Comparison of G8 and ISAR Screening Results in Geriatric Urology
Abstract
:1. Introduction
2. Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
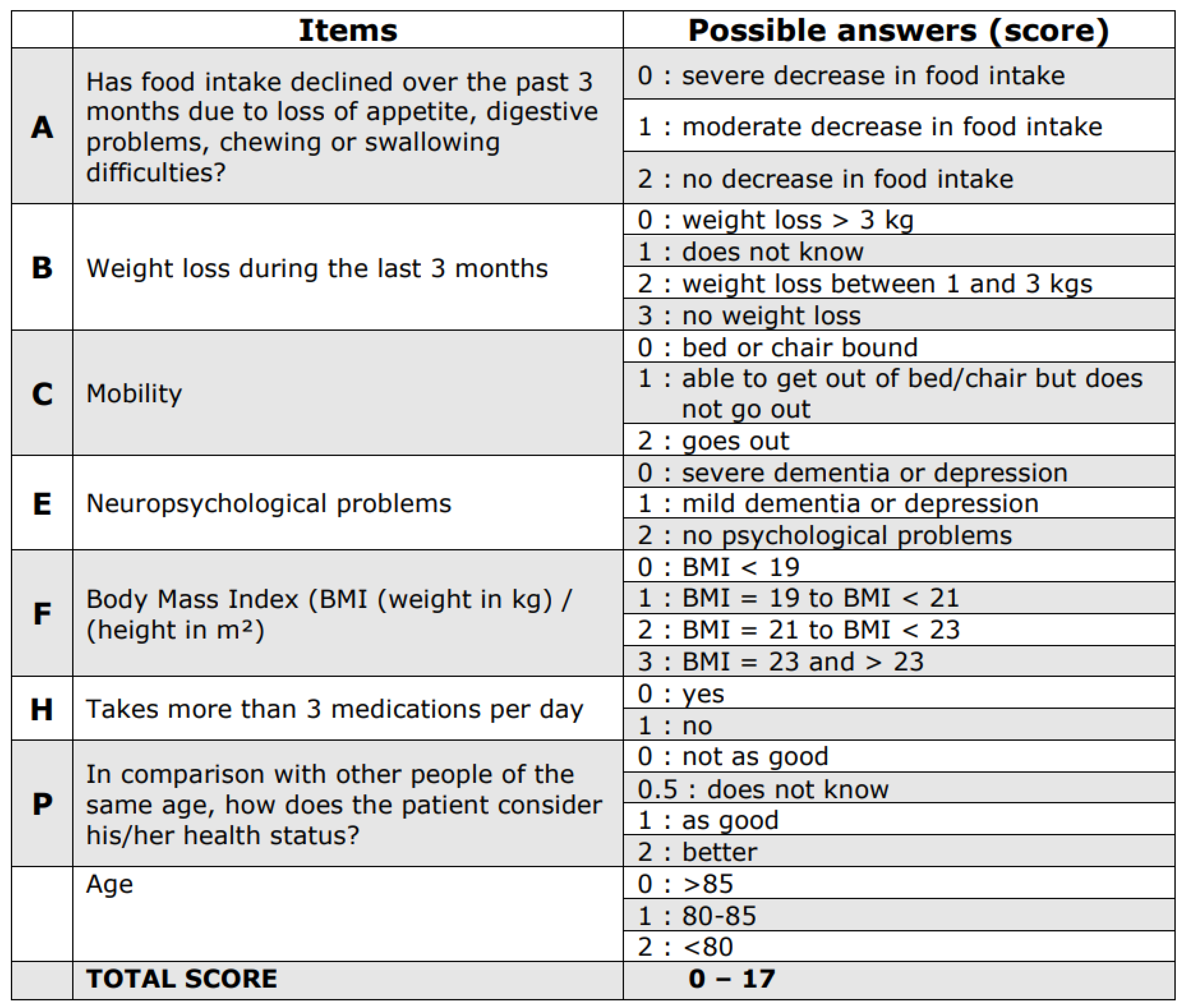
Appendix A. G8 Score
Appendix B
| Yes | No | |
|---|---|---|
| Before the illness that brought you to the hospital, did you need someone to help you on a regular basis? | 1 | 0 |
| Since the illness or injury that brought you to the hospital, have you needed more help than usually before? | 1 | 0 |
| Have you been hospitalized for more for one or more nights during the past 6 months? | 1 | 0 |
| In general, is your sight (with glasses) good? | 0 | 1 |
| In general, do you have serious problems with your memory? | 1 | 0 |
| Do you take more than six different medications every day? | 1 | 0 |
References
- Wiedemann, A. Geriatric urology: Increasingly important in urological care. Urologe A 2017, 56, 992–996. [Google Scholar] [CrossRef]
- Jang, I.Y.; Lee, C.K.; Jung, H.W.; Yu, S.S.; Lee, Y.S.; Lee, E.; Kim, D.H. Urologic symptoms and burden of frailty and geriatric conditions in older men: The Aging Study of PyeongChang Rural Area. Clin. Interv. Aging 2018, 13, 297–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michalik, C.; Juszczak, K.; Maciukiewicz, P.; Drewa, T.; Kenig, J. Geriatric assessment among elderly patients undergoing urological surgery: A systematic literature review. Adv. Clin. Exp. Med. 2020, 29, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Extermann, M.; Aapro, M.; Bernabei, R.; Cohen, H.J.; Droz, J.P.; Lichtman, S.; Mor, V.; Monfardini, S.; Repetto, L.; Sorbye, L.; et al. Use of comprehensive geriatric assessment in older cancer patients: Recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit. Rev. Oncol. Hematol. 2005, 55, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Kenis, C.; Bron, D.; Libert, Y.; Decoster, L.; Van Puyvelde, K.; Scalliet, P.; Cornette, P.; Pepersack, T.; Luce, S.; Langenaeken, C.; et al. Relevance of a systematic geriatric screening and assessment in older patients with cancer: Results of a prospective multicentric study. Ann. Oncol. 2013, 24, 1306–1312. [Google Scholar] [CrossRef] [PubMed]
- Overcash, J.A.; Beckstead, J.; Extermann, M.; Cobb, S. The abbreviated comprehensive geriatric assessment (aCGA): A retrospective analysis. Crit. Rev. Oncol. Hematol. 2005, 54, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Decoster, L.; Van Puyvelde, K.; Mohile, S.; Wedding, U.; Basso, U.; Colloca, G.; Rostoft, S.; Overcash, J.; Wildiers, H.; Steer, C.; et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: An update on SIOG recommendationsdagger. Ann. Oncol. 