Hardness of Resin Cements Polymerized through Glass-Ceramic Veneers
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Materials
2.3. Preparation of Ceramic Sample
2.4. Preparation of Resin Cement Specimens
2.5. Microhardness Test
2.6. Light Attenuation Test Using MARC Patient Simulator
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- Hardness of the light-polymerized resin cement through ceramics depended on the type of cement, the thickness of the ceramic and polymerization time.
- Mean microhardness of Rely X Veneer cement was significantly higher than that of Variolink Esthetic cement. Although, a direct correlation was found between polymerization time and mean microhardness for both resin cements.
- Although light attenuation was significantly affected by the type of glass ceramic, the hardness of resin cement under different type of glass ceramic disks was not significantly difference.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beier, U.S.; Kapferer, I.; Burtscher, D.; Dumfahrt, H. Clinical Performance of Porcelain Laminate Veneers for up to 20 Years. Int. J. Prosthodont. 2012, 25, 79–85. [Google Scholar]
- Gurel, G.; Morimoto, S.; A Calamita, M.; Coachman, C.; Sesma, N. Clinical Performance of Porcelain Laminate Veneers: Outcomes of the Aesthetic Pre-Evaluative Temporary (APT) Technique. Int. J. Periodont. Restor. Dent. 2012, 32, 625–636. [Google Scholar]
- Li, R.W.K.; Chow, T.W.; Matinlinna, J.P. Ceramic Dental Biomaterials and CAD/CAM Technology: State of the Art. J. Prosthodont. Res. 2014, 58, 208–216. [Google Scholar] [CrossRef]
- Vargas, M.A.; Bergeron, C.; Diaz-Arnold, A. Cementing All-Ceramic Restorations. J. Am. Dent. Assoc. 2011, 142, 20S–24S. [Google Scholar] [CrossRef]
- Layton, D.; Walton, T. An p to 16-Year Prospective Study of 304 Porcelain Veneers. Int. J. Prosthodont. 2007, 20, 389–396. [Google Scholar] [PubMed]
- Fradeani, M. Six-Year Follow-Up with Empress Veneers. Int. J. Periodont. Restor. Dent. 1998, 18, 216–225. [Google Scholar]
- Guess, P.C.; Zavanelli, R.A.; Silva, N.R.F.A.; Bonfante, E.A.; Coelho, P.G.; Thompson, V.P. Monolithic CAD/CAM Lithium Disilicate Versus Veneered Y-TZP Crowns: Comparison of Failure Modes and Reliability after Fatigue. Int. J. Prosthodont. 2010, 23, 434–442. [Google Scholar]
- Meng, X.; Yoshida, K.; Atsuta, M. Influence of Ceramic Thickness on Mechanical Properties and Polymer Structure of Dual-Cured Resin Luting Agents. Dent. Mater. 2008, 24, 594–599. [Google Scholar] [CrossRef]
