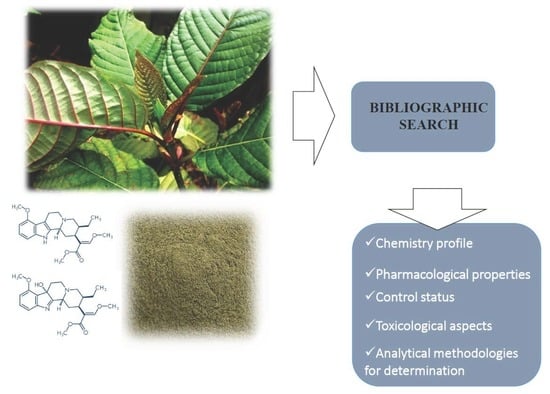
Mitragyna speciosa: Clinical, Toxicological Aspects and Analysis in Biological and Non-Biological Samples
Abstract
1. Introduction
2. Research Methodology
3. Toxicokinetics and Pharmacodynamics
4. Clinical Effects/Pharmacology
4.1. Analgesic Properties
4.2. Anti-Inflammatory Properties
4.3. Gastrointestinal Effects
4.4. Anti-Depressant Activity
4.5. Antioxidant and Anti-Bacterial Properties
5. Toxicology
6. Case Reports
7. Analytical Methodologies
8. Conclusions and Future Perspective
Author Contributions
Funding
Conflicts of Interest
References
- Dennehy, C.E.; Tsourounis, C.; Miller, A.E. Evaluation of Herbal Dietary Supplements Marketed on the Internet for Recreational Use. Complement. Altern. Med. 2014, 39, 1634–1639. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Müller, C.P.; Vicknasingam, B.K. Kratom (Mitragyna speciosa) dependence, withdrawal symptoms and craving in regular users. Drug Alcohol Depend. 2014, 139, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Müller, C.P.; Vicknasingam, B.K.; Mansor, S.M. Social Functioning of Kratom (Mitragyna speciosa) Users in Malaysia. J. Psychoact. Drugs 2015, 47, 125–131. [Google Scholar] [CrossRef] [PubMed]
- European Monitoring Centre for Drugs and Drug Adiction. New Psychoactive Substances in Europe. Available online: http://www.emcdda.europa.eu/system/files/publications/65/TD0415135ENN.pdf (accessed on 12 January 2019).
- Adkins, J.E.; Boyer, E.W.; Mccurdy, C.R. Mitragyna speciosa, A Psychoactive Tree from Southeast Asia with Opioid Activity. Curr. Top. Med. Chem. 2011, 11, 1165–1175. [Google Scholar] [CrossRef] [PubMed]
- Takayama, H. Chemistry and Pharmacology of Analgesic Indole Alkaloids from the Rubiaceous Plant, Mitragyna speciosa. Chem. Pharm. Bull. 2004, 52, 916–928. [Google Scholar] [CrossRef] [PubMed]
- Gong, F.; Gu, H.; Xu, Q.; Kang, W. Genus Mitragyna: Ethnomedicinal uses and pharmacological studies. Phytopharmacology 2012, 3, 263–272. [Google Scholar]
- Davis, G.G. Drug abuse: Newly-Emerging drugs and trends. Clin. Lab. Med. 2012, 32, 407–417. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, T.; Kawamura, M.; Kikura-Hanajiri, R.; Takayama, H.; Goda, Y. The botanical origin of kratom (Mitragyna speciosa; Rubiaceae) available as abused drugs in the Japanese markets. J. Nat. Med. 2009, 63, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Tanguay, P. Kratom in Thailand. Transl. Inst. Legis. Reform Drug Policies 2011, 13, 1–16. [Google Scholar] [CrossRef]
- Saingam, D.; Assanangkornchai, S.; Geater, A.F.; Balthip, Q. Pattern and consequences of krathom (Mitragyna speciosa Korth.) use among male villagers in southern Thailand: A qualitative study. Int. J. Drug Policy 2018, 24, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Narayanan, S.; Vicknasingam, B. Traditional and non-traditional uses of Mitragynine (Kratom): A survey of the literature. Brain Res. Bull. 2016, 126, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Vicknasingam, B.; Narayanan, S.; Beng, G.T.; Mansor, S.M. The informal use of ketum (Mitragyna speciosa) for opioid withdrawal in the northern states of peninsular Malaysia and implications for drug substitution therapy. Int. J. Drug Policy 2010, 21, 283–288. [Google Scholar] [CrossRef] [PubMed]
- Swogger, M.T.; Hart, E.; Erowid, F.; Erowid, E.; Trabold, N.; Yee, K.; Parkhurst, K.A.; Priddy, B.M.; Walsh, Z. Experiences of Kratom Users: A Qualitative Analysis. J. Psychoact. Drugs 2015, 47, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Assanangkornchai, S.; Muekthong, A. The Use of Mitragynine speciosa (“Krathom”), an Addictive Plant, in Thailand. Subst. Use Misuse 2006, 6084, 2145–2157. [Google Scholar]
- Grundmann, O. Patterns of Kratom use and health impact in the US—Results from an online survey. Drug Alcohol Depend. 2017, 176, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.M.; Sharma, A.; Schifano, F.; Feinmann, C. “Legal highs” on the net-Evaluation of UK-based Websites, products and product information. Forensic Sci. Int. 2011, 206, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Hillebrand, J.; Olszewski, D.; Sedefov, R. Legal Highs on the Internet. Subst. Use Misuse 2010, 45, 330–340. [Google Scholar] [CrossRef] [PubMed]
- European Monitoring Centre for Drugs and Drug Adiction. Khat Drug Profile. Available online: http://www.emcdda.europa.eu/publications/drug-profiles/khat (accessed on 11 January 2019).
