Comparison of Three Internal Fixation Constructs for AO/OTA 33-A3 Distal Femoral Fractures: A Biomechanical Study
Abstract
1. Introduction
2. Methods
2.1. Materials and Methods
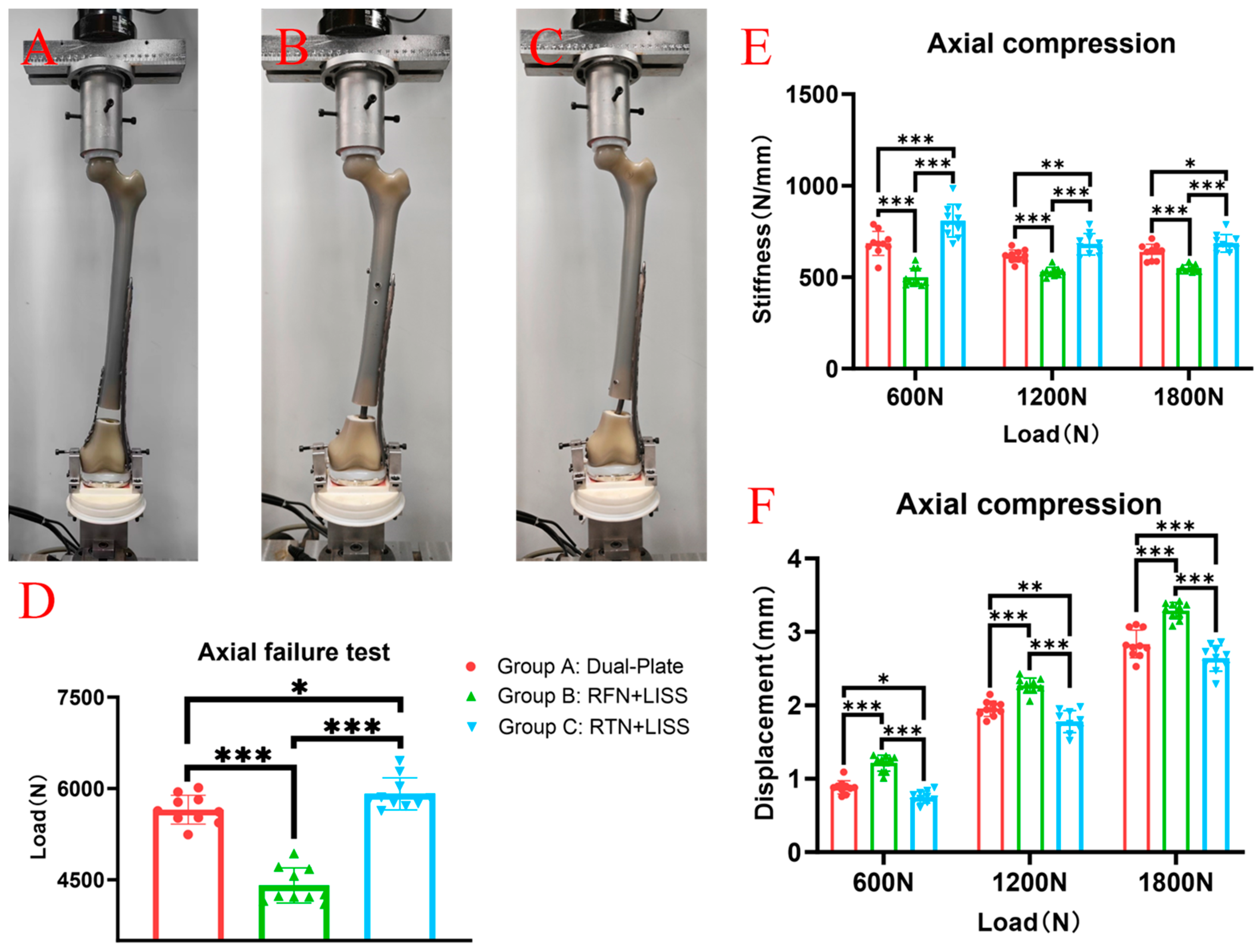
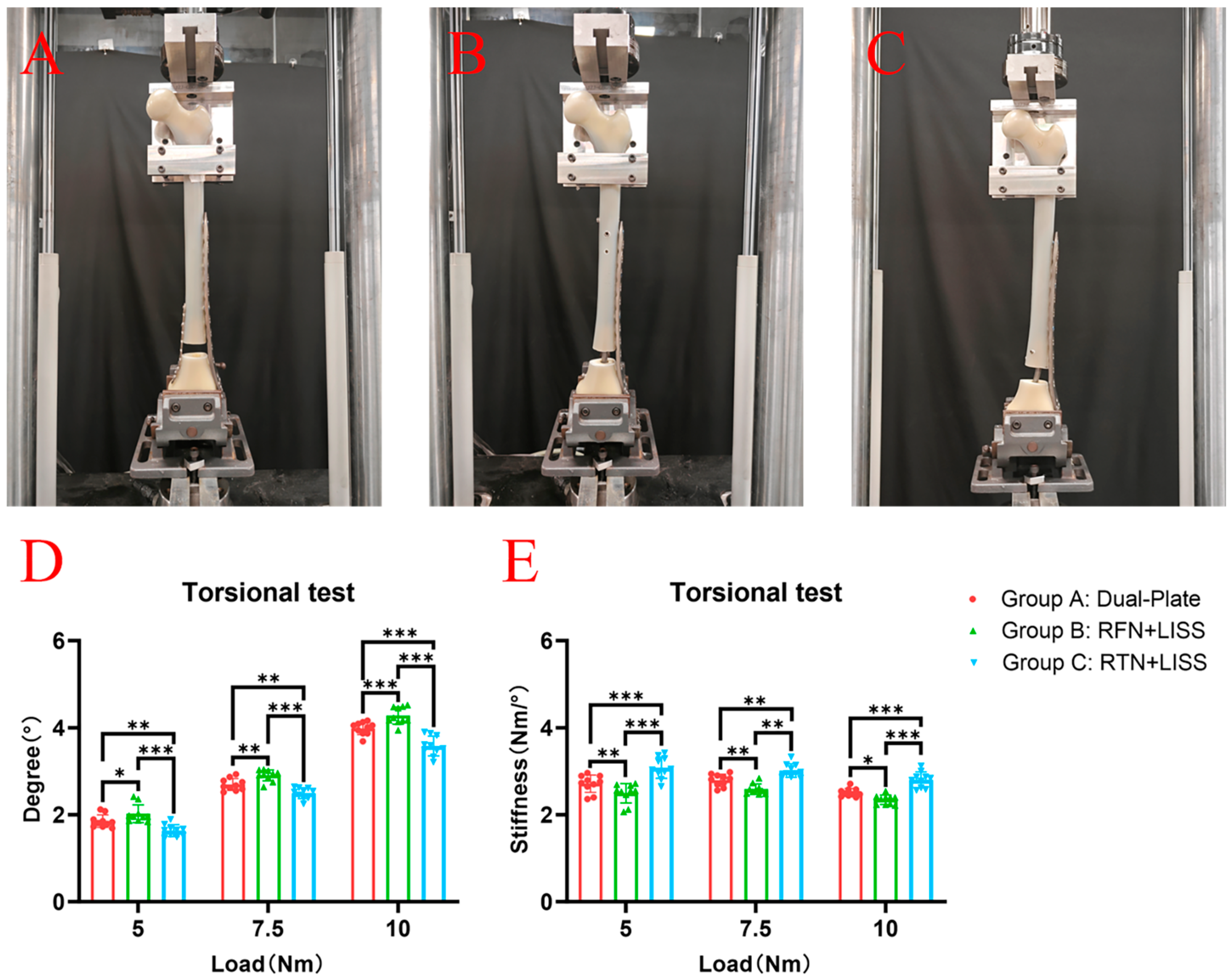
2.2. Biomechanical Testing
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Elsoe, R.; Ceccotti, A.A.; Larsen, P. Population-based epidemiology and incidence of distal femur fractures. Int. Orthop. 2018, 42, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Ambade, R.; Landge, S.; Goyal, S.; Goel, S. Comprehensive Review on Distal Femur Fractures: From Epidemiology to Treatment Strategies. Cureus 2024, 16, e57937. [Google Scholar] [CrossRef] [PubMed]
- Hake, M.E.; Davis, M.E.; Perdue, A.M.; Goulet, J.A. Modern Implant Options for the Treatment of Distal Femur Fractures. J. Am. Acad. Orthop. Surg. 2019, 27, e867–e875. [Google Scholar] [CrossRef] [PubMed]
- Nester, M.; Borrelli, J., Jr. Distal femur fractures management and evolution in the last century. Int. Orthop. 2023, 47, 2125–2135. [Google Scholar] [CrossRef] [PubMed]
- Rinehart, D.; Youngman, T.; Ahn, J.; Huo, M. Review of patient-reported outcomes in periprosthetic distal femur fractures after total knee arthroplasty: A plate or intramedullary nail? Arthroplasty 2021, 3, 24. [Google Scholar] [CrossRef]
- Sain, A.; Sharma, V.; Farooque, K.; Muthukumaran, V.; Pattabiraman, K. Dual Plating of the Distal Femur: Indications and Surgical Techniques. Cureus 2019, 11, e6483. [Google Scholar] [CrossRef]
- Tank, J.C.; Schneider, P.S.; Davis, E.; Galpin, M.; Prasarn, M.L.; Choo, A.M.; Munz, J.W.; Achor, T.S.; Kellam, J.F.; Gary, J.L. Early Mechanical Failures of the Synthes Variable Angle Locking Distal Femur Plate. J. Orthop. Trauma 2016, 30, e7–e11. [Google Scholar] [CrossRef]
- Canadian Orthopaedic Trauma Society. Are Locking Constructs in Distal Femoral Fractures Always Best? A Prospective Multicenter Randomized Controlled Trial Comparing the Less Invasive Stabilization System With the Minimally Invasive Dynamic Condylar Screw System. J. Orthop. Trauma 2016, 30, e1–e6. [Google Scholar] [CrossRef]
- Rodriguez, E.K.; Boulton, C.; Weaver, M.J.; Herder, L.M.; Morgan, J.H.; Chacko, A.T.; Appleton, P.T.; Zurakowski, D.; Vrahas, M.S. Predictive factors of distal femoral fracture nonunion after lateral locked plating: A retrospective multicenter case-control study of 283 fractures. Injury 2014, 45, 554–559. [Google Scholar] [CrossRef]
