Upper Crossed Syndrome and Scapulae Upper-Trapping: A Mesotherapy Protocol in Cervicoscapulobrachial Pain—The 8:1 Block
Abstract
1. Introduction
2. Biomechanical and Kinesiological Considerations
3. Cervicoscapulobrachialgia: A Proposition
4. Differential Diagnoses in Cervicoscapulobrachialgia
5. Diagnostic Reasoning
6. A New Protocol: The 8:1 Block
7. Discussion and Description of the Technique
7.1. Protocol Description
7.2. Injection Sites
- Posterior Points (8):
- Cervical facets (between C1 and C4)
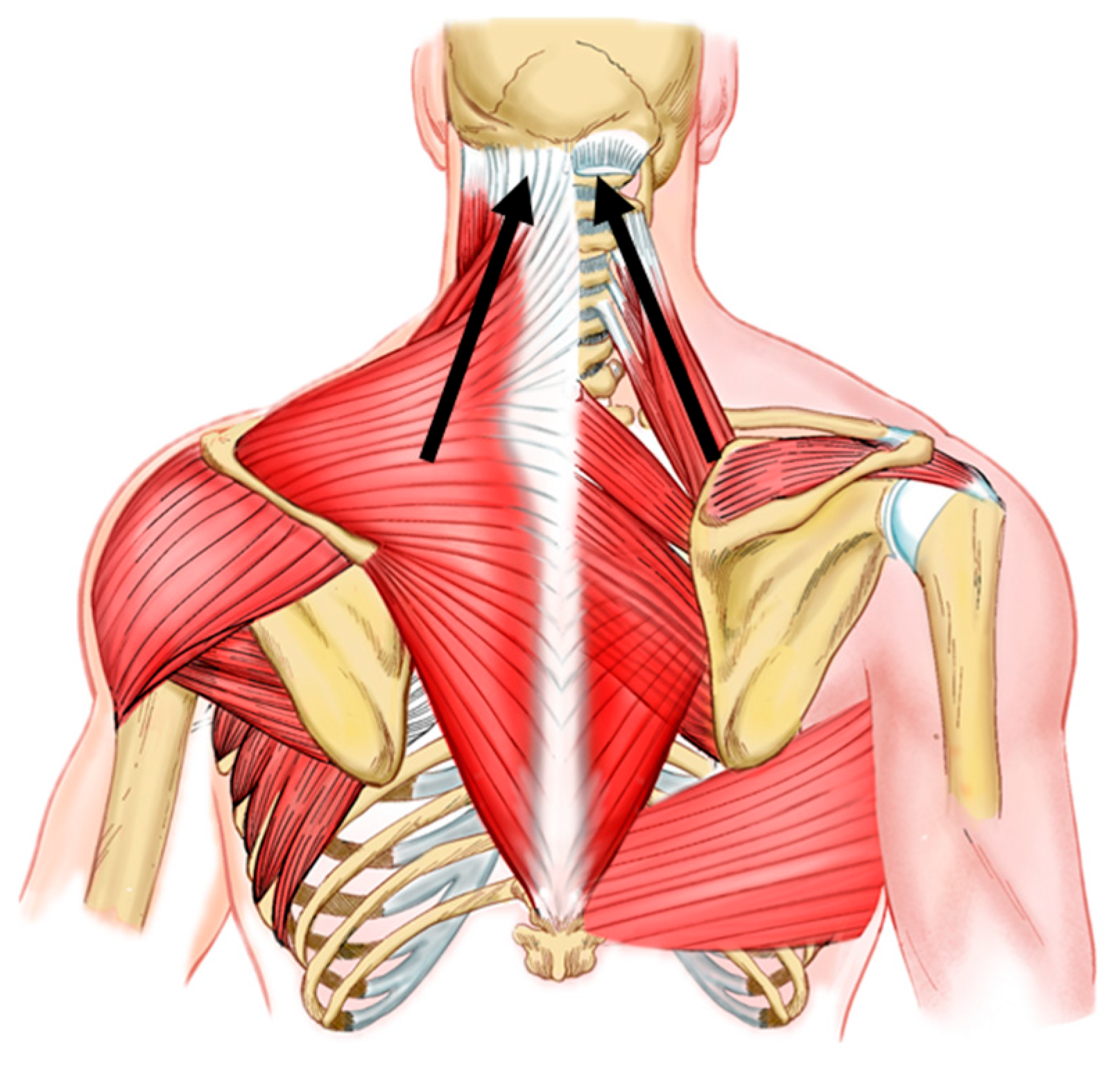
- Scapular enthesis of the levator scapulae
- Entheses of the lesser and greater rhomboids
- Supraspinatus point over the suprascapular nerve
- Three additional points between the scapular entheses and thoracic spinous processes targeting the spinal portion of the accessory nerve and dorsal scapular nerve.
