Magnetic Resonance Imaging of the Cervical Spine: Frequency of Abnormal Findings with Relation to Age
Abstract
:1. Introduction
2. Methods
2.1. Patients
2.2. Ethical Approval
2.3. Statistical Analysis
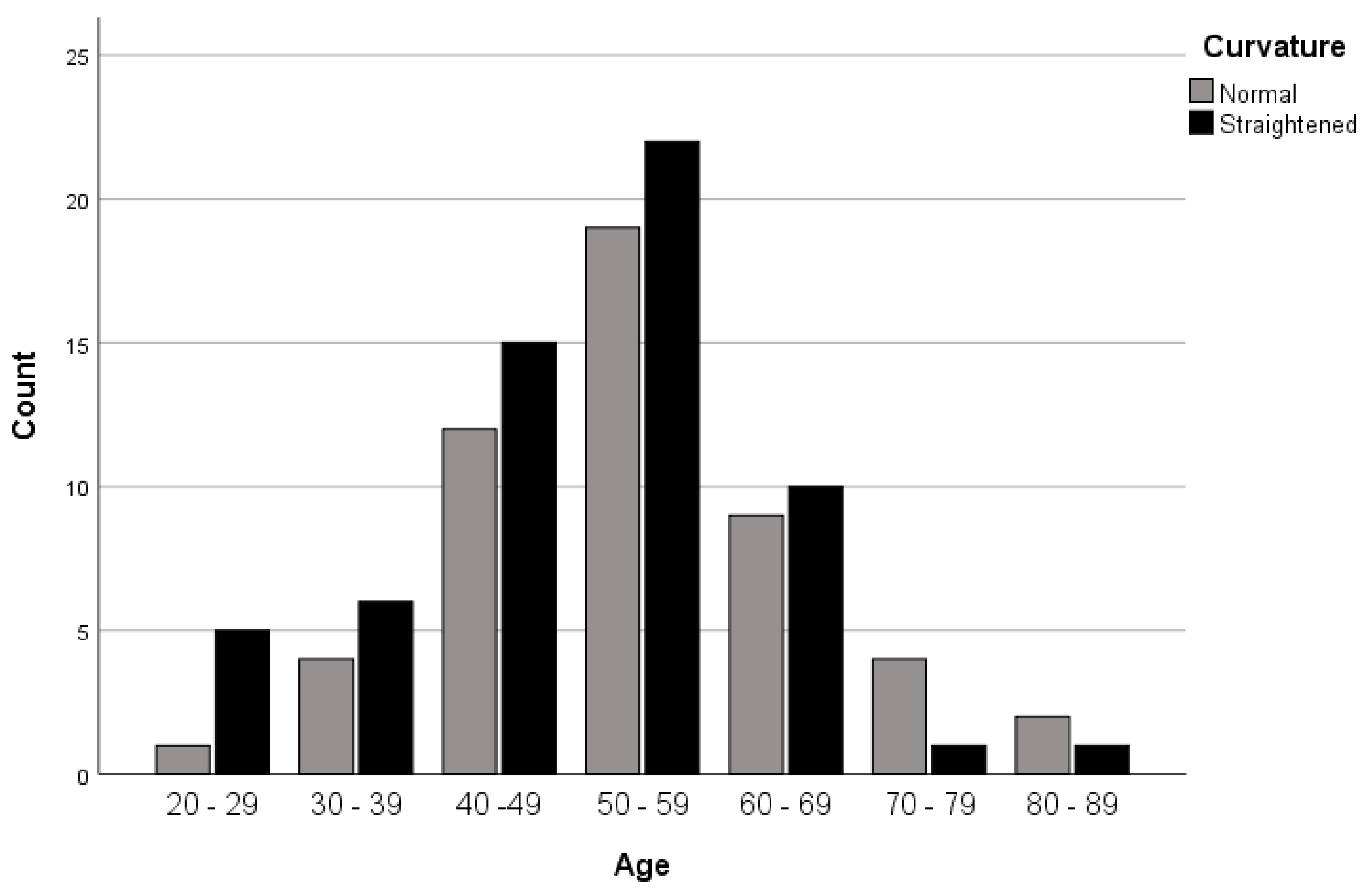
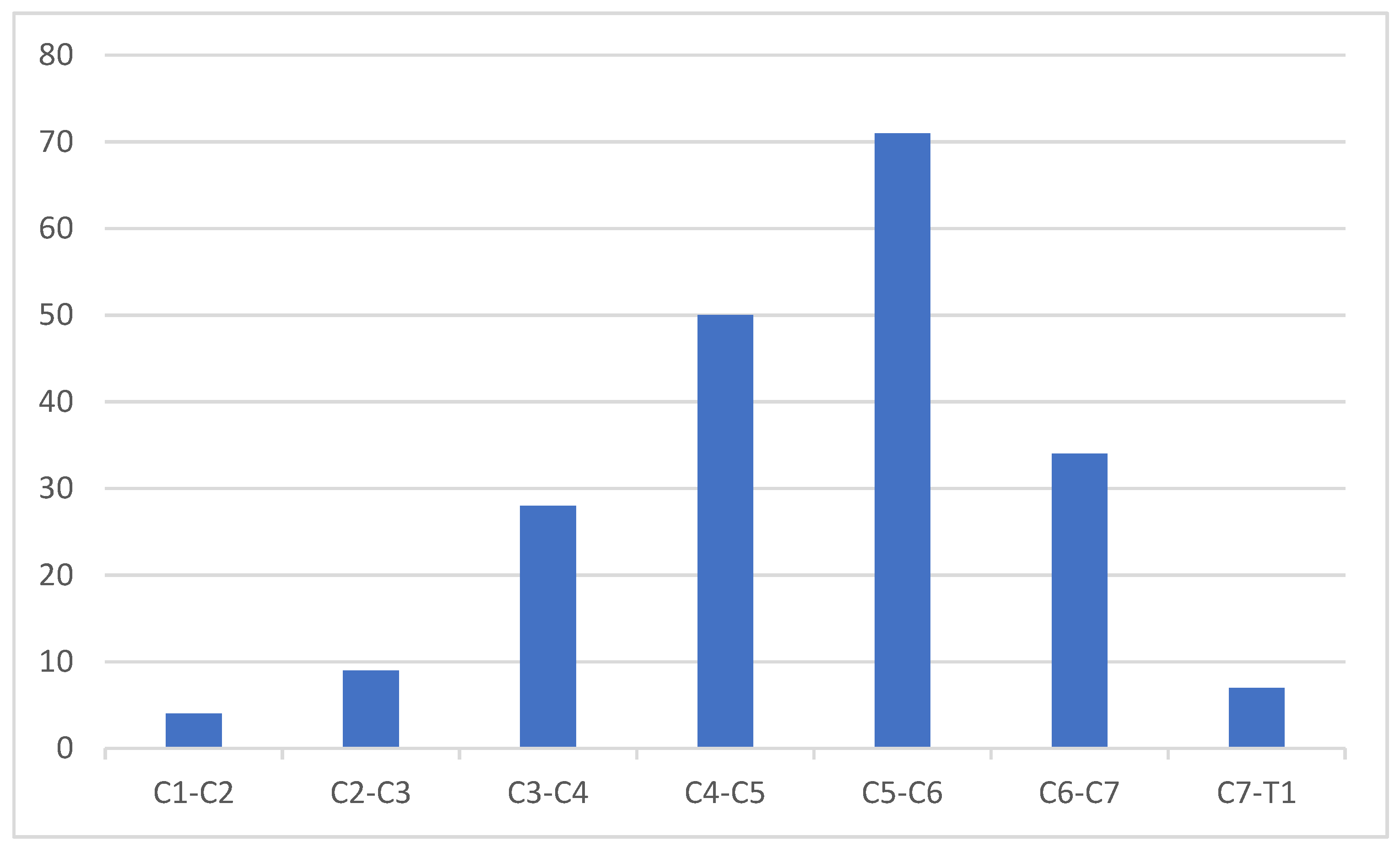
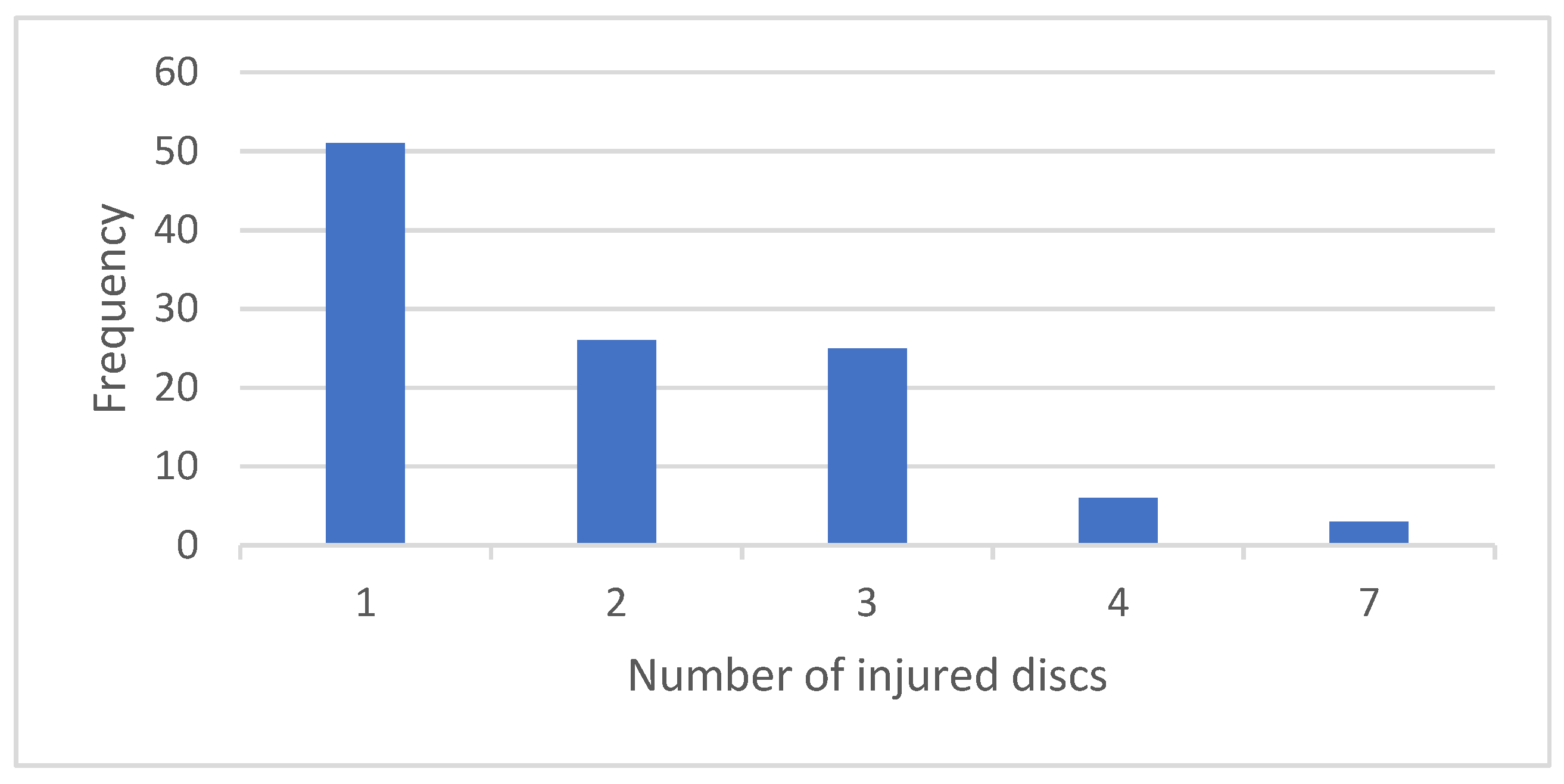
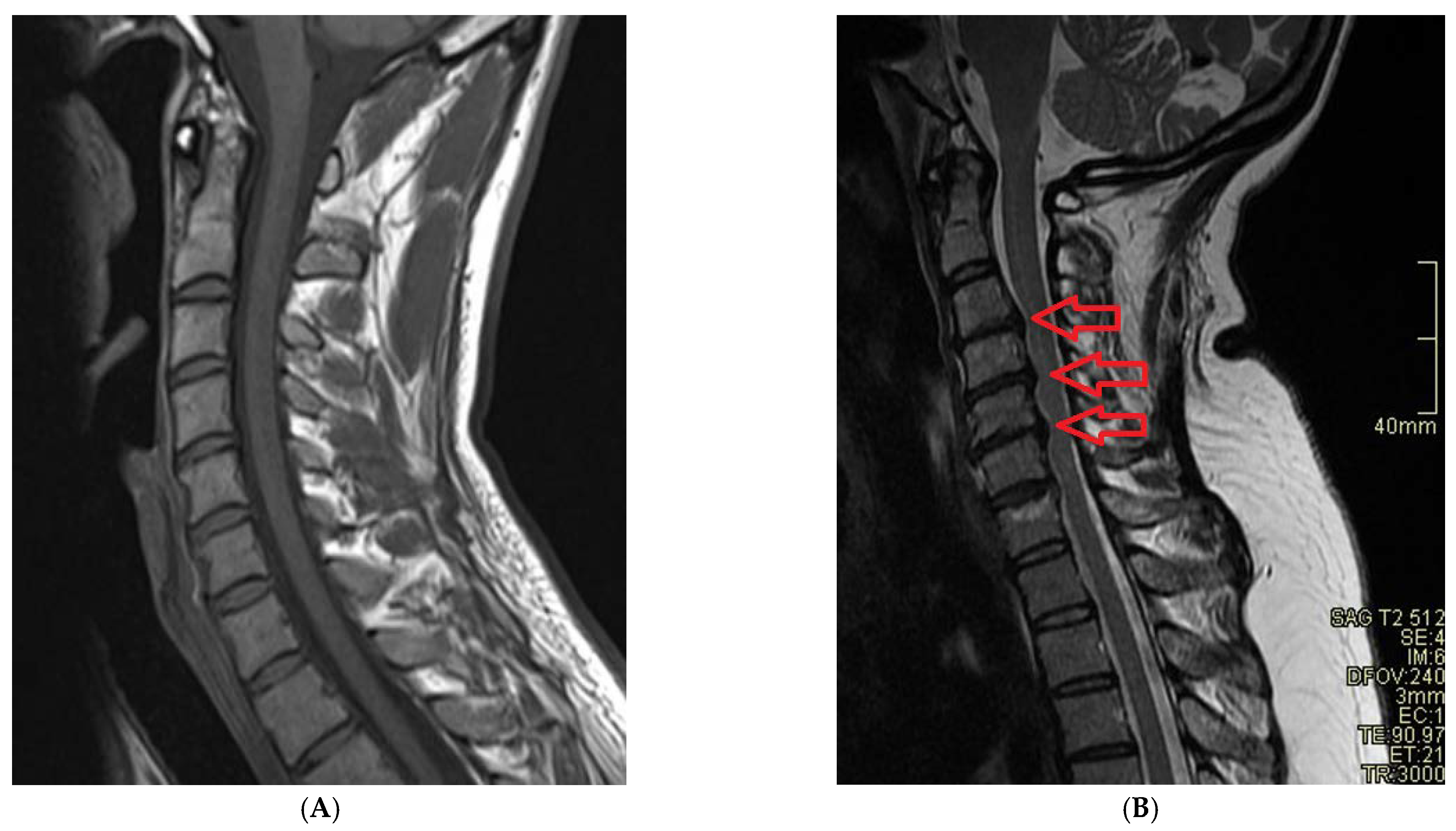
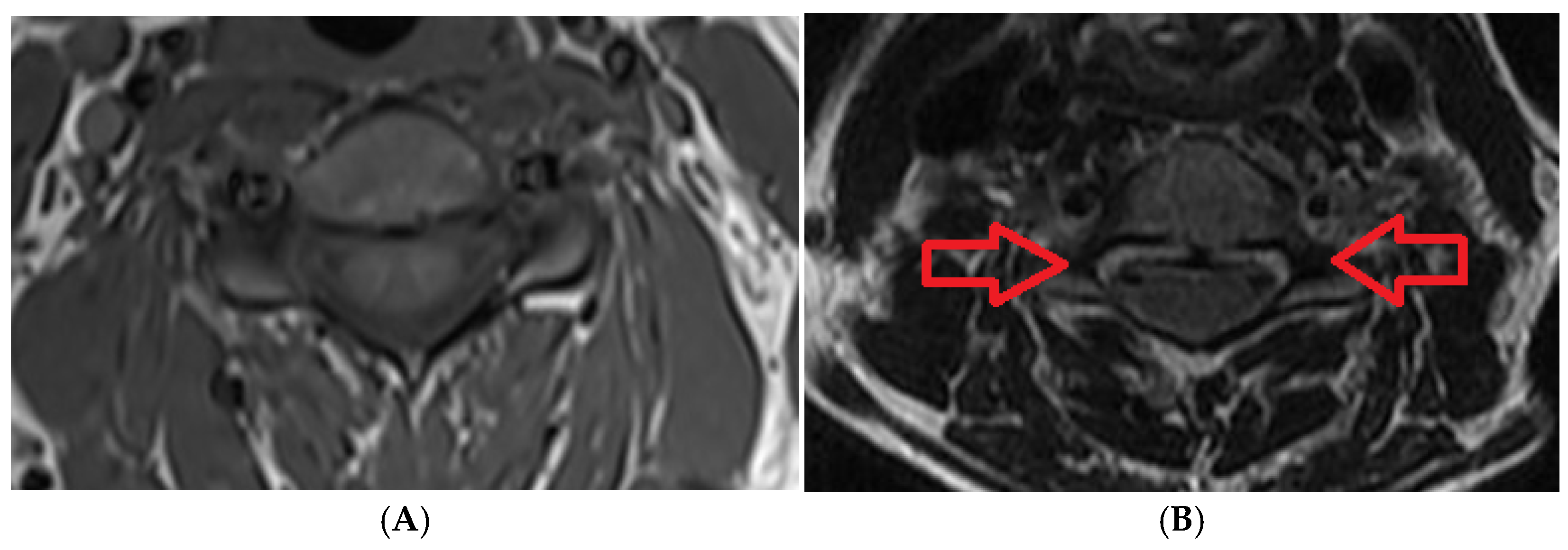
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Liu, C.Y.; Zygourakis, C.C.; Yoon, S.; Kliot, T.; Moriates, C.; Ratliff, J.; Dudley, R.A.; Gonzales, R.; Mummaneni, P.V.; Ames, C.P. Trends in Utilization and Cost of Cervical Spine Surgery Using the National Inpatient Sample Database, 2001 to 2013. Spine 2017, 42, E906–E913. [Google Scholar] [CrossRef]
- Asemota, A.O.; Ahmed, A.K.; Purvis, T.E.; Passias, P.G.; Goodwin, C.R.; Sciubba, D.M. Analysis of Cervical Spine Injuries in Elderly Patients from 2001 to 2010 Using a Nationwide Database: Increasing Incidence, Overall Mortality, and Inpatient Hospital Charges. World Neurosurg. 2018, 120, e114–e130. [Google Scholar] [CrossRef]
- Deckey, D.G.; Makovicka, J.L.; Chung, A.S.; Hassebrock, J.D.; Patel, K.A.; Tummala, S.V.; Chhabra, A. Neck and cervical spine injuries in National College Athletic Association athletes: A 5-year epidemiologic study. Spine 2020, 45, 55–64. [Google Scholar] [CrossRef]