2015, 26, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Xue, Q.L. The frailty syndrome: Definition and natural history. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Montroni, I.; Rostoft, S.; Spinelli, A.; Van Leeuwen, B.L.; Ercolani, G.; Saur, N.M.; Jaklitsch, M.T.; Somasundar, P.S.; de Liguori Carino, N.; Ghignone, F.; et al. GOSAFE—Geriatric Oncology Surgical Assessment and Functional rEcovery after Surgery: Early analysis on 977 patients. J. Geriatr. Oncol. 2020, 11, 244–255. [Google Scholar] [CrossRef] [Green Version]
- Mottet, N.; Bellmunt, J.; Bolla, M.; Briers, E.; Cumberbatch, M.G.; De Santis, M.; Fossati, N.; Gross, T.; Henry, A.M.; Joniau, S.; et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2017, 71, 618–629. [Google Scholar] [CrossRef]
- Cavusoglu, C.; Deniz, O.; Tuna Dogrul, R.; Ileri, I.; Yildirim, F.; Caliskan, H.; Ozsurekci, C.; Coteli, S.; Kizilarslanoglu, M.C.; Goker, B. Validity and reliability of the G8 screening test in older non-cancer patients. Eur. Geriatr. Med. 2021, 12, 397–404. [Google Scholar] [CrossRef]
- Wiedemann, A.; Puttmann, J.; Heppner, H. The ISAR-positive patient in urology. Aktuelle. Urol. 2019, 50, 100–105. [Google Scholar] [CrossRef]
- Singler, K.; Heppner, H.J.; Skutetzky, A.; Sieber, C.; Christ, M.; Thiem, U. Predictive validity of the identification of seniors at risk screening tool in a German emergency department setting. Gerontology 2014, 60, 413–419. [Google Scholar] [CrossRef] [Green Version]
- Souwer, E.T.D.; Verweij, N.M.; van den Bos, F.; Bastiaannet, E.; Slangen, R.M.E.; Steup, W.H.; Hamaker, M.E.; Portielje, J.E.A. Risk stratification for surgical outcomes in older colorectal cancer patients using ISAR-HP and G8 screening tools. J. Geriatr. Onco.l 2018, 9, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Schulkes, K.J.G.; Souwer, E.T.D.; van Elden, L.J.R.; Codrington, H.; van der Sar-van der Brugge, S.; Lammers, J.J.; Portielje, J.E.A.; van den Bos, F.; Hamaker, M.E. Prognostic Value of Geriatric 8 and Identification of Seniors at Risk for Hospitalized Patients Screening Tools for Patients With Lung Cancer. Clin. Lung. Cancer 2017, 18, 660–666.e1. [Google Scholar] [CrossRef] [PubMed]
- Scharf, A.C.; Gronewold, J.; Dahlmann, C.; Schlitzer, J.; Kribben, A.; Gerken, G.; Rassaf, T.; Kleinschnitz, C.; Dodel, R.; Frohnhofen, H.; et al. Health outcome of older hospitalized patients in internal medicine environments evaluated by Identification of Seniors at Risk (ISAR) screening and geriatric assessment. BMC Geriatr. 2019, 19, 221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bellera, C.A.; Rainfray, M.; Mathoulin-Pelissier, S.; Mertens, C.; Delva, F.; Fonck, M.; Soubeyran, P.L. Screening older cancer patients: First evaluation of the G-8 geriatric screening tool. Ann. Onco.l 2012, 23, 2166–2172. [Google Scholar] [CrossRef]