- Anterior Point (1):
7.3. Dosage and Frequency
7.4. Anesthesia
8. Conclusions and Final Considerations
9. Author’s Note
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Janda, V. Janda Compendium; O.P.T.P.: Plymouth, MN, USA, 1997; Volume II, pp. 7–13. [Google Scholar]
- Stevens, G.T. The Pose of the Body as Related to the Type of the Cranium and the Direction of the Visual Plane. Buffalo Med. J. 1901, 40, 576–580. [Google Scholar] [PubMed]
- Schwartz, L. A resume, with comments, of the available literature relating to posture. Public Health Rep. 1927, 42, 1219–1224. [Google Scholar] [CrossRef]
- Sheikhhoseini, R.; Shahrbanian, S.; Sayyadi, P.; O’Sullivan, K. Effectiveness of Therapeutic Exercise on Forward Head Posture: A Systematic Review and Meta-analysis. J. Manip. Physiol. Ther. 2018, 41, 530–539. [Google Scholar] [CrossRef] [PubMed]
- Iannotti, J.P.; Parker, R.D. The Netter Collection of Medical Illustrations (Frank H. Netter, MD). Musculoskeletal System, Part 1: Upper Limb, 2nd ed.; Elsevier: Amsterdam, The Netherlands, 2013; pp. 2–3. [Google Scholar]
- Neumann, D.A. Cinesiologia do Aparelho Musculoesquelético: Fundamentos Para Reabilitação, 3rd ed.; Elsevier: Rio de Janeiro, Brazil, 2011. [Google Scholar]
- Levangie, P.K.; Norkin, C.C.; Lewek, M.D. (Eds.) Joint Structure & Function: A Comprehensive Analysis, 6th ed.; McGraw Hill: New York, NY, USA, 2019. [Google Scholar]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013, 33, 629–808. [Google Scholar] [CrossRef] [PubMed]
- Fejer, R.; Kyvik, K.O.; Hartvigsen, J. The prevalence of neck pain in the world population: A systematic critical review of the literature. Eur. Spine J. 2006, 15, 834–848. [Google Scholar] [CrossRef] [PubMed]
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman MJ, M.; Kolahi, A.A.; Safiri, S. Neck pain: Global epidemiology, trends and risk factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef] [PubMed]
- Gangavelli, R.; Nair, N.S.; Bhat, A.K.; Solomon, J.M. Cervicobrachial pain—How Often is it Neurogenic? J. Clin. Diagn. Res. 2016, 10, YC14–YC16. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.D.; Jiang, L.S.; Dai, L.Y. Degenerative cervical spondylolisthesis: A systematic review. Int. Orthop. (SICOT) 2011, 35, 869–875. [Google Scholar] [CrossRef]
- Aktaş, İ.; Ünlü Özkan, F. Pectoralis minor syndrome. Turk. J. Phys. Med. Rehabil. 2022, 68, 447–455. [Google Scholar] [CrossRef]
- Ahmed, A.S.; Graf, A.R.; Karzon, A.L.; Graulich, B.L.; Egger, A.C.; Taub, S.M.; Gottschalk, M.B.; Bowers, R.L.; Wagner, E.R. Pectoralis minor syndrome—Review of pathoanatomy, diagnosis, and management of the primary cause of neurogenic thoracic outlet syndrome. JSES Rev. Rep. Tech. 2022, 2, 469–488. [Google Scholar] [CrossRef]