- Zaveri, G.; Das, G. Management of sub-axial cervical spine injuries. Indian J. Orthop. 2017, 51, 633–652. [Google Scholar] [CrossRef]
- Meron, A.; McMullen, C.; Laker, S.R.; Currie, D.; Comstock, R.D. Epidemiology of cervical spine injuries in high school athletes over a ten-year period. PM&R 2018, 10, 365–372. [Google Scholar]
- Bokhari, A.R.; Sivakumar, B.; Sefton, A.; Lin, J.; Smith, M.M.; Gray, R.; Hartin, N. Morbidity and mortality in cervical spine injuries in the elderly. ANZ J. Surg. 2018, 89, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Cazzola, D.; Holsgrove, T.; Preatoni, E.; Gill, H.; Trewartha, G. Cervical Spine Injuries: A Whole-Body Musculoskeletal Model for the Analysis of Spinal Loading. PLoS ONE 2017, 12, e0169329. [Google Scholar] [CrossRef]
- Page, P.S.; Wei, Z.; Brooks, N.P. Motorcycle helmets and cervical spine injuries: A 5-year experience at a Level 1 trauma center. J. Neurosurg. Spine 2018, 28, 607–611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kato, F.; Yukawa, Y.; Suda, K.; Yamagata, M.; Ueta, T. Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: Magnetic resonance imaging of over 1,200 asymptomatic subjects. Eur. Spine J. 2012, 21, 1499–1507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, E.; Matsumoto, M.; Ichihara, D.; Chiba, K.; Toyama, Y.; Fujiwara, H.; Momoshima, S.; Nishiwaki, Y.; Hashimoto, T.; Ogawa, J.; et al. Does the sagittal alignment of the cervical spine have an impact on disk degeneration? Minimum 10-year follow-up of asymptomatic volunteers. Eur. Spine J. 2009, 18, 1644–1651. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vale, F.L.; Burns, J.; Jackson, A.B.; Hadley, M.N. Combined medical and surgical treatment after acute spinal cord injury: Results of a prospective pilot study to assess the merits of aggressive medical resuscitation and blood pressure management. J. Neurosurg. 1997, 87, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Aarabi, B.; Olexa, J.; Chryssikos, T.; Galvagno, S.M.; Hersh, D.; Wessell, A.; Sansur, C.; Schwartzbauer, G.; Crandall, K.; Shanmuganathan, K.; et al. Extent of Spinal Cord Decompression in Motor Complete (American Spinal Injury Association Impairment Scale Grades A and B) Traumatic Spinal Cord Injury Patients: Post-Operative Magnetic Resonance Imaging Analysis of Standard Operative Approaches. J. Neurotrauma 2019, 36, 862–876. [Google Scholar] [CrossRef]
- Jain, N.B.; Ayers, G.D.; Peterson, E.N.; Harris, M.B.; Morse, L.; O’Connor, K.C.; Garshick, E. Traumatic spinal cord injury in the United States, 1993–2012. JAMA 2015, 313, 2236–2243. [Google Scholar] [CrossRef]
- Kumagai, G.; Ono, A.; Numasawa, T.; Wada, K.; Inoue, R.; Iwasaki, H.; Ishibashi, Y.; Iwane, K.; Matsuzaka, M.; Takahashi, I.; et al. Association between roentgenographic findings of the cervical spine and neck symptoms in a Japanese community population. J. Orthop. Sci. 2014, 19, 390–397. [Google Scholar] [CrossRef] [Green Version]
- Swinnen, T.W.; Westhovens, R.; Dankaerts, W.; De Vlam, K. Widespread pain in axial spondyloarthritis: Clinical importance and gender differences. Arthritis Res. 2018, 20, 156. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Liu, P.; Ma, Z.; Mou, J.; Wang, Z.; Sun, D.; Cheng, J.; Zhang, D.; Xiao, J. The effects of aging on the profile of the cervical spine. Medicine 2019, 98, e14425. [Google Scholar] [CrossRef]
- Cote, P.; Cassidy, J.D.; Yong-Hing, K.; Sibley, J.; Loewy, J. Apophysial joint degeneration, disc degeneration, and sagittal curve of the cervical spine. Can they be measured reliably on radiographs? Spine 1997, 22, 859–864. [Google Scholar] [CrossRef]
- Gore, D.R.; Sepic, S.B.; Gardner, G.M. Roentgenographic Findings of the Cervical Spine in Asymptomatic People. Spine 1986, 11, 521–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fehlings, M.G.; Singh, A.; Tetreault, L.; Kalsi-Ryan, S.; Nouri, A. Global prevalence and incidence of traumatic spinal cord injury. Clin. Epidemiol. 2014, 6, 309–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, E.; Matsumoto, M.; Fujiwara, H.; Toyama, Y. Disc degeneration of cervical spine on MRI in patients with lumbar disc herniation: Comparison study with asymptomatic volunteers. Eur. Spine J. 2010, 20, 585–591. [Google Scholar] [CrossRef] [Green Version]