- Rassam, Y.; Schindler, A.; Willschrei, P.; Horstmann, M. The G8 questionnaire as a geriatric screening tool in urooncology. Aktuelle. Urol. 2020, 51, 36–41. [Google Scholar] [CrossRef] [PubMed]
- McCusker, J.; Bellavance, F.; Cardin, S.; Trepanier, S. Screening for geriatric problems in the emergency department: Reliability and validity. Identification of Seniors at Risk (ISAR) Steering Committee. Acad. Emerg. Med. 1998, 5, 883–893. [Google Scholar] [CrossRef]
- Slankamenac, K.; Haberkorn, G.; Meyer, O.; Bischoff-Ferrari, H.A.; Keller, D.I. Prediction of Emergency Department Re-Visits in Older Patients by the Identification of Senior at Risk (ISAR) Screening. Geriatrics 2018, 3, 33. [Google Scholar] [CrossRef] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Moore, Z.E.; Patton, D. Risk assessment tools for the prevention of pressure ulcers. Cochrane Database Syst. Rev. 2019, 1, CD006471. [Google Scholar] [CrossRef] [PubMed]
- Droz, J.P.; Albrand, G.; Gillessen, S.; Hughes, S.; Mottet, N.; Oudard, S.; Payne, H.; Puts, M.; Zulian, G.; Balducci, L.; et al. Management of Prostate Cancer in Elderly Patients: Recommendations of a Task Force of the International Society of Geriatric Oncology. Eur. Urol. 2017, 72, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Tapia, C.; Paillaud, E.; Liuu, E.; Tournigand, C.; Ibrahim, R.; Fossey-Diaz, V.; Culine, S.; Canoui-Poitrine, F.; Audureau, E.; Group, E.S. Prognostic value of the G8 and modified-G8 screening tools for multidimensional health problems in older patients with cancer. Eur. J. Cancer 2017, 83, 211–219. [Google Scholar] [CrossRef]
- Droz, J.P.; Aapro, M.; Balducci, L.; Boyle, H.; Van den Broeck, T.; Cathcart, P.; Dickinson, L.; Efstathiou, E.; Emberton, M.; Fitzpatrick, J.M.; et al. Management of prostate cancer in older patients: Updated recommendations of a working group of the International Society of Geriatric Oncology. Lancet Oncol. 2014, 15, e404–e414. [Google Scholar] [CrossRef]
| All | |
|---|---|
| Patients (m/f), (n = pat.) | 100 (78/22) |
| Age, (y, min–max) | 83.25 (75–101) |
| malignancy, (n = pat.) | 56 |
| benign disease, (n = pat.) | 44 |
| prostate cancer | 24 |
| urothelial cancer | 28 |
| renal cancer | 4 |
| urolithiasis | 4 |
| benign subvesical obstruction | 21 |