- United Nations Office on Drugs and Crime (UNODC). UNODC Early Warning Advisory (EWA) on New Psychoactive Substances (NPS). Available online: https://www.unodc.org/LSS/Home/NPS (accessed on 16 January 2019).
- Kratom (Mitragyna speciosa) Drug Profile. Available online: http://www.emcdda.europa.eu/publications/drug-profiles/kratom (accessed on 11 January 2019).
- Ahmad, K.; Aziz, Z. Mitragyna speciosa use in the northern states of Malaysia: A cross-sectional study. J. Ethnopharmacol. 2012, 141, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Jansen, K.; Prast, C. Ethnopharmacology of kratom and mitragyna alkaloids. J. Ethnopharmacol. 1988, 23, 115–119. [Google Scholar] [CrossRef]
- Shellard, E.J. Ethnopharmacology of kratom and the Mitragyna alkaloids. J. Ethnopharmacol. 1989, 25, 123–124. [Google Scholar] [CrossRef]
- Feng, L.-Y.; Battulga, A.; Han, E.; Chung, H.; Li, J.-H. New psychoactive substances of natural origin: A brief review. J. Food Drug Anal. 2017, 25, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Raffa, R.B. Kratom and Other Mitragynines: The Chemistry and Pharmacology of Opioids from a Non-Opium Source, 1st ed.; Raffa, R.B., Ed.; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Schro, S.; Stu, B.; Arndt, T.; Claussen, U.; Gu, B.; Werle, A.; Wolf, G. Kratom alkaloids and O-desmethyltramadol in urine of a “Krypton” herbal mixture consumer. Forensic Sci. Int. 2011, 208, 47–52. [Google Scholar]
- Ponglux, D.; Wongseripipatana, S.; Takayama, H.; Kilcuchi, M.; Kurihara, M. A New Indole Alkaloid, 7a-Hydroxy-7H-mitragynine, from Mitragyna speciosa in Thailand. Planta Med. 1994, 60, 581–582. [Google Scholar] [CrossRef] [PubMed]
- Prozialeck, W.C.; Jivan, J.K.; Andurkar, S.V. Pharmacology of Kratom: An Emerging Botanical Agent with Stimulant, Analgesic and Opioid-Like Effects. J. Am. Osteopath. Assoc. 2012, 112, 792–799. [Google Scholar] [PubMed]
- Hendrickson, J.B.; Sims, J.J. Mitragyna alkaloids: The structure of stipulatine. Tetrahedron Lett. 1963, 4, 929–935. [Google Scholar] [CrossRef]
- Veeramohan, R.; Azizan, K.A.; Aizat, W.M.; Goh, H.-H.; Mansor, S.M.; Yusof, N.S.M.; Baharum, S.N.; Ng, C.L. Metabolomics data of Mitragyna speciosa leaf using LC-ESI-TOF-MS. Data Br. 2018, 18, 1212–1216. [Google Scholar] [CrossRef] [PubMed]
- Lesiak, A.D.; Cody, R.B.; Dane, A.J.; Musah, R.A. Rapid detection by direct analysis in real time-mass spectrometry (DART-MS) of psychoactive plant drugs of abuse: The case of Mitragyna speciosa aka “Kratom”. Forensic Sci. Int. 2014, 242, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, S.; Ramanathan, S.; Ismail, S.; Adenan, M.I.; Mansor, S.M.; Murugaiyah, V. Determination of mitragynine in plasma with solid-phase extraction and rapid HPLC-UV analysis, and its application to a pharmacokinetic study in rat. Anal. Bioanal. Chem. 2010, 397, 2023–2030. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, S.; Parthasarathy, S.; Murugaiyah, V.; Magosso, E.; Tan, S.C.; Mansor, S.M. Understanding the physicochemical properties of mitragynine, a principal alkaloid of Mitragyna speciosa, for preclinical evaluation. Molecules 2015, 20, 4915–4927. [Google Scholar] [CrossRef] [PubMed]
- Manda, V.K.; Avula, B.; Ali, Z.; Khan, I.A.; Walker, L.A.; Khan, S.I. Evaluation of in vitro absorption, distribution, metabolism, and excretion (ADME) properties of mitragynine, 7-hydroxymitragynine, and mitraphylline. Planta Med. 2014, 80, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Trakulsrichai, S.; Sathirakul, K.; Auparakkitanon, S.; Krongvorakul, J.; Sueajai, J.; Noumjad, N.; Sukasem, C.; Wananukul, W. Pharmacokinetics of mitragynine in man. Drug Des. Dev. Ther. 2015, 9, 2421–2429. [Google Scholar]
- Boyer, E.; Babu, K.; Adkins, J.; McCurdy, C.; Harpern, J. Self-treatment of opioid withdrawal using kratom (Mitragynia speciosa Korth). Addiction 2013, 103, 1048–1050. [Google Scholar] [CrossRef] [PubMed]
- Avery, B.A.; Boddu, S.P.; Sharma, A.; Furr, E.B.; Leon, F.; Cutler, S.J.; McCurdy, C.R. Comparative Pharmacokinetics of Mitragynine after Oral Administration of Mitragyna speciosa (Kratom) Leaf Extracts in Rats. Planta Med. 2018, in press. [Google Scholar] [CrossRef] [PubMed]
- Yusof, S.R.; Mohd Uzid, M.; Teh, E.-H.; Hanapi, N.A.; Mohideen, M.; Mohamad Arshad, A.S.; Mordi, M.N.; Loryan, I.; Hammarlund-Udenaes, M. Rate and extent of mitragynine and 7-hydroxymitragynine blood–brain barrier transport and their intra-brain distribution: The missing link in pharmacodynamic studies. Addict. Biol. 2018, in press. [Google Scholar] [CrossRef] [PubMed]