- Siivola, S.M.; Levoska, S.; Tervonen, O.; Ilkko, E.; Vanharanta, H.; Keinänen-Kiukaanniemi, S. MRI changes of cervical spine in asymptomatic and symptomatic young adults. Eur. Spine J. 2002, 11, 358–363. [Google Scholar] [CrossRef] [Green Version]
- Matsumoto, M.; Okada, E.; Ichihara, D.; Watanabe, K.; Chiba, K.; Toyama, Y.; Fujiwara, H.; Momoshima, S.; Nishiwaki, Y.; Hashimoto, T.; et al. Age-Related Changes of Thoracic and Cervical Intervertebral Discs in Asymptomatic Subjects. Spine 2010, 35, 1359–1364. [Google Scholar] [CrossRef]
- Boden, S.D.; McCowin, P.R.; Davis, D.O.; Dina, T.S.; Mark, A.S.; Wiesel, S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J. Bone Jt. Surg.-Am. Vol. 1990, 72, 1178–1184. [Google Scholar] [CrossRef]
- Schellhas, K.P.; Smith, M.D.; Gundry, C.R.; Pollei, S.R. Cervical discogenic pain: Prospective correlation of magnetic resonance imaging and discography in asymptomatic subjects and pain sufferers. Spine 1996, 21, 300–311. [Google Scholar] [CrossRef]
- Aarabi, B.; Simard, J.M.; Kufera, J.A.; Alexander, M.; Zacherl, K.M.; Mirvis, S.E.; Shanmuganathan, K.; Schwartzbauer, G.; Maulucci, C.; Slavin, J.; et al. Intramedullary lesion expansion on magnetic resonance