Teledentistry for Pediatric Dental Emergency: Comparison Between Experienced and Novice Users
Abstract
1. Introduction
2. Materials and Methods
2.1. Teledentistry Index (TDI)
2.2. Usability and Confidence Survey
2.3. Statistical Analysis
3. Results
3.1. Demographics of Study Participants
3.2. Teledentistry in Different Scenarios
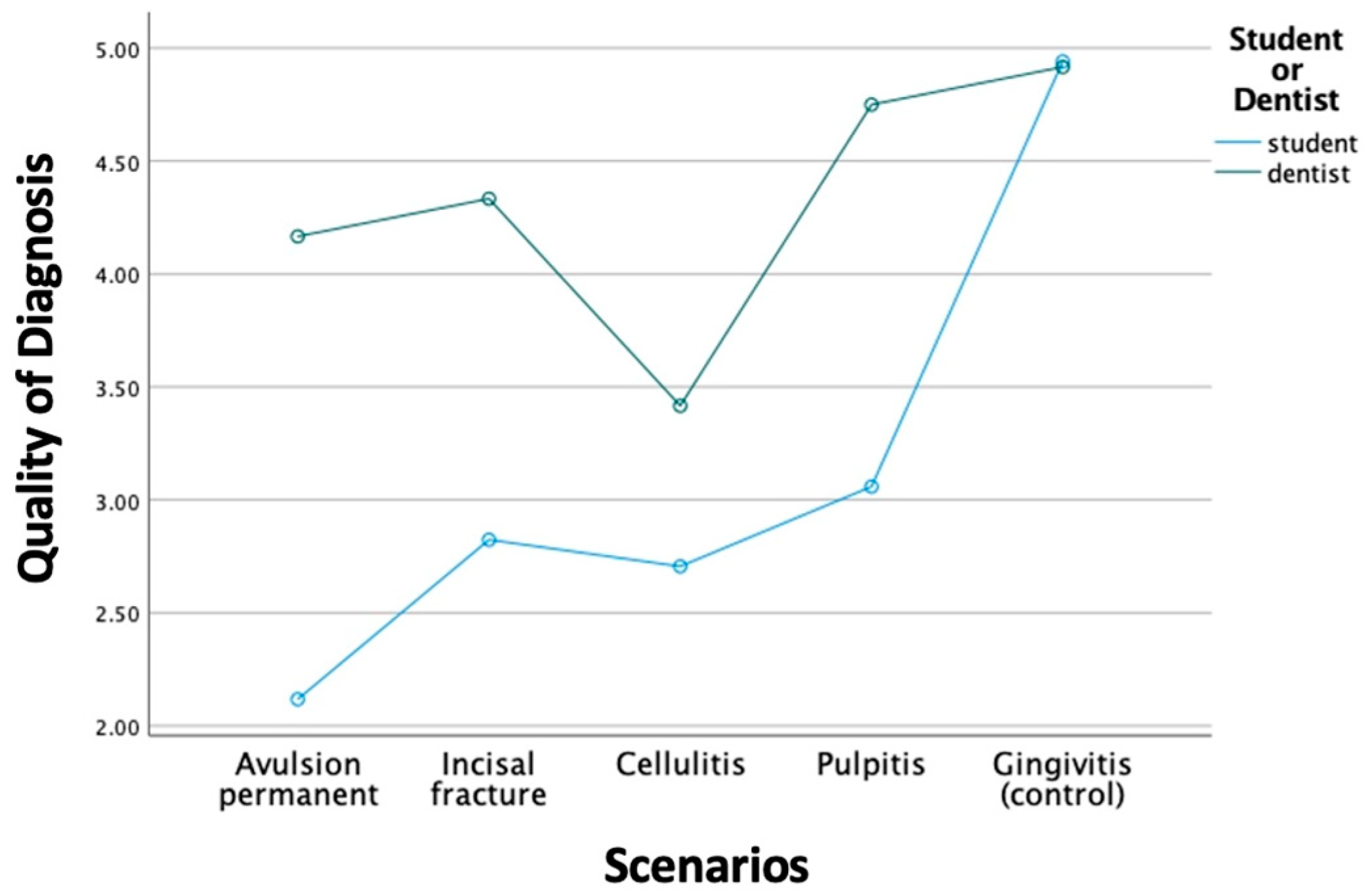
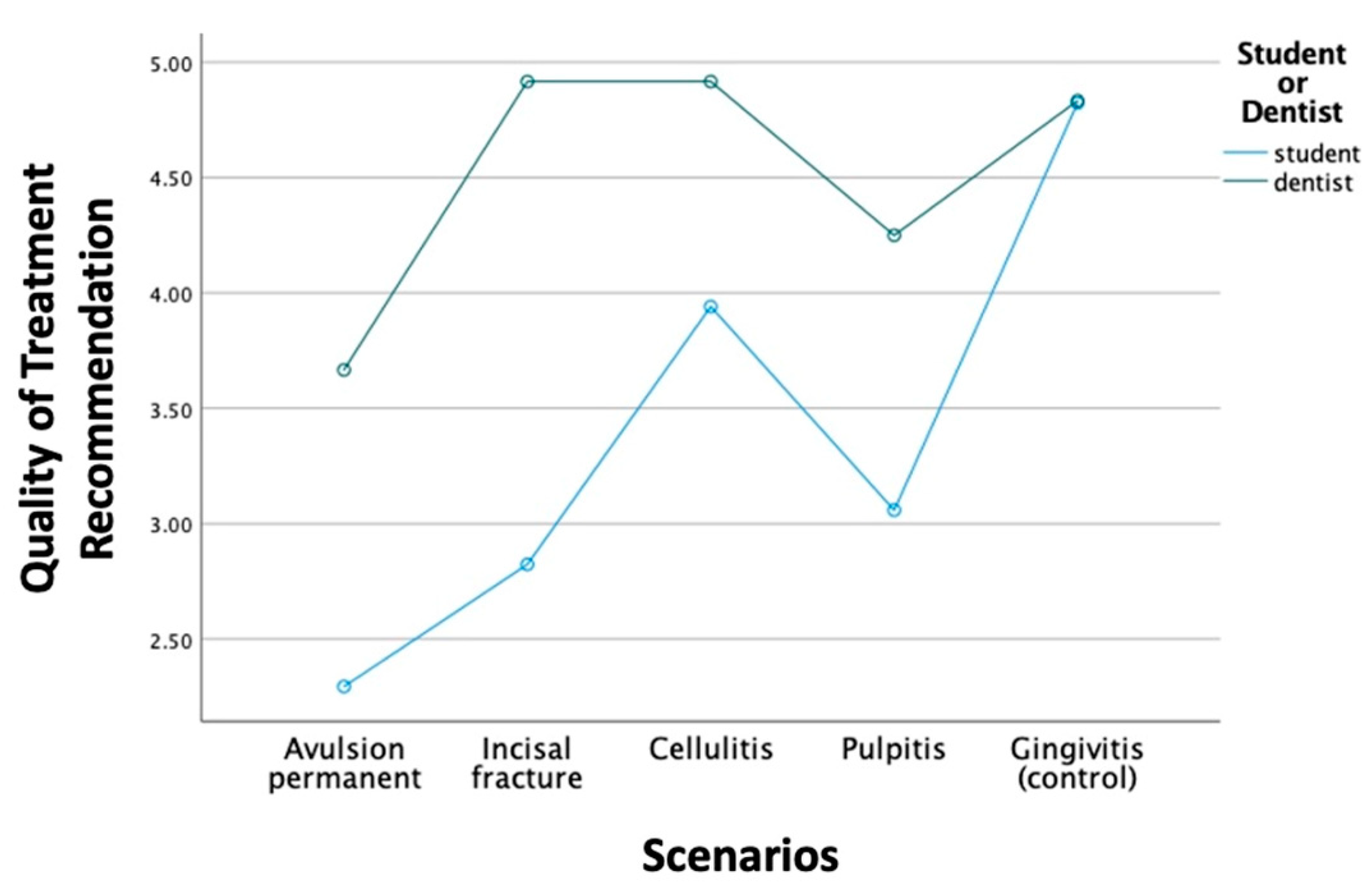