- Azizi, J.; Ismail, S.; Mansor, S.M. Mitragyna speciosa Korth leaves extracts induced the CYP450 catalyzed aminopyrine-N-demethylase (APND) and UDP-glucuronosyl transferase (UGT) activities in male Sprague-Dawley rat livers. Drug Metab. Drug Interact. 2013, 28, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.M.; Chik, Z.; Ramachandra, M.; Subramaniam, U.; Raja Aziddin, R.E.; Mohamed, Z. Evaluation of the effects of Mitragyna speciosa alkaloid extract on cytochrome P450 enzymes using a high throughput assay. Molecules 2011, 16, 7344–7356. [Google Scholar] [CrossRef] [PubMed]
- Kamble, S.H.; Sharma, A.; King, T.I.; León, F.; McCurdy, C.R.; Avery, B.A. Metabolite profiling and identification of enzymes responsible for the metabolism of mitragynine, the major alkaloid of Mitragyna speciosa (kratom). Xenobiotica 2018, 14, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Uno, Y.; Uehara, S.; Murayama, N.; Yamazaki, H. Cytochrome P450 1A1, 2C9, 2C19, and 3A4 Polymorphisms Account for Interindividual Variability of Toxicological Drug Metabolism in Cynomolgus Macaques. Chem. Res. Toxicol. 2018, 31, 1373–1381. [Google Scholar] [CrossRef] [PubMed]
- Philipp, A.A.; Wissenbach, D.K.; Weber, A.A.; Zapp, J.; Maurer, H.H. Metabolism studies of the Kratom alkaloid speciociliatine, a diastereomer of the main alkaloid mitragynine, in rat and human urine using liquid chromatography-linear ion trap mass spectrometry. Anal. Bioanal. Chem. 2011, 399, 2747–2753. [Google Scholar] [CrossRef] [PubMed]
- Mcintyre, I.M.; Trochta, A.; Stolberg, S.; Campman, S.C. Mitragynine ‘Kratom’ Related Fatality: A Case Report with Postmortem Concentrations. J. Anal. Toxicol. 2014, 39, 152–155. [Google Scholar] [CrossRef] [PubMed]
- Hanapi, N.A.; Ismail, S.; Mansor, S.M. Inhibitory effect of mitragynine on human cytochrome P450 enzyme activities. Pharmacogn. Res. 2013, 5, 241–246. [Google Scholar]
- Cinosi, E.; Martinotti, G.; Simonato, P.; Singh, D.; Demetrovics, Z.; Roman-Urrestarazu, A.; Bersani, F.S.; Vicknasingam, B.; Piazzon, G.; Li, J.H.; et al. Following “the Roots” of Kratom (Mitragyna speciosa): The Evolution of an Enhancer from a Traditional Use to Increase Work and Productivity in Southeast Asia to a Recreational Psychoactive Drug in Western Countries. Biomed. Res. Int. 2015, 2015, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Koe, X.F.; Jamil, M.F.A.; Adenan, M.I.; Tan, M.L.; Lim, E.L.; Seah, T.C.; Majid, M.I.A.; Wahab, H.A. In vitro evaluation of cytochrome P450 induction and the inhibition potential of mitragynine, a stimulant alkaloid. Toxicol. In Vitr. 2012, 27, 812–824. [Google Scholar]
- Showande, S.J.; Fakeye, T.O.; Kajula, M.; Hokkanen, J.; Tolonen, A. Potential inhibition of major human cytochrome P450 isoenzymes by selected tropical medicinal herbs—Implication for herb–drug interactions. Food Sci. Nutr. 2019, 7, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Ulbricht, C.; Costa, D.; Dao, J.; Isaac, R.; Leblanc, Y.C.; Rhoades, J.; Windsor, R.C. An evidence-based systematic review of kratom (Mitragyna speciosa) by the natural standard research collaboration. J. Diet. Suppl. 2013, 10, 152–170. [Google Scholar] [CrossRef] [PubMed]
- Hughes, R.L. Fatal combination of mitragynine and quetiapine—A case report with discussion of a potential herb-drug interaction. Forensic Sci. Med. Pathol. 2018, 15, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.B.; Pakiam, C.; Rahim, R.A. Psychoactive plant abuse: The identification of mitragynine in ketum and in ketum preparations. Bull. Narc. 2007, 249, 249–256. [Google Scholar]
- Roche, K.M.; Hart, K.; Sangalli, B.; Lefberg, J.; Bayer, M. Kratom: A Case of a Legal High. Clin. Toxicol. 2008, 46, 598. [Google Scholar]
- Ward, J.; Rosenbaum, C.; Hernon, C.; McCurdy, C.R.; Boyer, E.W. Herbal Medicines for the Management of Opioid Addiction. CNS Drugs 2011, 25, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, K.; Horie, S.; Takayama, H.; Ishikawa, H.; Aimi, N.; Ponglux, D.; Murayama, T.; Watanabe, K. Antinociception, tolerance and withdrawal symptoms induced by 7-hydroxymitragynine, an alkaloid from the Thai medicinal herb Mitragyna speciosa. Life Sci. 2005, 78, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Hassan, Z.; Muzaimi, M.; Navaratnam, V.; Yusoff, N.H.M.; Suhaimi, F.W.; Vadivelu, R.; Vicknasingam, B.K.; Amato, D.; von Hörsten, S.; Ismail, N.I.W.; et al. From Kratom to mitragynine and its derivatives: Physiological and behavioural effects related to use, abuse, and addiction. Neurosci. Biobehav. Rev. 2013, 37, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Thongpradichote, S.; Matsumoto, K.; Tohda, M.; Takayama, H.; Aimi, N.; Sakai, S.I.; Watanabe, H. Identification of opioid receptor subtypes in antinociceptive actions of supraspinally-administered mitragynine in mice. Life Sci. 1998, 62, 1371–1378. [Google Scholar] [CrossRef]