imaging in patients with motor complete cervical spinal cord injury. J. Neurosurg. Spine 2012, 17, 243–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simard, J.M.; Woo, S.K.; Norenberg, M.D.; Tosun, C.; Chen, Z.; Ivanova, S.; Tsymbalyuk, O.; Bryan, J.; Landsman, D.; Gerzanich, V. Brief Suppression of Abcc8 Prevents Autodestruction of Spinal Cord after Trauma. Sci. Transl. Med. 2010, 2, 28ra29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aarabi, B.; Albrecht, J.S.; Simard, J.M.; Chryssikos, T.; Schwartzbauer, G.; Sansur, C.A.; Crandall, K.; Gertner, M.; Howie, B.; Wessell, A.; et al. Trends in Demographics and Markers of Injury Severity in Traumatic Cervical Spinal Cord Injury. J. Neurotrauma 2021, 38, 756–764. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; He, Y.; DeVivo, M.J. Changing Demographics and Injury Profile of New Traumatic Spinal Cord Injuries in the United States, 1972–2014. Arch. Phys. Med. Rehabil. 2016, 97, 1610–1619. [Google Scholar] [CrossRef] [PubMed]
- McCaughey, E.J.; Purcell, M.; McLean, A.N.; Fraser, M.H.; Bewick, A.; Borotkanics, R.J.; Allan, D.B. Changing demographics of spinal cord injury over a 20-year period: A longitudinal population-based study in Scotland. Spinal Cord 2015, 54, 270–276. [Google Scholar] [CrossRef] [Green Version]