- Scott, A.; Ashe, M.C. Common tendinopathies in the upper and lower extremities. Curr. Sports Med. Rep. 2006, 5, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Romero-Morales, C.; López-López, D.; Almazán-Polo, J.; Mogedano-Cruz, S.; Sosa-Reina, M.D.; García-Pérez-de-Sevilla, G.; Martín-Pérez, S.; González-de-la-Flor, Á. Prevalence, diagnosis and management of musculoskeletal disorders in elite athletes: A mini-review. Dis.-A-Mon. 2024, 70, 101629. [Google Scholar] [CrossRef] [PubMed]
- Vila, H.; Barreiro, A.; Ayán, C.; Antúnez, A.; Ferragut, C. The Most Common Handball Injuries: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10688. [Google Scholar] [CrossRef] [PubMed]
- Young, W.K.; Briner, W.; Dines, D.M. Epidemiology of Common Injuries in the Volleyball Athlete. Curr. Rev. Musculoskelet. Med. 2023, 16, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Liaghat, B.; Pedersen, J.R.; Husted, R.S.; Pedersen, L.L.; Thorborg, K.; Juhl, C.B. Diagnosis, prevention and treatment of common shoulder injuries in sport: Grading the evidence—A statement paper commissioned by the Danish Society of Sports Physical Therapy (DSSF). Br. J. Sports Med. 2023, 57, 408–416. [Google Scholar] [CrossRef]
- Hasley, I.B.; Ostby, T.D.; Fjosne, C.M.; Jelsing, E.J. Etiology and Prevention of Common Injuries in Golf. Curr. Sports Med. Rep. 2023, 22, 210–216. [Google Scholar] [CrossRef]
- Apostolakos, J.M.; Brusalis, C.M.; Uppstrom, T.; RThacher, R.; Kew, M.; Taylor, S.A. Management of Common Football-Related Injuries About the Shoulder. HSS J. 2023, 19, 339–350. [Google Scholar] [CrossRef]
- Leung, J. A Guide to Indoor Rock Climbing Injuries. Curr. Sports Med. Rep. 2023, 22, 55–60. [Google Scholar] [CrossRef]
- Russek, A.S. Diagnosis and Treatment of Scapulocostal Syndrome. JAMA J. Am. Med. Assoc. 1952, 150, 25. [Google Scholar] [CrossRef]
- Lawrence, R.L.; Braman, J.P.; Keefe, D.F.; Ludewig, P.M. The Coupled Kinematics of Scapulothoracic Upward Rotation. Phys. Ther. 2020, 100, 283–294. [Google Scholar] [CrossRef]
- Dias de Lacerda, A.P.; Rodrigues de Andrade, P.; Kamonseki, D.H.; Parizotto, N.A.; Alves da Silva, A.S.; Bernardo de Medeiros, L.; de Almeida Ferreira, J.J. Accuracy of infrared thermography in detecting tendinopathy: A systematic review with meta-analysis. Phys. Ther. Sport 2022, 58, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, S.; Fernando, R.; Screen, H.; Waugh, C.; Tucker, A.; Morrissey, D. The use of medical infrared thermography in the detection of tendinopathy: A systematic review. Phys. Ther. Rev. 2016, 21, 75–82. [Google Scholar] [CrossRef]