- Yamamoto, L.T.; Horie, S.; Takayama, H.; Aimi, N.; Sakai, S.I.; Yano, S.; Shan, J.; Pang, P.K.T.; Ponglux, D.; Watanabe, K. Opioid receptor agonistic characteristics of mitragynine pseudoindoxyl in comparison with mitragynine derived from Thai medicinal plant Mitragyna speciosa. Gen. Pharmacol. 1999, 33, 73–81. [Google Scholar] [CrossRef]
- White, C.M. Pharmacologic and clinical assessment of kratom. Bull. Am. Soc. Hosp. Pharm. 2018, 75, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Stolt, A.-C.; Schröder, H.; Neurath, H.; Grecksch, G.; Höllt, V.; Meyer, M.R.; Maurer, H.H.; Ziebolz, N.; Havemann-Reinecke, U.; Becker, A. Behavioral and neurochemical characterization of kratom (Mitragyna speciosa) extract. Psychopharmacology 2014, 231, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Hemby, S.E.; McIntosh, S.; Leon, F.; Cutler, S.J.; McCurdy, C.R. Abuse liability and therapeutic potential of the Mitragyna speciosa (kratom) alkaloids mitragynine and 7-hydroxymitragynine. Addict. Biol. 2018, in press. [Google Scholar] [CrossRef] [PubMed]
- Vermaire, D.J.; Skaer, D.; Tippets, W. Kratom and General Anesthesia: A Case Report and Review of the Literature. A A Pract. 2019, 12, 103–105. [Google Scholar] [CrossRef] [PubMed]
- Vijeepallam, K.; Pandy, V.; Kunasegaran, T.; Murugan, D.D.; Naidu, M. Mitragyna speciosa leaf extract exhibits antipsychotic-like effect with the potential to alleviate positive and negative symptoms of psychosis in mice. Front. Pharmacol. 2016, 7, 464. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Yano, S.; Horie, S.; Yamamoto, L. Inhibitory effect of mitragynine, an alkaloid with analgesic effect from Thai medicinal plant Mitragyna speciosa, on electrically stimulated contraction of isolated guinea-pig ileum through the opioid receptor. Life Sci. 1997, 60, 933–942. [Google Scholar] [CrossRef]
- Havemann-Reinecke, U. P01-50-Kratom and alcohol dependence: Clinical symptoms, withdrawal treatment and pharmacological mechanisms—A case report. Eur. Psychiatry 2011, 26, 50. [Google Scholar] [CrossRef]
- Matsumoto, K.; Yamamoto, L.T.; Watanabe, K.; Yano, S.; Shan, J.; Pang, P.K.T.; Ponglux, D.; Takayama, H.; Horie, S. Inhibitory effect of mitragynine, an analgesic alkaloid from Thai herbal medicine, on neurogenic contraction of the vas deferens. Life Sci. 2005, 78, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Wei, H.; Wu, J.; Fadzly, M.; Jamil, A. Evaluation of the Cardiotoxicity of Mitragynine and Its Analogues Using Human Induced Pluripotent Stem Cell- Derived Cardiomyocytes. PLoS ONE 2014, 9, e115648. [Google Scholar] [CrossRef] [PubMed]
- Horie, S.; Koyama, F.; Takayama, H.; Ishikawa, H.; Aimi, N.; Ponglux, D.; Matsumoto, K.; Murayama, T. Indole alkaloids of a Thai medicinal herb, Mitragyna speciosa, that has opioid agonistic effect in guinea-pig ileum. Planta Med. 2005, 71, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Reanmongkol, W.; Keawpradub, N.; Sawangjaroen, K. Effects of the extracts from Mitragyna speciosa Korth. leaves on analgesic and behavioral activities in experimental animals. Songklanakarin J. Sci. Technol. 2017, 29, 39–48. [Google Scholar]
- Sabetghadam, A.; Ramanathan, S.; Mahsufi Mansor, S. The evaluation of antinociceptive activity of alkaloid, methanolic, and aqueous extracts of Malaysian Mitragyna speciosa Korth leaves in rats. Pharmacogn. Res. 2010, 2, 181–185. [Google Scholar]
- Matsumoto, K.; Hatori, Y.; Murayama, T. Involvement of μ-opioid receptors in antinociception and inhibition of gastrointestinal transit induced by 7-hydroxymitragynine, isolated from Thai herbal medicine Mitragyna speciosa. Eur. J. Pharmacol. 2006, 549, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Utar, Z.; Majid, M.I.A.; Adenan, M.I.; Jamil, M.F.A.; Lan, T.M. Mitragynine inhibits the COX-2 mRNA expression and prostaglandin E2 production induced by lipopolysaccharide in RAW264.7 macrophage cells. J. Ethnopharmacol. 2011, 136, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Mossadeq, W.M.S.; Sulaiman, M.R.; Mohamad, T.A.T.; Chiong, H.S.; Zakaria, Z.A.; Jabit, M.L.; Baharuldin, M.T.H.; Israf, D.A. Anti-Inflammatory and Antinociceptive Effects of Mitragyna speciosa Korth. Med. Princ. Pract. 2009, 18, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Chittrakarn, S.; Sawangjaroen, K.; Prasettho, S.; Janchawee, B.; Keawpradub, N. Inhibitory effects of kratom leaf extract (Mitragyna speciosa Korth.) on the rat gastrointestinal tract. J. Ethnopharmacol. 2008, 116, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, S.; Miyashita, S.; Yamamoto, M.; Horie, S.; Sakai, S. Effect of mitragynine, derived from Thai folk medicine, on gastric acid secretion through opioid receptor in anesthetized rats. Eur. J. Pharmacol. 2002, 443, 185–188. [Google Scholar] [CrossRef]