- Friedenberg, Z.B.; Miller, W.T. Degenerative Disc Disease Of The Cervical Spine. J. Bone Jt. Surg. Am. 1963, 45, 1171–1178. [Google Scholar] [CrossRef]
- Wang, X.-R.; Kwok, T.C.Y.; Griffith, J.F.; Yu, B.W.M.; Leung, J.C.S.; Wáng, Y.X.J. Prevalence of cervical spine degenerative changes in elderly population and its weak association with aging, neck pain, and osteoporosis. Ann. Transl. Med. 2019, 7, 486. [Google Scholar] [CrossRef]
- Yokoyama, K.; Kawanishi, M.; Yamada, M.; Tanaka, H.; Ito, Y.; Kawabata, S.; Kuroiwa, T. Age-related variations in global spinal alignment and sagittal balance in asymptomatic Japanese adults. Neurol. Res. 2017, 39, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Luo, J.; Pan, Z.; Zhiyun, L.; Pang, L.; Zhong, J.; Li, Z.; Cao, K. The change of cervical spine alignment along with aging in asymptomatic population: A preliminary analysis. Eur. Spine J. 2017, 26, 2363–2371. [Google Scholar] [CrossRef] [PubMed]
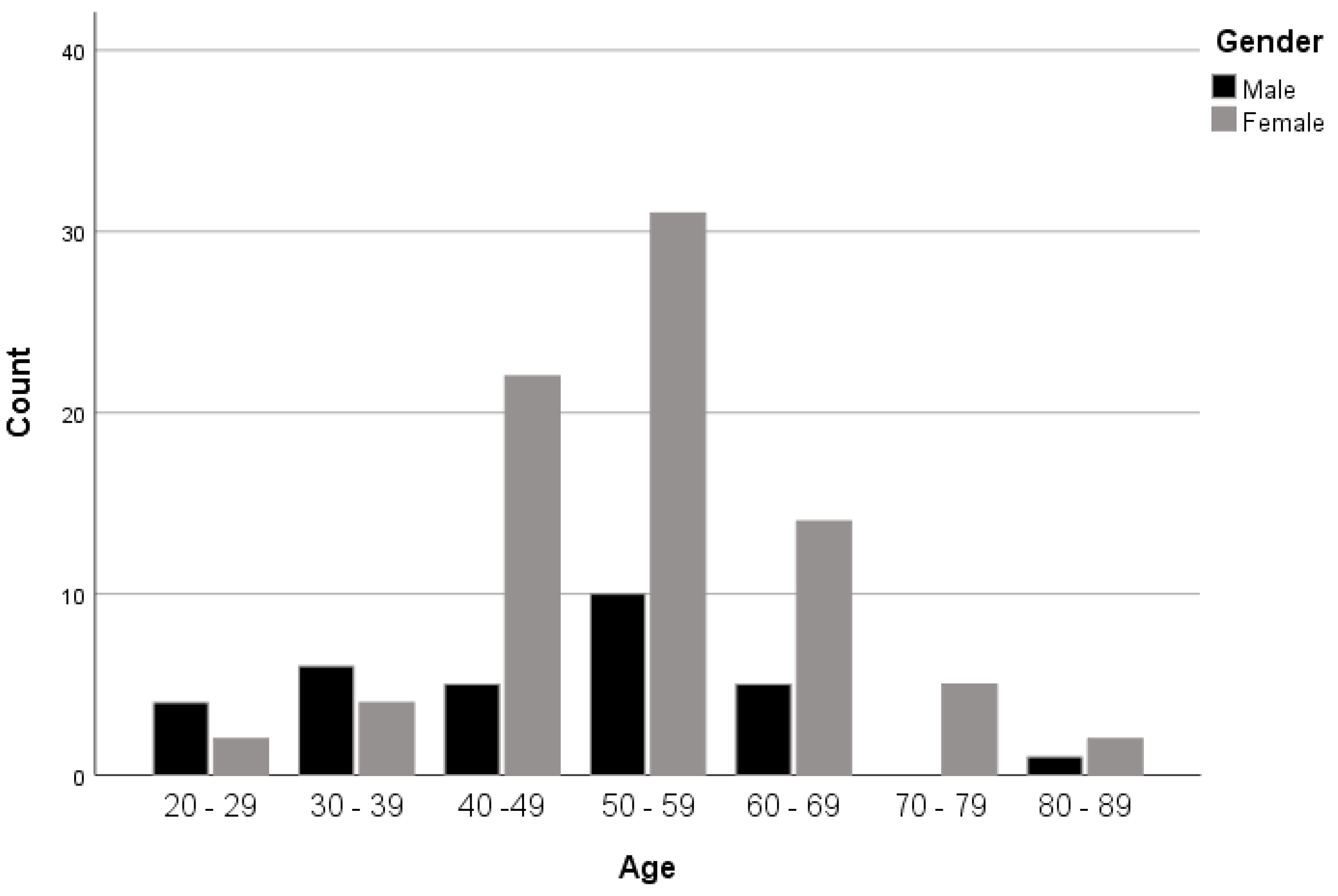
| Gender | Total | ||||
|---|---|---|---|---|---|
| Male | Female | ||||
| Age | 20–29 | Count | 4 | 2 | 6 |
| % within age | 66.7% | 33.3% | 100.0% | ||
| 30–39 | Count | 6 | 4 | 10 | |
| % within age | 60.0% | 40.0% | 100.0% | ||
| 40–49 | Count | 5 | 22 | 27 | |
| % within age | 18.5% | 81.5% | 100.0% | ||
| 50–59 | Count | 10 | 31 | 41 | |
| % within age | 24.4% | 75.6% | 100.0% | ||
| 60–69 | Count | 5 | 14 | 19 | |
