | <0.001 * | −0.16 (−0.25, −0.08) | <0.001 * |
| Adjusted R2 = 0.33 | ||||
| Item | Crude | Adjusted | ||
|---|---|---|---|---|
| β (95% CI) | p Value | β (95% CI) | p Value | |
| Menopause period | 0.30 (0.14, 0.46) | <0.001 * | 0.07 (−0.07, 0.21) | 0.312 |
| BMI | 0.05 (−0.32, 0.43) | 0.780 | ||
| Grip strength | −0.47 (−0.75, −0.18) | 0.002 * | −0.22 (−0.46, 0.02) | 0.076 |
| Coronal malalignment (Yes vs. No) | 5.35 (2.40, 8.31) | <0.001 * | 2.33 (0.02, 4.79) | 0.048 * |
| Average T score | −2.29 (−3.79, −0.79) | 0.003 * | −0.82 (−2.05, 0.41) | 0.190 |
| Sagittal Parameters | ||||
| SVA | 0.22 (0.18, 0.26) | <0.001 * | 0.19 (0.15, 0.24) | <0.001 * |
| UCL | 0.15 (−0.01, 0.32) | 0.073 | ||
| MCL | 0.16 (−0.03, 0.34) | 0.093 | ||
| LCL | 0.12 (−0.07, 0.31) | 0.203 | ||
| C7 slope | 0.28 (0.11, 0.44) | 0.001 * | −0.08 (−0.23, 0.07) | 0.306 |
| UTK | −0.14 (−0.31, 0.03) | 0.111 | ||
| LTK | −0.14 (−0.34, 0.07) | 0.185 | ||
| ULL | 0.06 (−0.05, 0.16) | 0.288 | ||
| LLL | −0.22 (−0.36, −0.08) | 0.003 * | −0.11 (−0.22, −0.01) | 0.043 * |
| Adjusted R2 = 0.47 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiu, Y.-C.; Tsai, P.-C.; Lee, S.-H.; Wu, W.-T.; Yu, T.-C.; Lee, R.-P.; Chen, I.-H.; Wang, J.-H.; Yeh, K.-T. Research of Global Tilt and Functional Independence: Insights into Spinal Health of Older Women. Bioengineering 2024, 11, 493. https://doi.org/10.3390/bioengineering11050493
Chiu Y-C, Tsai P-C, Lee S-H, Wu W-T, Yu T-C, Lee R-P, Chen I-H, Wang J-H, Yeh K-T. Research of Global Tilt and Functional Independence: Insights into Spinal Health of Older Women. Bioengineering. 2024; 11(5):493. https://doi.org/10.3390/bioengineering11050493
Chicago/Turabian StyleChiu, Yu-Chieh, Ping-Chiao Tsai, Ssu-Hsien Lee, Wen-Tien Wu, Tzai-Chiu Yu, Ru-Ping Lee, Ing-Ho Chen, Jen-Hung Wang, and Kuang-Ting Yeh. 2024. "Research of Global Tilt and Functional Independence: Insights into Spinal Health of Older Women" Bioengineering 11, no. 5: 493. https://doi.org/10.3390/bioengineering11050493
APA StyleChiu, Y.-C., Tsai, P.-C., Lee, S.-H., Wu, W.-T., Yu, T.-C., Lee, R.-P., Chen, I.-H., Wang, J.-H., & Yeh, K.-T. (2024). Research of Global Tilt and Functional Independence: Insights into Spinal Health of Older Women. Bioengineering, 11(5), 493. https://doi.org/10.3390/bioengineering11050493