- Sabetghadam, A.; Ramanathan, S.; Sasidharan, S.; Mansor, S.M. Subchronic exposure to mitragynine, the principal alkaloid of Mitragyna speciosa, in rats. J. Ethnopharmacol. 2013, 146, 815–823. [Google Scholar] [CrossRef] [PubMed]
- Purintrapiban, J.; Keawpradub, N. Study on glucose transport in muscle cells by extracts from Mitragyna speciosa (Korth) and mitragynine. Nat. Prod. Res. 2011, 25, 1379–1387. [Google Scholar] [CrossRef] [PubMed]
- Kumarnsit, E.; Keawpradub, N.; Nuankaew, W. Effect of Mitragyna speciosa aqueous extract on ethanol withdrawal symptoms in mice. Fitoterapia 2007, 78, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Farah Idayu, N.; Taufik Hidayat, M.; Moklas, M.A.M.; Sharida, F.; Nurul Raudzah, A.R.; Shamima, A.R.; Apryani, E. Antidepressant-like effect of mitragynine isolated from Mitragyna speciosa Korth in mice model of depression. Phytomedicine 2011, 18, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.I.W.; Jayabalan, N.; Mansor, S.M.; Müller, C.P.; Muzaimi, M. Chronic mitragynine (kratom) enhances punishment resistance in natural reward seeking and impairs place learning in mice. Addict. Biol. 2017, 22, 967–976. [Google Scholar] [CrossRef] [PubMed]
- Hazim, A.I.; Mustapha, M.; Mansor, S.M. The effects on motor behaviour and short-term memory tasks in mice following an acute administration of Mitragyna speciosa alkaloid extract and mitragynine. J. Med. Plants 2011, 5, 5810–5817. [Google Scholar]
- Singh, D.; Narayanan, S.; Müller, C.P.; Vicknasingam, B.; Yücel, M.; Ho, E.T.W.; Hassan, Z.; Mahsufi Mansor, S. Long-Term Cognitive Effects of Kratom (Mitragyna speciosa Korth.) Use. J. Psychoact. Drugs 2018, 51, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, S.; Bin Azizi, J.; Ramanathan, S.; Ismail, S.; Sasidharan, S.; Mohd, M.I.; Mansor, S.M. Evaluation of antioxidant and antibacterial activities of aqueous, methanolic and alkaloid extracts from Mitragyna speciosa (rubiaceae family) leaves. Molecules 2009, 14, 3964–3974. [Google Scholar] [CrossRef] [PubMed]
- Suwanlert, S. A study of kratom eaters in Thailand. Bull. Narc. 1975, 27, 21–27. [Google Scholar] [PubMed]
- Stanciu, C.N.; Gnanasegaram, S.A.; Ahmed, S.; Penders, T. Kratom Withdrawal: A Systematic Review with Case Series. J. Psychoact. Drugs 2019, 51, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Smid, M.C.; Charles, J.E.; Gordon, A.J.; Wright, T.E. Use of Kratom, an Opioid-like Traditional Herb, in Pregnancy. Obstet. Gynecol. 2018, 132, 926–928. [Google Scholar] [CrossRef] [PubMed]
- Davidson, L.; Rawat, M.; Stojanovski, S.; Chandrasekharan, P. Natural Drugs, Not So Natural Effects: Neonatal Abstinence Syndrome Secondary to ‘Kratom’. J. Neonatal-Perinat. Med. 2018, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Swogger, M.T.; Walsh, Z. Kratom use and mental health: A systematic review. Drug Alcohol Depend. 2018, 183, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Azizi, J.; Ismail, S.; Mordi, M.N.; Ramanathan, S.; Said, M.I.M.; Mansor, S.M. In vitro and in vivo effects of three different Mitragyna speciosa korth leaf extracts on phase II drug metabolizing enzymes-glutathione transferases (GSTs). Molecules 2010, 15, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Harizal, S.N.; Mansor, S.M.; Hasnan, J.; Tharakan, J.K.J.; Abdullah, J. Acute toxicity study of the standardized methanolic extract of Mitragyna speciosa Korth in Rodent. J. Ethnopharmacol. 2010, 131, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Ilmie, M.U.; Jaafar, H.; Mansor, S.M.; Abdullah, J.M. Subchronic toxicity study of standardized methanolic extract of Mitragyna speciosa Korth in Sprague-Dawley Rats. Front. Neurosci. 2015, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Saidin, N.A.; Randall, T.; Takayama, H.; Holmes, E.; Gooderham, N. Malaysian Kratom, a phyto-pharmaceutical of abuse: Studies on the mechanism of its cytotoxicity. Toxicology 2008, 253, 19–20. [Google Scholar] [CrossRef]
- Fluyau, D.; Revadigar, N. Biochemical benefits, diagnosis, and clinical risks evaluation of kratom. Front. Psychiatry 2017, 8, 62. [Google Scholar] [CrossRef] [PubMed]
- Rusli, N.; Amanah, A.; Kaur, G.; Adenan, M.I.; Sulaiman, S.F.; Wahab, H.A.; Tan, M.L. The inhibitory effects of mitragynine on P-glycoprotein in vitro. Naunyn-Schmiedebergs Arch. Pharmacol. 2019, 1–16. Available online: https://link.springer.com/article/10.1007%2Fs00210-018-01605-y (accessed on 3 March 2019).