- Bottlang, M.; Doornink, J.; Lujan, T.J.; Fitzpatrick, D.C.; Marsh, J.L.; Augat, P.; von Rechenberg, B.; Lesser, M.; Madey, S.M. Effects of construct stiffness on healing of fractures stabilized with locking plates. J. Bone Joint Surg. Am. 2010, 92 (Suppl. S2), 12–22. [Google Scholar] [CrossRef]
- Ng, A.C.; Drake, M.T.; Clarke, B.L.; Sems, S.A.; Atkinson, E.J.; Achenbach, S.J.; Melton, L.J., 3rd. Trends in subtrochanteric, diaphyseal, and distal femur fractures, 1984–2007. Osteoporos. Int. 2012, 23, 1721–1726. [Google Scholar] [CrossRef]
- Espey, R.; Stevenson, L.; Tucker, A. Combined nail-plate constructs in the management of osteoporotic native distal femoral fractures: A systematic review of the available evidence. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 3215–3223. [Google Scholar] [CrossRef]
- Stoffel, K.; Sommer, C.; Lee, M.; Zhu, T.Y.; Schwieger, K.; Finkemeier, C. Double fixation for complex distal femoral fractures. EFORT Open Rev. 2022, 7, 274–286. [Google Scholar] [CrossRef] [PubMed]
- Liporace, F.A.; Aneja, A.; Carroll, E.A.; Yoon, R.S. Maintaining the Neutral Axis in the Treatment of Distal Femur Fractures Via Dual Plate or Nail Plate Combination Technique: When and How? J. Orthop. Trauma 2021, 35 (Suppl. S5), S38–S40. [Google Scholar] [CrossRef] [PubMed]
- von Keudell, A.; Shoji, K.; Nasr, M.; Lucas, R.; Dolan, R.; Weaver, M.J. Treatment Options for Distal Femur Fractures. J. Orthop. Trauma 2016, 30 (Suppl. S2), S25–S27. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.J.; Goodnough, L.H.; Salazar, B.P.; Gardner, M.J. Impact on periosteal vasculature after dual plating of the distal femur: A cadaveric study. OTA Int. 2021, 4, e131. [Google Scholar] [CrossRef] [PubMed]
- Wright, D.J.; DeSanto, D.J.; McGarry, M.H.; Lee, T.Q.; Scolaro, J.A. Supplemental Fixation of Supracondylar Distal Femur Fractures: A Biomechanical Comparison of Dual-Plate and Plate-Nail Constructs. J. Orthop. Trauma 2020, 34, 434–440. [Google Scholar] [CrossRef]
- Xie, W.; Luo, D.; Xie, L.; Zhu, L.; Zhou, L.; Lian, K.; Lin, D.; Liu, H. A Biomechanical Comparison Study of Plate-Nail and Dual-Plate Fixation in AO/OTA 41-C2 Tibial Plateau Fractures. Bioengineering 2024, 11, 839. [Google Scholar] [CrossRef]
- Gwathmey, F.W., Jr.; Jones-Quaidoo, S.M.; Kahler, D.; Hurwitz, S.; Cui, Q. Distal femoral fractures: Current concepts. J. Am. Acad. Orthop. Surg. 2010, 18, 597–607. [Google Scholar] [CrossRef]