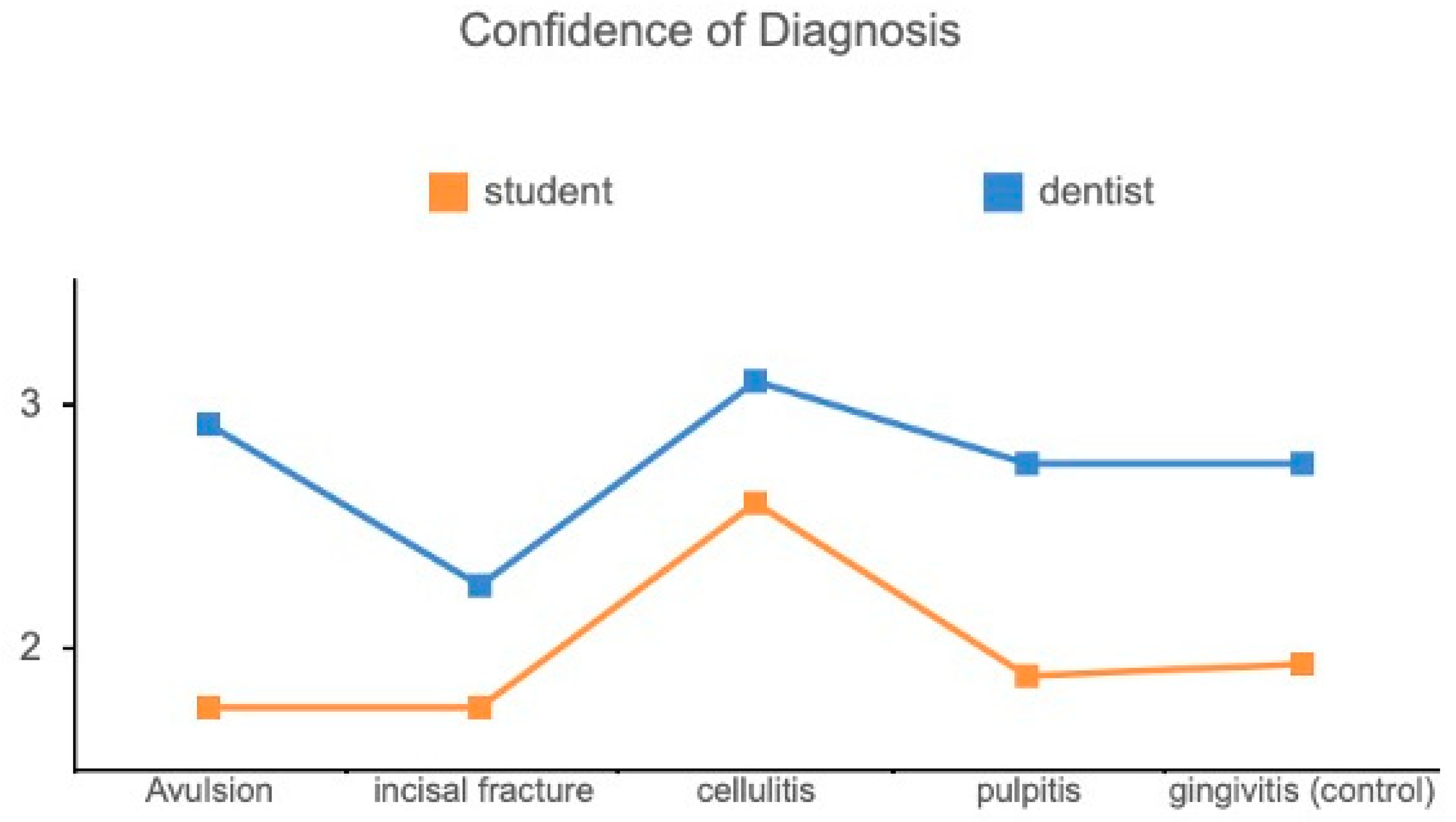
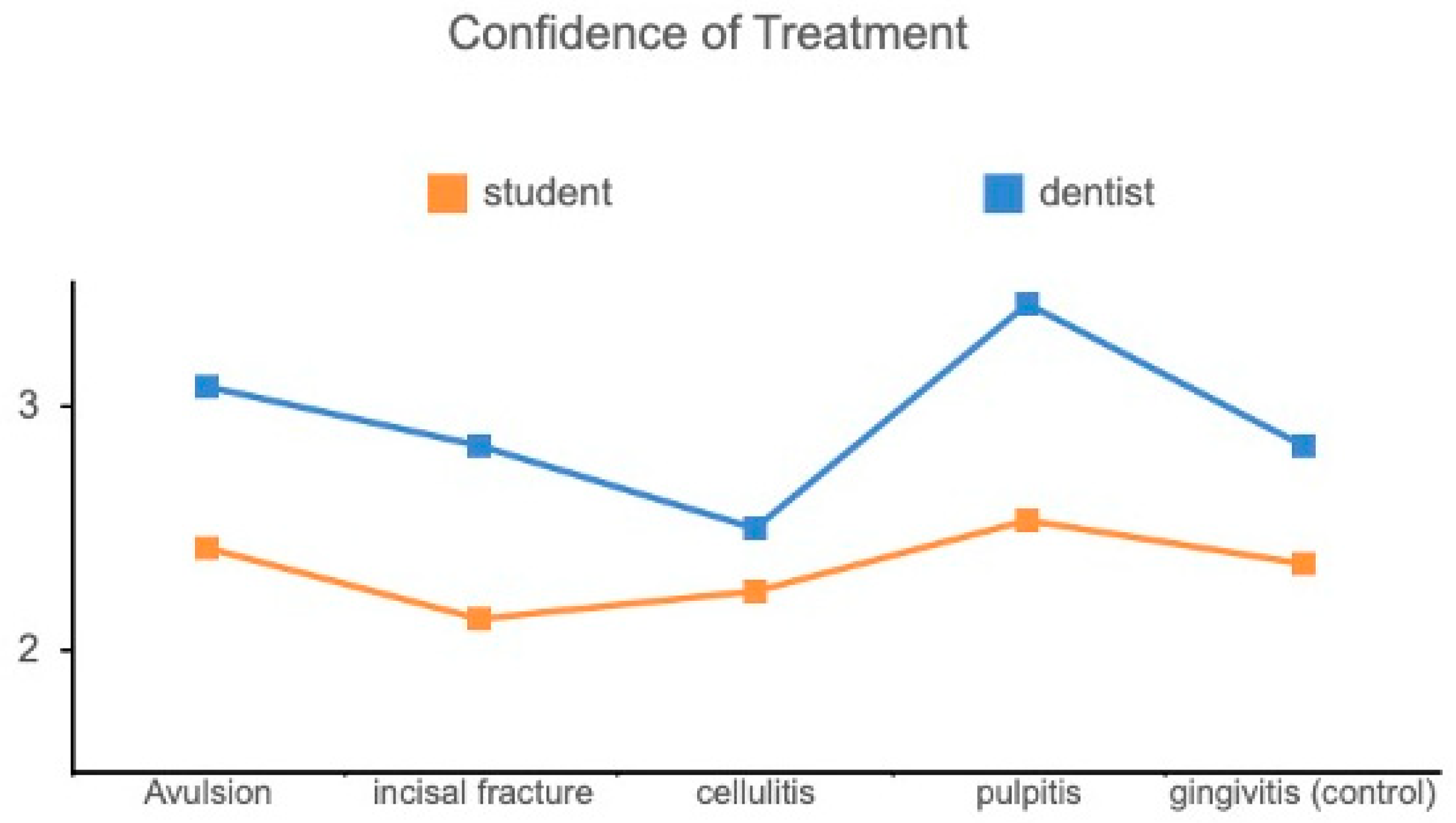
3.3. Comparison Between General Dentists and Dental Students
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- ATDA_Teledental Practice Position Paper. American Teledentsitry Association. ATDA Position Papers and Research. Available online: https://www.americanteledentistry.org/white-papers/ (accessed on 2 February 2023.).