- Nelsen, J.L.; Lapoint, J.; Hodgman, M.J.; Aldous, K.M. Seizure and Coma Following Kratom (Mitragynina speciosa Korth) Exposure. J. Med. Toxicol. 2010, 6, 424–426. [Google Scholar] [CrossRef] [PubMed]
- Kronstrand, R.; Roman, M.; Thelander, G.; Eriksson, A. Unintentional Fatal Intoxications with Mitragynine and O-Desmethyltramadol from the Herbal Blend Krypton. J. Anal. Toxicol. 2011, 35, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Hypothyroidism, S.P.; Sheleg, S.V.; Collins, G.B. A Coincidence of Addiction to “kratom” and Severe Primary Hypothyroidism. Am. Soc. Addict. Med. 2011, 5, 300–301. [Google Scholar]
- Kapp, F.G.; Maurer, H.H.; Auwärter, V.; Winkelmann, M. Hermanns-Clausen, M. Intrahepatic Cholestasis Following Abuse of Powdered Kratom (Mitragyna speciosa). J. Med. Toxicol. 2011, 7, 227–231. [Google Scholar] [CrossRef] [PubMed]
- McWhirter, L.; Morris, S. A case report of inpatient detoxification after kratom (Mitragyna speciosa) dependence. Eur. Addict. Res. 2010, 16, 229–231. [Google Scholar] [CrossRef] [PubMed]
- Domingo, O.; Roider, G.; Stöver, A.; Graw, M.; Musshoff, F.; Sachs, H.; Bicker, W. Mitragynine concentrations in two fatalities. Forensic Sci. Int. 2017, 271, e1–e7. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Narayanan, S.; Vicknasingam, B.; Corazza, O.; Santacroce, R.; Roman-Urrestarazu, A. Changing trends in the use of kratom (Mitragyna speciosa) in Southeast Asia. Hum. Psychopharmacol. Clin. Exp. 2017, 32, e2582. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Narayanan, S.; Müller, C.P.; Swogger, M.T.; Chear, N.J.Y.; Bin Dzulkapli, E.; Yusoff, N.S.M.; Ramachandram, D.S.; León, F.; McCurdy, C.R.; et al. Motives for using Kratom (Mitragyna speciosa Korth.) among regular users in Malaysia. J. Ethnopharmacol. 2019, 233, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration Statement from FDA Commissioner Scott Gottlieb, M.D., on the Agency’s Scientific Evidence on the Presence of Opioid Compounds in Kratom, Underscoring Its Potential for Abuse. Available online: https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm595622.htm (accessed on 18 January 2019).
- Kikura-Hanajiri, R. Detection of mitragyne and its analogs. In Kratom and Other Mitragynines: The Chemistry and Pharmacology of Opioids from a Non-Opium Source; Raffa, R.B., Ed.; CRC Press: Boca Raton, FL, USA, 2014; pp. 153–166. [Google Scholar]
- Wang, M.; Carrell, E.J.; Ali, Z.; Avula, B.; Avonto, C.; Parcher, J.F.; Khan, I.A. Comparison of three chromatographic techniques for the detection of mitragynine and other indole and oxindole alkaloids in Mitragyna speciosa (kratom) plants. J. Sep. Sci. 2014, 37, 1411–1418. [Google Scholar] [CrossRef] [PubMed]
- Kowalczuk, A.; Losak, A.; Zjawiony, A.L. Comprehensive methodology for identification of Kratom in police laboratories. Forensic Sci. Int. 2013, 233, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, S.; Ramanathan, S.; Murugaiyah, V. A simple HPLC-DAD method for the detection and quantification of psychotropic mitragynine in Mitragyna speciosa (ketum) and its products for the application in forensic investigation. Forensic Sci. Int. 2013, 226, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Fuenffinger, N.; Ritchie, M.; Ruth, A.; Gryniewicz-ruzicka, C. Evaluation of ion mobility spectrometry for the detection of mitragynine in kratom products. J. Pharm. Biomed. Anal. 2017, 134, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Limsuwanchote, S.; Wungsintaweekul, J.; Keawpradub, N.; Putalun, W.; Morimoto, S.; Tanaka, H. Development of indirect competitive ELISA for quantification of mitragynine in Kratom (Mitragyna speciosa (Roxb.) Korth.). Forensic Sci. Int. 2015, 244, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Philipp, A.A.; Meyer, M.R.; Wissenbach, D.K.; Weber, A.A.; Zoerntlein, S.W.; Zweipfenning, P.G.M.; Maurer, H.H. Monitoring of kratom or Krypton intake in urine using GC-MS in clinical and forensic toxicology. Anal. Bioanal. Chem. 2011, 400, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Mudge, E.M.; Brown, P.N. Determination of mitragynine in Mitragyna speciosa raw materials and finished products by liquid chromatography with UV detection: Single-laboratory validation. J. AOAC Int. 2017, 100, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Orio, L.; Alexandru, L.; Cravotto, G.; Mantegna, S.; Barge, A. UAE, MAE, SFE-CO2 and classical methods for the extraction of Mitragyna speciosa leaves. Ultrason. Sonochem. 2012, 19, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Le, D.; Goggin, M.M.; Janis, G.C. Analysis of Mitragynine and Metabolites in Human Urine for Detecting the Use of the Psychoactive Plant Kratom. J. Anal. Toxicol. 2012, 36, 616–625. [Google Scholar] [CrossRef] [PubMed]