- Butt, M.S.; Krikler, S.J.; Ali, M.S. Displaced fractures of the distal femur in elderly patients. Operative versus non-operative treatment. J. Bone Joint Surg. Br. 1996, 78, 110–114. [Google Scholar] [CrossRef]
- Kaur, A.; Mohan, S.; Rundle, C.H. A segmental defect adaptation of the mouse closed femur fracture model for the analysis of severely impaired bone healing. Anim. Models Exp. Med. 2020, 3, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Linn, M.S.; McAndrew, C.M.; Prusaczyk, B.; Brimmo, O.; Ricci, W.M.; Gardner, M.J. Dynamic Locked Plating of Distal Femur Fractures. J. Orthop. Trauma 2015, 29, 447–450. [Google Scholar] [CrossRef] [PubMed]
- Cui, S.; Bledsoe, J.G.; Israel, H.; Watson, J.T.; Cannada, L.K. Locked plating of comminuted distal femur fractures: Does unlocked screw placement affect stability and failure? J. Orthop. Trauma 2014, 28, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Fairres, M.J.; Brodke, D.; O’Hara, N.; Devana, S.; Hernandez, A.; Burke, C.; Gupta, J.; McKibben, N.; O’Toole, R.; Morellato, J.; et al. Risk Factors of Failure in 228 Periprosthetic Distal Femur Fractures: A Multicenter Study. J. Orthop. Trauma 2024, 38, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Ricci, W.M.; Streubel, P.N.; Morshed, S.; Collinge, C.A.; Nork, S.E.; Gardner, M.J. Risk factors for failure of locked plate fixation of distal femur fractures: An analysis of 335 cases. J. Orthop. Trauma 2014, 28, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Stockton, D.J.; O’Hara, N.N.; Brodke, D.J.; McKibben, N.; Healey, K.; Goch, A.; Demyanovich, H.; Devana, S.; Hernandez, A.; Burke, C.E.; et al. Technical Factors Contributing to Nonunion in Supracondylar Distal Femur Fractures Treated With Lateral Locked Plating: A Risk-Stratified Analysis. J. Orthop. Trauma 2024, 38, 49–55. [Google Scholar] [CrossRef]
- Beltran, M.J.; Gary, J.L.; Collinge, C.A. Management of distal femur fractures with modern plates and nails: State of the art. J. Orthop. Trauma 2015, 29, 165–172. [Google Scholar] [CrossRef]
- Henderson, C.E.; Kuhl, L.L.; Fitzpatrick, D.C.; Marsh, J.L. Locking plates for distal femur fractures: Is there a problem with fracture healing? J. Orthop. Trauma 2011, 25 (Suppl. S1), S8–S14. [Google Scholar] [CrossRef]