- ADA Guide to Understanding and Documenting Teledentistry Events. American Teledentsitry Association. ATDA External Papers. Available online: https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/publications/cdt/v4_d9995andd9996__adaguidetounderstandinganddocumentingteledentistryevents_2023jan.pdf (accessed on 2 February 2023).
- Jampani, N.D.; Nutalapati, R.; Dontula, B.S.; Boyapati, R. Applications of teledentistry: A literature review and update. J. Int. Soc. Prev. Community Dent. 2011, 1, 37–44. [Google Scholar] [PubMed]
- UP White Paper Teledentistry Improving Oral Health Using Telehealth-Connected Teams. American Teledentsitry Association. ATDA External Papers. Available online: https://www.americanteledentistry.org/wp-content/uploads/2018/02/UofP_WhitePaper_Telehealth.pdf (accessed on 2 February 2023).
- Flores, A.; Lazaro, S.A.; Molina-Bastos, C.G.; Guattini, V.L.O.; Umpierre, R.N.; Goncalves, M.R.; Carrard, V.C. Teledentistry in the diagnosis of oral lesions: A systematic review of the literature. J. Am. Med. Inform. Assoc. 2020, 27, 1166–1172. [Google Scholar] [CrossRef] [PubMed]
- Wallace, C.K.; Schofield, C.E.; Burbridge, L.A.L.; O’Donnell, K.L. Role of teledentistry in paediatric dentistry. Br. Dent. J. 2021, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Estai, M.; Kanagasingam, Y.; Mehdizadeh, M.; Vignarajan, J.; Norman, R.; Huang, B.; Spallek, H.; Irving, M.; Arora, A.; Kruger, E.; et al. Teledentistry as a novel pathway to improve dental health in school children: A research protocol for a randomised controlled trial. BMC Oral Health 2020, 20, 11. [Google Scholar] [CrossRef] [PubMed]
- Ackerman, M.B. Teleorthodontic treatment with clear aligners: An analysis of outcome in treatment supervised by general practitioners versus orthodontic specialists. J. Dent. Res. Rep. 2019, 2, 1–4. [Google Scholar] [CrossRef]
- Carrard, V.C.; Roxo Goncalves, M.; Rodriguez Strey, J.; Pilz, C.; Martins, M.; Martins, M.D.; Schmitz, C.A.; Dal Moro, R.G.; D’Avila, O.P.; Rados, D.; et al. Telediagnosis of oral lesions in primary care: The EstomatoNet Program. Oral Dis. 2018, 24, 1012–1019. [Google Scholar] [CrossRef]
- Khan, S.A.; Omar, H. Teledentistry in practice: Literature review. Telemed. J. e-Health 2013, 19, 565–567. [Google Scholar] [CrossRef]
- ATDA-Teledentistry-Efficacy-One-Pager. American Teledentistry Association. Available online: https://www.americanteledentistry.org/white-papers/ (accessed on 2 February 2023).
- Bahramian, H.; Gharib, B.; Baghalian, A. COVID-19 Considerations in Pediatric Dentistry. JDR Clin. Transl. Res. 2020, 5, 307–311. [Google Scholar] [CrossRef]
- Abbas, B.; Wajahat, M.; Saleem, Z.; Imran, E.; Sajjad, M.; Khurshid, Z. Role of Teledentistry in COVID-19 Pandemic: A Nationwide Comparative Analysis among Dental Professionals. Eur. J. Dent. 2020, 14, S116–S122. [Google Scholar] [CrossRef]
- Batra, P.; Tagra, H.; Katyal, S. Artificial Intelligence in Teledentistry. Discoveries 2022, 10, 153. [Google Scholar] [CrossRef]
- Ibrahim, S.A.; Pronovost, P.J. Diagnostic Errors, Health Disparities, and Artificial Intelligence. JAMA Health Forum 2021, 2, e212430. [Google Scholar] [CrossRef] [PubMed]
- Ghai, S. Teledentistry during COVID-19 pandemic. Diabetes Metab. Syndr. 2020, 14, 933–935. [Google Scholar] [CrossRef] [PubMed]
- Jayaraman, J.; Dhar, V.; Moorani, Z.; Donly, K.; Tinanoff, N.; Mitchell, S.; Wright, T. Impact of COVID-19 on Pediatric Dental Practice in the United States. Pediatr. Dent. 2020, 42, 180–183. [Google Scholar] [PubMed]