- dos Santos, J.B. Descrição do método de avaliação postural de Portland State University. Fisioter. Bras. 2005, 6, 392–395. [Google Scholar] [CrossRef]
- Santos, A.; Fantinati, A. Os Principais Softwares Utilizados na Biofotogrametria Computadorizada para Avaliação Postural: Uma Revisão Sistemática. Movimenta 2018, 4, 139–148. [Google Scholar]
- Souza, J.A.; Pasinato, F.; Basso, D.; Corrêa, E.C.R.; Da Silva, A.M.T. Biofotogrametria confiabilidade das medidas do protocolo do software para avaliação postural (SAPO). Rev. Bras. Cineantropometria Desempenho Hum. 2011, 13, 299–305. [Google Scholar] [CrossRef]
- Hougs Kjær, B.; Ellegaard, K.; Wieland, I.; Warming, S.; Juul-Kristensen, B. Intra-rater and inter-rater reliability of the standardized ultrasound protocol for assessing subacromial structures. Physiother. Theory Pract. 2017, 33, 398–409. [Google Scholar] [CrossRef]
- Lee, H.J.; Lee, J.H.; Yi, K.H.; Kim, H.J. Sonoanatomy and an ultrasound scanning protocol of the intramuscular innervation pattern of the infraspinatus muscle. Reg. Anesth. Pain Med. 2023, 48, 175–179. [Google Scholar] [CrossRef]
- Widholm, P.; Ahlgren, A.; Karlsson, M.; Romu, T.; Tawil, R.; Wagner, K.R.; Statland, J.M.; Wang, L.H.; Shieh, P.B.; van Engelen, B.G.M.; et al. Quantitative muscle analysis in facioscapulohumeral muscular dystrophy using whole-body fat-referenced MRI: Protocol development, multicenter feasibility, and repeatability. Muscle Nerve 2022, 66, 183–192. [Google Scholar] [CrossRef]
- Estwanik, J.J. Levator Scapulae Syndrome. Physician Sportsmed. 1989, 17, 57–68. [Google Scholar] [CrossRef]
- Behrsin, J.F.; Maguire, K. Levator scapulae action during shoulder movement: A possible mechanism for shoulder pain of cervical origin. Aust. J. Physiother. 1986, 32, 101–106. [Google Scholar] [CrossRef]
- Castelein, B.; Cools, A.; Parlevliet, T.; Cagnie, B. Are chronic neck pain, scapular dyskinesis and altered scapulothoracic muscle activity interrelated?: A case-control study with surface and fine-wire EMG. J. Electromyogr. Kinesiol. 2016, 31, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Kuzmich, D. The Levator Scapulae: Making the Con—NECK—Tion. J. Man. Manip. Ther. 1994, 2, 43–54. [Google Scholar] [CrossRef]
- Manchikanti, L.; Singh, V.; Rivera, J.; Pampati, V. Prevalence of cervical facet joint pain in chronic neck pain. Pain Physician 2002, 5, 243. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.P. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin. Proc. 2015, 90, 284–299. [Google Scholar] [CrossRef] [PubMed]