- Lujan, T.J.; Henderson, C.E.; Madey, S.M.; Fitzpatrick, D.C.; Marsh, J.L.; Bottlang, M. Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J. Orthop. Trauma 2010, 24, 156–162. [Google Scholar] [CrossRef]
- Saul, D.; Menger, M.M.; Ehnert, S.; Nüssler, A.K.; Histing, T.; Laschke, M.W. Bone Healing Gone Wrong: Pathological Fracture Healing and Non-Unions-Overview of Basic and Clinical Aspects and Systematic Review of Risk Factors. Bioengineering 2023, 10, 85. [Google Scholar] [CrossRef]
- Kim, H.S.; Yoon, Y.C.; Lee, S.J.; Sim, J.A. Which fixation produces the best outcome for distal femoral fractures? Meta-analysis and systematic review of retrograde nailing versus distal femoral plating in 2432 patients and 33 studies. Eur. J. Trauma Emerg. Surg. 2024, 50, 763–780. [Google Scholar] [CrossRef] [PubMed]
- Baghi, R.; Alon, G.; Oppizzi, G.; Badhyal, S.; Bowman, P.; Zhang, L.Q. Functional Electrical Stimulation of the Lateral Knee Muscles Can Reduce Peak Knee Adduction Moment during Stepping: A Pilot Study. Bioengineering 2024, 11, 881. [Google Scholar] [CrossRef] [PubMed]
- Yocum, D.; Ovispo-Martinez, A.; Valenzuela, K.A.; Wen, C.; Cates, H.; Zhang, S. Investigation of Biomechanical Differences in Level Walking between Patients with Bilateral and Unilateral Total Knee Replacements. Bioengineering 2024, 11, 763. [Google Scholar] [CrossRef] [PubMed]
- Hummer, E.T.; Porter, J.; Cates, H.; Zhang, S. Feasibility of Stationary Cycling with Pedal Force Visual Feedback Post-Total Knee Arthroplasty: Implications for Inter-Limb Deficits in Knee Joint Biomechanics. Bioengineering 2024, 11, 850. [Google Scholar] [CrossRef]
- Babhulkar, S.; Trikha, V.; Babhulkar, S.; Gavaskar, A.S. Current Concepts in Management of Distal Femur Fractures. Injury 2024, 55 (Suppl. S2), 111357. [Google Scholar] [CrossRef] [PubMed]
- Fontenot, P.B.; Diaz, M.; Stoops, K.; Barrick, B.; Santoni, B.; Mir, H. Supplementation of Lateral Locked Plating for Distal Femur Fractures: A Biomechanical Study. J. Orthop. Trauma 2019, 33, 642–648. [Google Scholar] [CrossRef]
- Thorne, T.J.; DeKeyser, G.J.; Clapp, I.; Haller, J.M. Risk of reverse golf club deformity with medial plating of distal femur fracture. Arch. Orthop. Trauma Surg. 2024, 144, 1211–1220. [Google Scholar] [CrossRef]
- Achudan, S.; Antony Xavier, R.P.; Tan, S.E. Medial plating of distal femur: Which pre-contoured angular stable plate fits best? Eur. J. Orthop. Surg. Traumatol. 2024, 34, 3297–3308. [Google Scholar] [CrossRef]