- Haimi, M.; Brammli-Greenberg, S.; Baron-Epel, O.; Waisman, Y. Assessing patient safety in a pediatric telemedicine setting: A multi-methods study. BMC Med. Inform. Decis. Mak. 2020, 20, 63. [Google Scholar] [CrossRef] [PubMed]
- Gurgel-Juarez, N.; Torres-Pereira, C.; Haddad, A.E.; Sheehy, L.; Finestone, H.; Mallet, K.; Wiseman, M.; Hour, K.; Flowers, H.L. Accuracy and effectiveness of teledentistry: A systematic review of systematic reviews. Evid.-Based Dent. 2022, 1–8. [Google Scholar] [CrossRef]
- Alabdullah, J.H.; Daniel, S.J. A Systematic Review on the Validity of Teledentistry. Telemed. J. e-Health 2018, 24, 639–648. [Google Scholar] [CrossRef]
- De Vasconcellos, L.G.O.; Brentel, A.S.; Vanderlei, A.D.; De Vasconcellos, L.M.R.; Valera, M.C.; De Araujo, M.A.M. Knowledge of general dentists in the current guidelines for emergency treatment of avulsed teeth and dental trauma prevention. Dent. Traumatol. 2009, 25, 578–583. [Google Scholar] [CrossRef]
- Rodd, H.D.; Farman, M.; Albadri, S.; Mackie, I.C. Undergraduate experience and self-assessed confidence in paediatric dentistry: Comparison of three UK dental schools. Br. Dent. J. 2010, 208, 221–225. [Google Scholar] [CrossRef]
- Machado, J.P.; Lam, X.T.; Chen, J.W. Use of a clinical decision support tool for the management of traumatic dental injuries in the primary dentition by novice and expert clinicians. Dent. Traumatol. 2018, 34, 120–128. [Google Scholar] [CrossRef]
- Ines Meurer, M.; Caffery, L.J.; Bradford, N.K.; Smith, A.C. Accuracy of dental images for the diagnosis of dental caries and enamel defects in children and adolescents: A systematic review. J. Telemed. Telecare 2015, 21, 449–458. [Google Scholar] [CrossRef]
- Yousaf, A.; Ali, F.; Zahra, S.F.T.; Hussain, S.M.; Banghar, F.; Bangash, K.A. DENTAL CONSIDERATIONS DURING THE OUTBREAK OF CORONA VIRUS DISEASE 2019 (COVID-19). Pak. Armed Forces Med. J. 2020, 70, S225-31. [Google Scholar]
- Kavadella, A.; Dias da Silva, M.A.; Kaklamanos, E.G.; Stamatopoulos, V.; Giannakopoulos, K. Evaluation of ChatGPT’s Real-Life Implementation in Undergraduate Dental Education: Mixed Methods Study. JMIR Med. Educ. 2024, 10, e51344. [Google Scholar] [CrossRef]
- Martens, L.C.; Rajasekharan, S.; Jacquet, W.; Vandenbulcke, J.D.; Van Acker, J.W.G.; Cauwels, R. Paediatric dental emergencies: A retrospective study and a proposal for definition and guidelines including pain management. Eur. Arch. Paediatr. Dent. 2018, 19, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.P.; Tsai, A.I.; Chen, C.M. A 2-year retrospective study of pediatric dental emergency visits at a hospital emergency center in Taiwan. Biomed. J. 2016, 39, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Fouad, A.F.; Abbott, P.V.; Tsilingaridis, G.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; O’Connell, A.; Flores, M.T.; Day, P.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2020, 36, 331–342. [Google Scholar] [CrossRef]
- Chen, J.W.; Hobdell, M.H.; Dunn, K.; Johnson, K.A.; Zhang, J. Teledentistry and its use in dental education. J. Am. Dent. Assoc. 2003, 134, 342–346. [Google Scholar] [CrossRef]
- Healthcare-Access_Telehealth. American Teledentsitry Association. ATDA External Papers. Available online: http://www.americanteledentistry.org/wp-content/uploads/2019/06/Healthcare-Access_Telehealth_v03_web.pdf (accessed on 2 February 2023).