- Falco, F.; Erhart, S.; Wargo, B.W.; Bryce, D.A.; Atluri, S.; Datta, S.; Hayek, S.M. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician 2009, 12, 323. [Google Scholar] [CrossRef] [PubMed]
- Candido, K.D.; England, B. Cervical spine pain related to the facet joints. Tech. Reg. Anesth. Pain Manag. 2015, 19, 109–118. [Google Scholar] [CrossRef]
- Hodge, J. Facet, nerve root, and epidural block. Semin. Ultrasound CT MRI 2005, 26, 98–102. [Google Scholar] [CrossRef]
- Bagoji, I.B.; Hadimani, G.A.; Bulgoud, R.S.; Desai, V.; Prakash, K.G.; Bharatha, A. Anatomical Variations of the Suprascapular Notch and its Importance in Suprascapular Entrapment Neuropathy. Maedica 2020, 15, 298–304. [Google Scholar] [CrossRef]
- Leider, J.D.; Derise, O.C.; Bourdreaux, K.A.; Dierks, G.J.; Lee, C.; Varrassi, G.; Sherman, W.F.; Kaye, A.D. Treatment of suprascapular nerve entrapment syndrome. Orthop. Rev. 2021, 13, 25554. [Google Scholar] [CrossRef]
- Bishop, K.N.; Varacallo, M. Anatomy, Shoulder and Upper Limb, Dorsal Scapular Nerve. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Williams, A.A.; Smith, H.F. Anatomical entrapment of the dorsal scapular and long thoracic nerves, secondary to brachial plexus piercing variation. Anat. Sci. Int. 2020, 95, 67–75. [Google Scholar] [CrossRef]
- Mammucari, M.; Maggiori, E.; Russo, D.; Giorgio, C.; Ronconi, G.; Ferrara, P.E.; Canzona, F.; Antonaci, L.; Violo, B.; Vellucci, R.; et al. Mesotherapy: From Historical Notes to Scientific Evidence and Future Prospects. Sci. World J. 2020, 2020, 3542848. [Google Scholar] [CrossRef] [PubMed]
- Herreros, F.O.C.; de Moraes, A.M.; Velho, P.E.N.F. Mesoterapia: Uma revisão bibliográfica. An. Bras. Dermatol. 2011, 86, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Brauneis, S.; Araimo, F.; Rossi, M.; Russo, D.; Mammuccari, M.; Maggiori, E.; di Marzo, R.; Vellucci, R.; Gori, F.; Bifarini, B.; et al. The role of mesotherapy in the management of spinal pain. A randomized controlled study. La Clin. Ter. 2023, 174, 336–342. [Google Scholar] [PubMed]
- Mammucari, M.; Gatti, A.; Maggiori, S.; Sabato, A.F. Role of Mesotherapy in Musculoskeletal Pain: Opinions from the Italian Society of Mesotherapy. Evid.-Based Complement. Altern. Med. 2012, 2012, 436959. [Google Scholar] [CrossRef]
- Tenforde, A.S.; Borgstrom, H.E.; DeLuca, S.; McCormack, M.; Singh, M.; Hoo, J.S.; Yun, P.H. Best practices for extracorporeal shockwave therapy in musculoskeletal medicine: Clinical application and training consideration. PM R J. Inj. Funct. Rehabil. 2022, 14, 611–619. [Google Scholar] [CrossRef]