- Philipp, A.A.; Wissenbach, D.K.; Zoerntlein, S.W.; Klein, O.N.; Kanogsunthornrat, J.; Maurer, H.H. Studies on the metabolism of mitragynine, the main alkaloid of the herbal drug Kratom, in rat and human urine using liquid chromatography-linear ion trap mass spectrometry. J. Mass Spectrom. 2009, 44, 1249–1261. [Google Scholar] [CrossRef] [PubMed]
- Guddat, S.; Görgens, C.; Steinhart, V.; Schänzer, W.; Thevis, M. Mitragynine (Kratom)—Monitoring in sports drug testing. Drug Test. Anal. 2016, 8, 1114–1118. [Google Scholar] [CrossRef] [PubMed]
- Holler, J.M.; Vorce, S.P.; McDonough-Bender, P.C.; Magluilo, J.; Solomon, C.J.; Levine, B. A drug toxicity death involving propylhexedrine and mitragynine. J. Anal. Toxicol. 2011, 35, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Tran, B.N.; Nelsen, J.L.; Aldous, K.M. Quantitative analysis of mitragynine in human urine by high performance liquid chromatography-tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2009, 877, 2499–2505. [Google Scholar] [CrossRef] [PubMed]
- Prutipanlai, S.; Botpiboon, O.; Janchawee, B.; Theanchaiwattana, S. Solid phase extraction method for determination of mitragynine in urine and its application to mitragynine excretion study in rats receiving caffeine. Trop. J. Pharm. Res. 2017, 16, 1675. [Google Scholar] [CrossRef]
- Neng, N.R.; Ahmad, S.M.; Gaspar, H.; Nogueira, J.M.F. Determination of mitragynine in urine matrices by bar adsorptive microextraction and HPLC analysis. Talanta 2015, 144, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Basiliere, S.; Bryand, K.; Kerrigan, S. Identification of five Mitragyna alkaloids in urine using liquid chromatography-quadrupole/time of flight mass spectrometry. J. Chromatogr. B 2018, 1080, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Janchawee, B.; Keawpradub, N.; Chittrakarn, S.; Prasettho, S.; Wararatananurak, P.; Sawangjareon, K. A high-performance liquid chromatographic method for determination of mitragynine in serum and its application to a pharmacokinetic study in rats. Biomed. Chromatogr. 2007, 183, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Chittrakarn, S.; Penjamras, P.; Keawpradub, N. Quantitative analysis of mitragynine, codeine, caffeine, chlorpheniramine and phenylephrine in a kratom (Mitragyna speciosa Korth.) cocktail using high-performance liquid chromatography. Forensic Sci. Int. 2012, 217, 81–86. [Google Scholar] [CrossRef] [PubMed]

| Compounds | Biological Sample (amount) | Analytical Technique | Internal Standard | Extraction Process | Linear Range (ng/mL) | LOD (ng/mL) | LOQ (ng/mL) | Recovery (%) | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Mitragynine, 7-hydroxymitraginine, speciogynine, speciocilliatine, and paynantheine | Urine (1 mL) | LC–ESI–MS–QTOF | mitragynine-d3 7-hydroxymitraginine-d3 | Solid-phase extraction (PolyChrom ClinII cartridges) | 2–500 | 0.25–1 | 0.5–1 | 96–63 | [120] |
| Mitragynine, 5-desmethylmitragynine and 17-desmethyldihydro-Mitragynine, and 7-hidroxymitragynine | Urine (0.2 mL) | UHPLC–ESI/MS–MS and LC–ESI/MS–MS | Mitraphylline | Enzymatic hydrolysis and liquid-liquid extraction (methyl tert-butyl ether) | 1–500 | - | 1.00 | 78–94 | [113] |
| Mitragynine | Urine (1 mL) | HPLC–DAD | - | BAµE (N-vinylpyrrolidone polymer) and back-extraction with methanol/acetonitrile (1:1, v/v) under sonication | 0.6–24 | 0.1 | 0.33 | 103 | [119] |
| Mitragynine | Urine (1 mL) | LC–ESI–MS (QTRAP) | methyltestosterone | Enzymatic hydrolysis and liquid-liquid extraction (ethyl tert-butyl ether) | 0.25–1.5 | 0.2 | 0.25 | 83 | [115] |
| Mitragynine | Peripheral blood, central blood, liver, vitreous, gastric content, and urine (1 mL) | GC–MS (EI) | mitragynine-d3 | Solid-phase extraction (Trace-J cartridges) | 50–1000 | 30 | 50 | - | [45] |
| Mitragynine, paynantheine, speciogynine, speciociliatine, 16-carboxy-mitragynine, 9-O-demethyl-mitragynine, and 9-O-demethyl-16-carboxy-mitragynine | Urine (3 mL) | GC–MS (EI) | - | Enzymatic hydrolysis and solid-phase extraction (HCX cartridge) | - | 100 | - | - | [110] |