- Calgaro, P.A.M.; Furuse, A.; Correr, G.; Ornaghi, B.P.; Gonzaga, C.C. Influence of the Interposition of Ceramic Spacers on the Degree of Conversion and the Hardness of Resin Cements. Braz. Oral Res. 2013, 27, 403–409. [Google Scholar] [CrossRef]
- Moreno, M.B.P.; Costa, A.R.; Rueggeberg, F.A.; Correr, A.B.; Sinhoreti, M.A.C.; Ambrosano, G.M.B.; Consani, S.; Sobrinho, L.C. Effect of Ceramic Interposition and Post-activation Times on Knoop Hardness of Different Shades of Resin Cement. Braz. Dent. J. 2018, 29, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Kesrak, P.; Leevailoj, C. Surface Hardness of Resin Cement Polymerized under Different Ceramic Materials. Int. J. Dent. 2012, 2012, 1–5. [Google Scholar] [CrossRef]
- Passos, S.P.; Kimpara, E.T.; Bottino, M.A.; Rizkalla, A.; Santos, G.C. Effect of Ceramic Thickness and Shade on Mechanical Properties of a Resin Luting Agent. J. Prosthodont. 2014, 23, 462–466. [Google Scholar] [CrossRef]
- Pilo, R.; Cardash, H. Post-Irradiation Polymerization of Different Anterior and Posterior Visible Light-Activated Resin Composites. Dent. Mater. 1992, 8, 299–304. [Google Scholar] [CrossRef]
- Peutzfeldt, A.; Lussi, A.; Flury, S. Effect of High-Irradiance Light-Curing on Micromechanical Properties of Resin Cements. BioMed Res. Int. 2016, 2016, 4894653. [Google Scholar] [CrossRef]
- Ilday, N.O.; Bayindir, Y.Z.; Bayindir, F.; Gurpinar, A. The Effect of Light Curing Units, Curing Time, and Veneering Materials on Resin Cement Microhardness. J. Dent. Sci. 2013, 8, 141–146. [Google Scholar] [CrossRef]
- Lopes, C.D.C.A.; Rodrigues, R.B.; Faria-E-Silva, A.; Júnior, P.C.S.; Soares, C.J.; Novais, V.R. Degree of Conversion and Mechanical Properties of Resin Cements Cured Through Different All-Ceramic Systems. Braz. Dent. J. 2015, 26, 484–489. [Google Scholar] [CrossRef]
- Yan, Y.L.; Kim, Y.K.; Kim, K.-H.; Kwon, T.-Y. Changes in Degree of Conversion and Microhardness of Dental Resin Cements. Oper. Dent. 2010, 35, 203–210. [Google Scholar] [CrossRef]
- Giorgi, M.C.C.; Pistor, V.; Mauler, R.S.; Lima, D.A.N.L.; Marchi, G.M.; Aguiar, F.H.B. Influence of Light-Activation Protocol on Methacrylate Resin-Composite Evaluated by Dynamic Mechanical Analysis and Degree of Conversion. Lasers Med. Sci. 2014, 30, 1219–1223. [Google Scholar] [CrossRef]
- Santini, A.; Tiu, S.H.; McGuinness, N.J.; Aldossary, M.S. Light Energy Attenuation Through Orthodontic Ceramic Brackets at Different Irradiation Times. J. Orthod. 2016, 43, 193–201. [Google Scholar] [CrossRef]
- Ilie, N. Transmitted Irradiance Through Ceramics: Effect on the Mechanical Properties of a Luting Resin Cement. Clin. Oral Investig. 2017, 21, 1183–1190. [Google Scholar] [CrossRef]