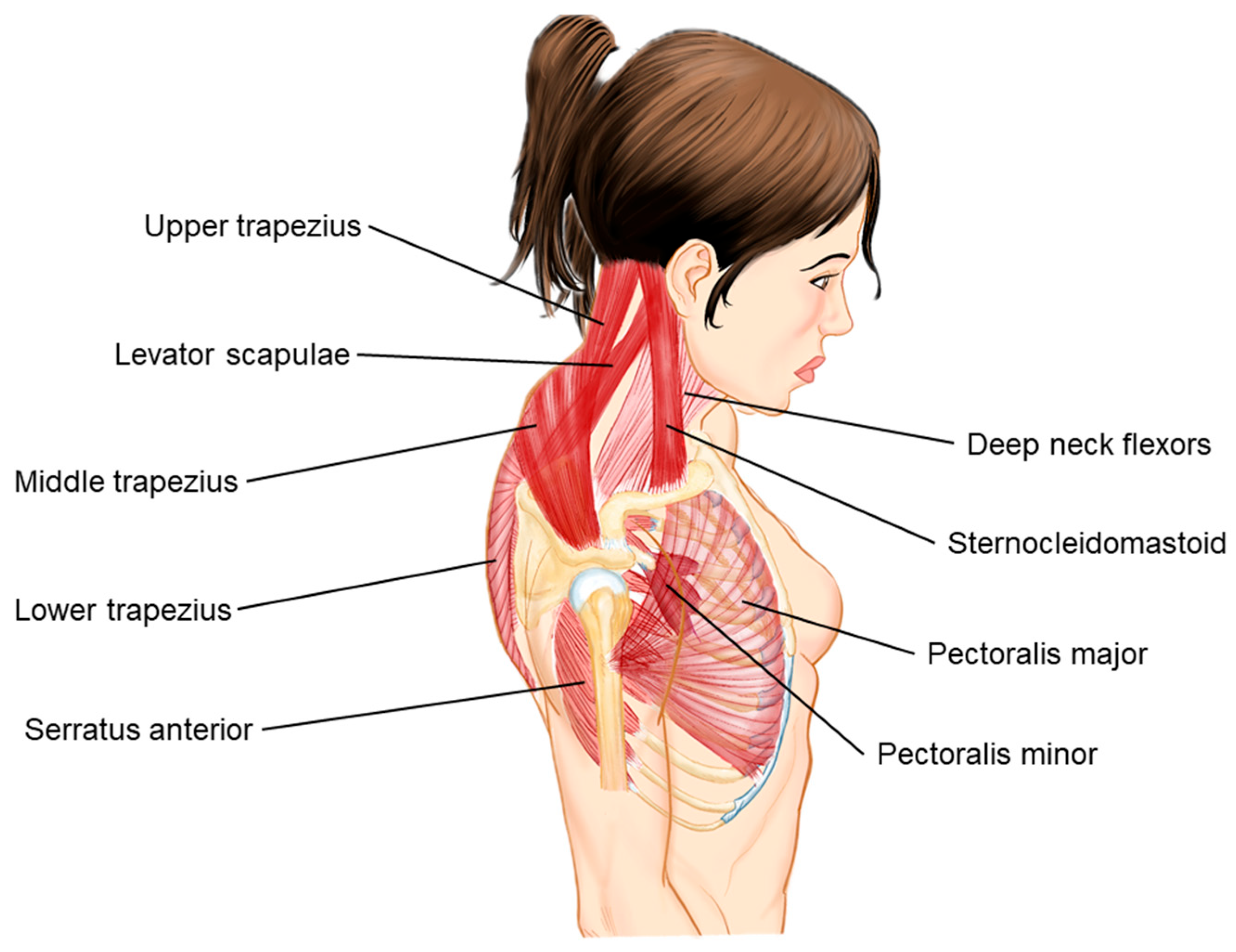







| Anatomic Change | Tightened Muscles | Weakened Muscles |
|---|---|---|
| Shoulder elevation, protraction, and internal rotation | Upper trapezius, levator scapulae, pectoralis minor | Middle trapezius, serratus anterior |
| Chin anteriorization and neck extension | Levator scapulae, suboccipital muscles, sternocleidomastoid | Scalenes, lower trapezius |
| Thoracic kyphosis | Pectoralis minor, pectoralis major, sternocleidomastoid | Scalenes, lower trapezius, middle trapezius |
| Solution Component | Volume | Purpose |
|---|---|---|
| Dextrose 50% | 1.5 mL | Provides osmotic effect for pain relief |
| Procaine 0.7% | 4.8 mL | Local anesthetic to reduce pain |
| Meloxicam 15 mg | 1.5 mL | Anti-inflammatory agent |
| Arnica montana D2 | 2.2 mL | Homeopathic remedy for inflammation |
| N-acetyl-cysteine 100 mg | 3 mL | Antioxidant to reduce oxidative stress |
| Thiocolchicoside 4 mg | 2 mL | Muscle relaxant |
| Total Solution | 15 mL | Combined solution for mesotherapy injection |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pires, L.; Santos, N.; Lana, J.V.; de Macedo, A.P.; Costa, F.R.; Azzini, G.O.M.; Mosaner, T.; de Moraes Ferreira Jorge, D.; Santos, G.S.; Medeiros, A.; et al. Upper Crossed Syndrome and Scapulae Upper-Trapping: A Mesotherapy Protocol in Cervicoscapulobrachial Pain—The 8:1 Block. Bioengineering 2024, 11, 1142. https://doi.org/10.3390/bioengineering11111142
Pires L, Santos N, Lana JV, de Macedo AP, Costa FR, Azzini GOM, Mosaner T, de Moraes Ferreira Jorge D, Santos GS, Medeiros A, et al. Upper Crossed Syndrome and Scapulae Upper-Trapping: A Mesotherapy Protocol in Cervicoscapulobrachial Pain—The 8:1 Block. Bioengineering. 2024; 11(11):1142. https://doi.org/10.3390/bioengineering11111142
Chicago/Turabian StylePires, Luyddy, Napoliane Santos, João Vitor Lana, Alex Pontes de Macedo, Fábio Ramos Costa, Gabriel Ohana Marques Azzini, Tomas Mosaner, Daniel de Moraes Ferreira Jorge, Gabriel Silva Santos, Arthur Medeiros, and et al. 2024. "Upper Crossed Syndrome and Scapulae Upper-Trapping: A Mesotherapy Protocol in Cervicoscapulobrachial Pain—The 8:1 Block" Bioengineering 11, no. 11: 1142. https://doi.org/10.3390/bioengineering11111142
APA StylePires, L., Santos, N., Lana, J. V., de Macedo, A. P., Costa, F. R., Azzini, G. O. M., Mosaner, T., de Moraes Ferreira Jorge, D., Santos, G. S., Medeiros, A., Pereira, J. A. R., & Lana, J. F. (2024). Upper Crossed Syndrome and Scapulae Upper-Trapping: A Mesotherapy Protocol in Cervicoscapulobrachial Pain—The 8:1 Block. Bioengineering, 11(11), 1142. https://doi.org/10.3390/bioengineering11111142