| urinary tract infections | 9 |
| upper urinary tract retention | 4 |
| hematuria | 6 |
| Results | |
| G 8 score (mean (min–max)) | 12.9 (4–17) |
| ISAR score (mean (min–max)) | 1.6 (0–6) |
| Charlson comorbidity score (mean (min–max)) | 3.1 (0–7) |
| length of hospital stay, (n = d), (mean (min–max)) | 7.9 (1–24) |
| number of coded diagnosis, (mean (min–max)) | 9.5, (2–32) |
| Braden score, (mean (min–max)) | 18.25 (9–23) |
| G8 Score | ISAR Score | Age | Charlson Comorbidity Index | Length of Stay (d) | Number of Coded Diagnosis | Braden Score | ||
|---|---|---|---|---|---|---|---|---|
| G8 score | Correlation coefficient, Spearman | 1 | −0.773 | −0.599 | −0.368 | −0.337 | −0.418 | 0.278 |
| p-value | 0.000 | 0.000 | 0.000 | 0.001 | 0.000 | 0.005 | ||
| ISAR score | Correlation coefficient, Spearman | −0.773 | 1 | 0.393 | 0.341 | 0.218 | 0.487 | −0.264 |
| p-value | 0.000 | 0.000 | 0.001 | 0.029 | 0.000 | 0.008 |
| 1. Pat. with Negative G8 Scores (n = 42 pat.) | 2. Pat. with Negative ISAR Scores (n = 76 pat.) | 3. Pat. with Positive G8 and Negative ISAR Scores (n = 34 pat.) | 4. Pat. with Positive G8 Scores (n = 58 pat.) | 5. Pat. with Positive ISAR Scores (n = 24 pat.) | p-Values | |
|---|---|---|---|---|---|---|
| G8 score (mean values) | 15.6 | 14.1 | 12.4 | 11.0 | 9.0 | p < 0.001 |
| ISAR score (mean values) | 0.4 | 0.8 | 1.3 | 2.4 | 4.0 | p < 0.001 |
| Charlson comorbidity Index (mean values) | 2.40 | 2.94 | 3.61 | 3.65 | 3.70 | p < 0.003 |
| Length of stay, days (mean values) | 6.14 | 7.38 | 8.91 | 9.20 | 9.62 | p < 0.001 |
| Number of coded diagnosis (mean values) | 6.73 | 8.23 | 10.08 | 11.46 | 13.41 | p < 0.001 |
| Braden score (mean values) | 19.42 | 18.88 | 18.20 | 17.39 | 16.25 | p < 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bouzan, J.; Stoilkov, B.; Nellas, S.; Horstmann, M. Comparison of G8 and ISAR Screening Results in Geriatric Urology. Medicines 2021, 8, 40. https://doi.org/10.3390/medicines8080040
Bouzan J, Stoilkov B, Nellas S, Horstmann M. Comparison of G8 and ISAR Screening Results in Geriatric Urology. Medicines. 2021; 8(8):40. https://doi.org/10.3390/medicines8080040
Chicago/Turabian StyleBouzan, Jobar, Boris Stoilkov, Spyridon Nellas, and Marcus Horstmann. 2021. "Comparison of G8 and ISAR Screening Results in Geriatric Urology" Medicines 8, no. 8: 40. https://doi.org/10.3390/medicines8080040
APA StyleBouzan, J., Stoilkov, B., Nellas, S., & Horstmann, M. (2021). Comparison of G8 and ISAR Screening Results in Geriatric Urology. Medicines, 8(8), 40. https://doi.org/10.3390/medicines8080040