- Konerding, K.L.; Heyder, M.; Kranz, S.; Guellmar, A.; Voelpel, A.; Watts, D.; Jandt, K.D.; Sigusch, B.W. Study of Energy Transfer by Different Light Curing Units into a class III Restoration as a Function of Tilt Angle and Distance, Using a MARC Patient Simulator (PS). Dent. Mater. 2016, 32, 676–686. [Google Scholar] [CrossRef]
- Oh, S.; Shin, S.-M.; Kim, H.-J.; Paek, J.; Kim, S.-J.; Yoon, T.H.; Kim, S.-Y. Influence of Glass-Based Dental Ceramic Type and Thickness with Identical Shade on the Light Transmittance and the Degree of Conversion of Resin Cement. Int. J. Oral Sci. 2018, 10, 1–6. [Google Scholar] [CrossRef]
- Ilie, N.; Simon, A. Effect of Curing Mode on the Micro-Mechanical Properties of Dual-Cured Self-Adhesive Resin Cements. Clin. Oral Investig. 2012, 16, 505–512. [Google Scholar] [CrossRef]
- Lee, I.B.; An, W.; Chang, J.; Um, C.M. Influence of Ceramic Thickness and Curing Mode on the Polymerization Shrinkage Kinetics of Dual-Cured Resin Cements. Dent. Mater. 2008, 24, 1141–1147. [Google Scholar] [CrossRef]
- Peixoto, R.T.; Paulinelli, V.M.; Sander, H.H.; Lanza, M.D.; Cury, L.A.; Poletto, L.T. Light Transmission Through Porcelain. Dent. Mater. 2007, 23, 1363–1368. [Google Scholar] [CrossRef]
- Hofmann, N.; Papsthart, G.; Hugo, B.; Klaiber, B. Comparison of Photo-Activation Versus Chemical or Dual-Curing of Resin-Based Luting Cements Regarding Flexural Strength, Modulus and Surface Hardness. J. Oral Rehabil. 2001, 28, 1022–1028. [Google Scholar] [CrossRef]
- Watanabe, H.; Kazama, R.; Asai, T.; Kanaya, F.; Ishizaki, H.; Fukushima, M.; Okiji, T. Efficiency of Dual-Cured ResinCement Polymerization Induced by High-Intensity LED Curing Units Through Ceramic Material. Oper. Dent. 2015, 40, 153–162. [Google Scholar] [CrossRef][Green Version]
- Moraes, R.R.; Brandt, W.C.; Naves, L.Z.; Correr-Sobrinho, L.; Piva, E. Light- and Time-Dependent Polymerization of Dual-Cured Resin Luting Agent Beneath Ceramic. Acta Odontol. Scand. 2008, 66, 257–261. [Google Scholar] [CrossRef]
- Gonçalves, L.S.; Moraes, R.; Ogliari, F.A.; Boaro, L.; Braga, R.R.; Consani, S. Improved Polymerization Efficiency of Methacrylate-Based Cements Containing an Iodonium Salt. Dent. Mater. 2013, 29, 1251–1255. [Google Scholar] [CrossRef]
- Breeding, L.C.; Dixon, D.L.; Caughman, W.F. The Curing Potential of Light-Activated Composite Resin Luting Agents. J. Prosthet. Dent. 1991, 65, 512–518. [Google Scholar] [CrossRef]