- Liu, H.; Xu, W.; Xiong, Y.; Zhang, J.; Xu, Z.; Wu, J. Retrograde tibial intramedullary nail versus minimally invasive locking plate for extra-articular distal tibial fractures: A comparative and retrospective study. J. Orthop. Surg. Res. 2024, 19, 481. [Google Scholar] [CrossRef]
- Liu, H.; Lin, W.; Xu, W.; Xiong, Y.; Zhang, J.; Wu, J. Comparison of retrograde and antegrade tibial intramedullary nail in the treatment of extra-articular distal tibial fractures. Int. Orthop. 2024, 10, 1–9. [Google Scholar] [CrossRef]
- Giorgio, I.; dell’Isola, F.; Andreaus, U.; Misra, A. An orthotropic continuum model with substructure evolution for describing bone remodeling: An interpretation of the primary mechanism behind Wolff’s law. Biomech. Model. Mechanobiol. 2023, 22, 2135–2152. [Google Scholar] [CrossRef] [PubMed]
- George, D.; Allena, R.; Remond, Y. A multiphysics stimulus for continuum mechanics bone remodeling. Math. Mech. Complex Sy 2018, 6, 307–319. [Google Scholar] [CrossRef]
- Li, X.; Deng, Z.; Lu, W. Mechanistic study of the effect of flexible fixation and load-bearing stress environment on fracture healing and shaping. Anim. Models Exp. Med. 2024. early view. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xie, W.; Liu, H.; Chen, S.; Xu, W.; Lin, W.; Chen, T.; Zhu, L.; Zhai, W.; Wu, J. Comparison of Three Internal Fixation Constructs for AO/OTA 33-A3 Distal Femoral Fractures: A Biomechanical Study. Bioengineering 2024, 11, 1110. https://doi.org/10.3390/bioengineering11111110
Xie W, Liu H, Chen S, Xu W, Lin W, Chen T, Zhu L, Zhai W, Wu J. Comparison of Three Internal Fixation Constructs for AO/OTA 33-A3 Distal Femoral Fractures: A Biomechanical Study. Bioengineering. 2024; 11(11):1110. https://doi.org/10.3390/bioengineering11111110
Chicago/Turabian StyleXie, Wei, Hui Liu, Shufen Chen, Weizhen Xu, Weibin Lin, Tianlai Chen, Lingqi Zhu, Wenliang Zhai, and Jin Wu. 2024. "Comparison of Three Internal Fixation Constructs for AO/OTA 33-A3 Distal Femoral Fractures: A Biomechanical Study" Bioengineering 11, no. 11: 1110. https://doi.org/10.3390/bioengineering11111110
APA StyleXie, W., Liu, H., Chen, S., Xu, W., Lin, W., Chen, T., Zhu, L., Zhai, W., & Wu, J. (2024). Comparison of Three Internal Fixation Constructs for AO/OTA 33-A3 Distal Femoral Fractures: A Biomechanical Study. Bioengineering, 11(11), 1110. https://doi.org/10.3390/bioengineering11111110