- State Telehealth Laws and Medicaid Program Policies. Available online: https://www.cchpca.org/2023/05/Spring2023_ExecutiveSummary.pdf (accessed on 2 February 2023).
| Characteristic | Dental Students (N = 85) | General Dentists (N = 60) | p-Value (X2 Test) |
|---|---|---|---|
| Age | <0.001 * | ||
| 20–30 years old | 76 (89.4%) | 6 (10.0%) | |
| 31–40 years old | 9 (10.6%) | 25 (41.7%) | |
| >40 years old | 0 | 29 (48.3%) | |
| Years in practice | <0.001 * | ||
| Students | 80 (94%) | 0 | |
| <2 years | 2 (2.5%) | 7 (11.6%) | |
| 2–5 years | 3 (3.5%) | 10 (16.7%) | |
| 6–10 years | 0 | 9 (15%) | |
| >10 years | 0 | 34 (56.7%) | |
| Gender | 0.365 (NS) | ||
| Male | 43 (50.6%) | 26 (43.3%) | |
| Female | 42 (49.4%) | 33 (55%) | |
| Do not want to disclose | 0 | 1 (1.7%) | |
| Practice setting | |||
| Student | 85 (100%) | 0 | <0.001 * |
| Full-time faculty | 0 | 29 (48.3%) | |
| Private practitioner | 0 | 29 (48.3%) | |
| Community health | 0 | 2 (3.4%) | |
| Sensitivity of diagnosis | 54.4% | 83.3% | |
| Sensitivity of treatment planning | 57.4% | 93.8% |
| TDI | Avulsion | Incisal Fracture | Cellulitis | Pulpitis | Gingivitis (Control) | p-Value |
|---|---|---|---|---|---|---|
| QD | 2.97 (±1.64) | 3.45 (±1.35) | 3.00 (±1.13) | 3.76 (±1.50) | 4.93 (±0.26) | <0.001 * |
| QT | 2.86 (±1.38) | 3.69 (±1.56) | 4.34 (±1.26) | 3.55 (±1.27) | 4.83 (±0.47) | <0.001 * |
| CD | 2.24 (±1.18) | 1.97 (±1.12) | 2.79 (±0.86) | 2.24 (±1.12) | 2.28 (±1.07) | 0.045 * |
| CT | 2.69 (±1.00) | 2.41 (±1.12) | 2.34 (±0.90) | 2.90 (±1.05) | 2.55 (±1.12) | 0.150 |
| DI (%) | 39.90 (±15.08) | 34.14 (±11.50) | 39.28 (±9.76) | 44.65 (±11.48) | 40.17 (±14.48) | 0.042 * |
| Avulsion | Incisal Fracture | Cellulitis | Pulpitis | Gingivitis (Control) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DS | GD | DS | GD | DS | GD | DS | GD | DS | GD | |
| QD | 2.12 (±1.27) | 4.17 (±1.34) | 2.82 (±1.13) | 4.33 (±1.15) | 2.71 (±1.16) | 3.42 (±1.00) | 3.06 (±1.48) | 4.75 (±0.87) | 4.94 (±0.24) | 4.92 (±0.29) |
| QT | 2.30 (±1.26) | 3.67 (±1.15) | 2.82 (±1.51) | 4.92 (±0.29) | 3.94 (±1.52) | 4.92 (±0.29) | 3.06 (±1.34) | 4.25 (±0.75) | 4.82 (±0.53) | 4.83 (±0.39) |
| CD | 1.76 (±1.15) | 2.92 (±0.90) | 1.76 (±1.25) | 2.25 (±0.87) | 2.59 (±0.87) | 3.09 (±0.79) | 1.88 (±0.86) | 2.75 (±1.29) | 1.94 (±1.20) | 2.75 (±0.62) |
| CT | 2.41 (±1.00) | 3.08 (±0.90) | 2.12 (±1.05) | 2.83 (±1.11) | 2.24 (±1.03) | 2.50 (±0.67) | 2.53 (±1.18) | 3.42 (±0.51) | 2.35 (±1.17) | 2.83 (±1.03) |
| DI (%) | 38.93 (±12.74) | 41.27 (±18.42) | 30.88 (±11.07) | 38.75 (±10.90) | 39.64 (±7.19) | 38.77 (±12.91) | 43.34 (±11.84) | 46.49 (±11.18) | 38.53 (±12.60) | 42.50 (±17.12) |