| Mitragynine | Urine (2 mL) | LC–ESI/MS–MS | Ajmalicine | Liquid extraction; liquid-liquid extraction (Methyl tert-butyl ether) | 0.01–5 | 0.02 | 0.1 | 81 | [117] |
| Mitragynine | Blood and urine (1 mL), tissues (liver, kidney, heart, spleen, lung −1g), bile, and vitreous humor | LC–ESI/MS–MS | Proadifen | Enzymatic hydrolysis and liquid-liquid extraction (n-butyl chloride) | 1–10 | 0.25 | 1 | 103 | [116] |
| Mitragynine | Rat serum (0.1 mL) | HPLC–UV LC–ESI–MS | Acenapthene | Liquid–liquid extraction (diethyl ether) | 100–10,000 | 30 | 100 | 85–84 | [121] |
| Mitragynine | Rat plasma (0.1 mL) | HPLC–UV | Mefloquine | Solid-phase extraction (MCX Oasis cartridges) | 50–1000 | 25 | 50 | 96–98 | [33] |
| Mitragynine | Rat and human urine (1 mL) | HPLC–DAD | - | Solid-phase extraction (Oasis® HLB cartridge) | 100–10,000 | - | 100 | 93–101 | [118] |
| Mitragynine and metabolites | Rat and human urine (1 mL) | LC–ESI.LIT and LC–ESI.Orbitrap MS | - | Enzymatic hydrolysis and solid-phase extraction (Isolute Confirm HCX and Isolute Confirm C18 cartridges) | - | - | - | - | [114] |
| Compounds | Sample (Amount) | Analytical Technique | Extraction | LOD | LOQ | Recovery (%) | Reference |
|---|---|---|---|---|---|---|---|
| Several secondary metabolites | Mature leaves (100 mg) | LC–ESI–TOF–MS | Ice cold methanol | - | - | - | [31] |
| Mitragynine | Dried leaves (1.13 kg) | icELISA and HPLC–DAD | Methanol maceration, acid-base extraction, and silica gel column chromatography | 32.47 μg/mL | - | - | [109] |
| Mitragynine | Leaves (5 kg) | HPLC–DAD | Methanol maceration and liquid extraction (chloroform) | 0.25 μg/mL | 0.5 μg/mL | 95–101 | [107] |
| Ketum drink (1 mL) | Direct injection | ||||||
| Mitragynine 7-OH mitragynine | Raw materials and powdered extracts (100 mg) and capsules | HPLC–UV | For dry test materials (0.5 M acetic acid in 70% methanol) For beverages (dilution with methanol) | 0.002% (w/w) | 0.006% (w/w) | 94–95 | [111] |
| Liquid finished products and/or beverages | 0.2 μg/mL | 0.6 μg/mL | |||||
| 7-hidroxymitragynine | Raw materials, powdered extracts, and capsules | 0.004% (w/w) | 0.011% (w/w) | 96–99 | |||
| Liquid finished products and/or beverages | 0.4 μg/mL | 1.1 μg/mL | |||||
| Mitragynine | Ketum cocktail | HPLC–DAD | Freeze drying and reconstitution with methanol:water (80:20, v/v) | 1.000 μg/mL | 3.000 μg/mL | 95 | [122] |
| Mitragynine | Dried plant material (2 g) | TLC and HPLC–UV | Ethanol | 1 μg /mL | - | - | [106] |
| Mitragynine | Kratom (powder or ground leaves material (100 mg); ¼ tea-spoon, liquid: 250 μL, capsule: 1) | IMS and LC–MS/MS | Methanol and ultrasonic bath sonication | 0.5 ng/μL | - | - | [108] |
| 2000 μg/mL | 6000 μg/mL | ||||||
| Mitragynine, 7-hydroxymitragynine, and mitraphylline (stereoisomers, mitraciliatine, speciogynine, speciociliatine) | Plant material as fresh leaves (1.0 cm × 0.5 cm) | HR–DART–MS | Ethanol | - | - | - | [32] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meireles, V.; Rosado, T.; Barroso, M.; Soares, S.; Gonçalves, J.; Luís, Â.; Caramelo, D.; Simão, A.Y.; Fernández, N.; Duarte, A.P.; et al. Mitragyna speciosa: Clinical, Toxicological Aspects and Analysis in Biological and Non-Biological Samples. Medicines 2019, 6, 35. https://doi.org/10.3390/medicines6010035
Meireles V, Rosado T, Barroso M, Soares S, Gonçalves J, Luís Â, Caramelo D, Simão AY, Fernández N, Duarte AP, et al. Mitragyna speciosa: Clinical, Toxicological Aspects and Analysis in Biological and Non-Biological Samples. Medicines. 2019; 6(1):35. https://doi.org/10.3390/medicines6010035
Chicago/Turabian StyleMeireles, Vânia, Tiago Rosado, Mário Barroso, Sofia Soares, Joana Gonçalves, Ângelo Luís, Débora Caramelo, Ana Y. Simão, Nicolás Fernández, Ana Paula Duarte, and et al. 2019. "Mitragyna speciosa: Clinical, Toxicological Aspects and Analysis in Biological and Non-Biological Samples" Medicines 6, no. 1: 35. https://doi.org/10.3390/medicines6010035
APA StyleMeireles, V., Rosado, T., Barroso, M., Soares, S., Gonçalves, J., Luís, Â., Caramelo, D., Simão, A. Y., Fernández, N., Duarte, A. P., & Gallardo, E. (2019). Mitragyna speciosa: Clinical, Toxicological Aspects and Analysis in Biological and Non-Biological Samples. Medicines, 6(1), 35. https://doi.org/10.3390/medicines6010035