| % within age | 26.3% | 73.7% | 100.0% | ||
| 70–79 | Count | 0 | 5 | 5 | |
| % within age | 0.0% | 100.0% | 100.0% | ||
| 80–89 | Count | 1 | 2 | 3 | |
| % within age | 33.3% | 66.7% | 100.0% | ||
| Total | Count | 31 | 80 | 111 | |
| % within age | 27.9% | 72.1% | 100.0% | ||
| Number | Percentage % | |
|---|---|---|
| Disc protrusions | 28 | 25.2 |
| Disc bulge | 13 | 11.7 |
| Mild spondylodegenerative changes | 58 | 52.3 |
| Disc osteophytic complexes | 10 | 9 |
| Burst fracture | 2 | 1.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alghamdi, A.; Alqahtani, A. Magnetic Resonance Imaging of the Cervical Spine: Frequency of Abnormal Findings with Relation to Age. Medicines 2021, 8, 77. https://doi.org/10.3390/medicines8120077
Alghamdi A, Alqahtani A. Magnetic Resonance Imaging of the Cervical Spine: Frequency of Abnormal Findings with Relation to Age. Medicines. 2021; 8(12):77. https://doi.org/10.3390/medicines8120077
Chicago/Turabian StyleAlghamdi, Ali, and Abeer Alqahtani. 2021. "Magnetic Resonance Imaging of the Cervical Spine: Frequency of Abnormal Findings with Relation to Age" Medicines 8, no. 12: 77. https://doi.org/10.3390/medicines8120077
APA StyleAlghamdi, A., & Alqahtani, A. (2021). Magnetic Resonance Imaging of the Cervical Spine: Frequency of Abnormal Findings with Relation to Age. Medicines, 8(12), 77. https://doi.org/10.3390/medicines8120077