| TDI | Age | Years in Practice | ||
|---|---|---|---|---|
| Correlation Coefficient | Sig. (2-Tailed) | Correlation Coefficient | Sig. (2-Tailed) | |
| QD | 0.309 | <0.001 * | 0.408 | <0.001 * |
| QT | 0.266 | 0.001 * | 0.325 | <0.001 * |
| CD | 0.287 | <0.001 * | 0.278 | <0.001 * |
| CT | 0.211 | 0.011 * | 0.262 | 0.001 * |
| Usability | Dental Students (N = 85) | General Dentists (N = 60) | p-Value (X2 Test) |
|---|---|---|---|
| The teledentistry is helpful in making a diagnosis. | 0.211 | ||
| Strongly agree | 7 (8.2%) | 5 (8.3%) | |
| Agree | 39 (45.9%) | 22 (36.7%) | |
| Neutral | 22 (25.9%) | 20 (33.3%) | |
| Disagree | 17 (20%) | 10 (16.7%) | |
| Strongly disagree | 0 | 3 | |
| The teledentistry is helpful in making a treatment recommendation. | 0.327 | ||
| Strongly agree | 7 (8.2%) | 5 (8.3%) | |
| Agree | 49 (57.6%) | 35 (58.3%) | |
| Neutral | 20 (23.5%) | 12 (20%) | |
| Disagree | 9 (10.6%) | 5 (8.3%) | |
| Strongly disagree | 0 | 3 (5%) | |
| The teledentistry is easy to use. | 0.742 | ||
| Strongly agree | 13 (15.3%) | 8 (13.3%) | |
| Agree | 51 (60%) | 40 (66.7%) | |
| Neutral | 15 (17.6%) | 10 (16.7%) | |
| Disagree | 6 (7.1%) | 2 (3.33%) | |
| Strongly disagree | 0 | 0 | |
| I like to use teledentistry in my practice. | 0.059 | ||
| I will always use it. | 1 (1.2%) | 2 (3.33%) | |
| I will often use it. | 22 (25.9%) | 7 (11.7%) | |
| I will sometimes use it. | 51 (60%) | 34 (56.7%) | |
| I will rarely use it. | 8 (9.4%) | 14 (23.3%) | |
| I will never use it. | 3 (3.5%) | 3 (5%) | |
| Teledentistry will improve the care I provided. | 0.348 | ||
| Strongly agree | 8 (9.4%) | 4 (6.7%) | |
| Agree | 55 (64.7%) | 32 (53.3%) | |
| Neutral | 17 (20%) | 19 (31.7%) | |
| Disagree | 4 (4.7%) | 5 (8.3%) | |
| Strongly disagree | 1 (1.2%) | 0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C.-C.; Chen, J.-W. Teledentistry for Pediatric Dental Emergency: Comparison Between Experienced and Novice Users. Bioengineering 2024, 11, 1054. https://doi.org/10.3390/bioengineering11111054
Huang C-C, Chen J-W. Teledentistry for Pediatric Dental Emergency: Comparison Between Experienced and Novice Users. Bioengineering. 2024; 11(11):1054. https://doi.org/10.3390/bioengineering11111054
Chicago/Turabian StyleHuang, Chih-Chieh, and Jung-Wei Chen. 2024. "Teledentistry for Pediatric Dental Emergency: Comparison Between Experienced and Novice Users" Bioengineering 11, no. 11: 1054. https://doi.org/10.3390/bioengineering11111054
APA StyleHuang, C.-C., & Chen, J.-W. (2024). Teledentistry for Pediatric Dental Emergency: Comparison Between Experienced and Novice Users. Bioengineering, 11(11), 1054. https://doi.org/10.3390/bioengineering11111054