- Zhang, X.; Wang, F. Hardness of Resin Cement Cured Under Different Thickness of Lithium Disilicate-Based Ceramic. Chin. Med. J. 2011, 124, 3762–3767. [Google Scholar]
- Rasetto, F.H.; Driscoll, C.F.; Prestipino, V.; Masri, R.; von Fraunhofer, J.A. Light Transmission Through All-Ceramic Dental Materials: A Pilot Study. J. Prosthet. Dent. 2004, 91, 441–446. [Google Scholar] [CrossRef]
- AlShaafi, M.M.; AlQahtani, M.Q.; Price, R.B. Effect of Exposure Time on the Polymerization of Resin Cement Through Ceramic. J. Adhes. Dent. 2014, 16, 129–135. [Google Scholar]
- Shenoy, A.; Shenoy, N. Dental Ceramics: An. Update. J. Conserv. Dent. 2010, 13, 195–203. [Google Scholar] [CrossRef]



| Material\Shade | Product Description | Manufacturer | Batch Number |
|---|---|---|---|
| IPS e.max CAD\A2 | Lithium disilicate glass-ceramic | Ivoclar Vivadent AG FL-9494Schaan/Liechtenstein Germany | X09583 |
| Celtra Duo\A2 | Zircona-reinforced lithium silicate ceramic | DeguDent GmbH Rodenbacher Chaussee 4 63457Hanau-Wolfgang, Germbany | 16000013 |
| VITABLOCSEsthetic Line\1M2C | Feldspathic ceramic | VITA Zahnfabrik Spitalgasse3 79713Bad Sackingen, Germany | 57090 |
| Rely X Veneer\ Light yellow | Light-polymerize d resin cements | 3M ESPE 2510 Conway Avenue St. Paul, MN 55144-1000USA | N952985 |
| Variolink Esthetic\ Neutral | Ivoclar Vivadent AG, Fl-9494 Schaan/Liechtenstein, Germany | X16532 |
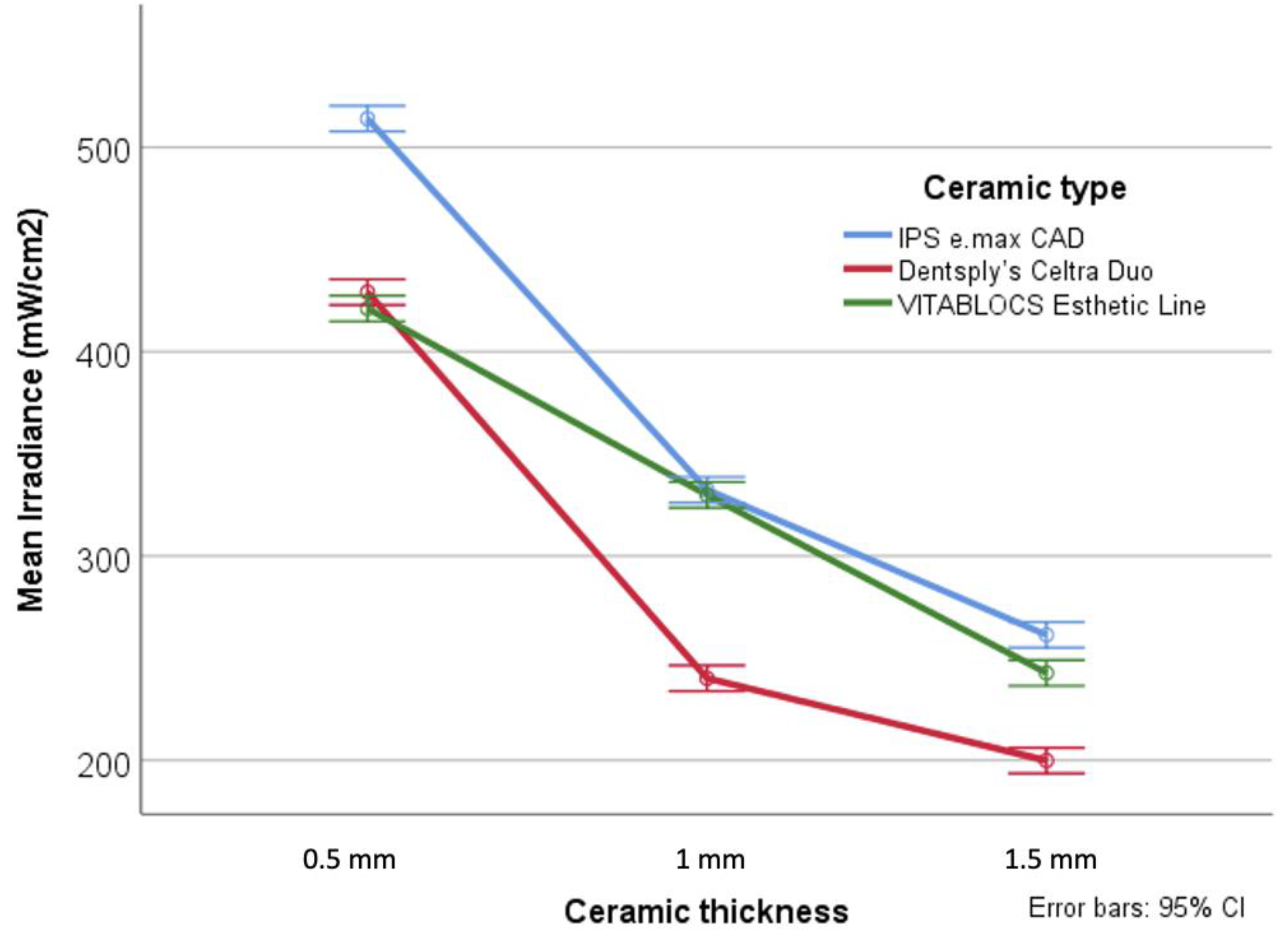
| Ceramic Type and Thickness | Deep-Cure | Blue-Phase | |
|---|---|---|---|
| IPS e.max CAD | 0.5 mm | 566.00 ± 20.97 C | 462.00 ± 23.54 D |
| 1 mm | 361.75 ± 9.59 F | 303.00 ± 21.73 G | |
| 1.5 mm | 286.25 ± 8.11 G,H | 236.50 ± 22.06 I | |
| Celtra Duo | 0.5 mm | 473.00 ± 55.17 D | 385.21 ± 26.41 E,F |
| 1 mm | 251.75 ± 12.63 H,I | 228.50 ± 6.81 K | |
| 1.5 mm | 222.54 ± 4.15 K | 177.25 ± 9.01 L | |
| VITABLOCS Esthetic Line | 0.5 mm | 450.75 ± 7.12 D | 391.42 ± 6.86 E |
| 1 mm | 359.25 ± 9.03 F | 300.50 ± 21.52 G | |
| 1.5 mm | 270.25 ± 30.47 H | 215.25 ± 21.79 K | |
| Control (no ceramic disk interposition) | 1470 ± 3.25 A | 1200 ± 2.7 B | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aldryhim, H.; El-Mowafy, O.; McDermott, P.; Prakki, A. Hardness of Resin Cements Polymerized through Glass-Ceramic Veneers. Dent. J. 2021, 9, 92. https://doi.org/10.3390/dj9080092
Aldryhim H, El-Mowafy O, McDermott P, Prakki A. Hardness of Resin Cements Polymerized through Glass-Ceramic Veneers. Dentistry Journal. 2021; 9(8):92. https://doi.org/10.3390/dj9080092
Chicago/Turabian StyleAldryhim, Hanan, Omar El-Mowafy, Peter McDermott, and Anuradha Prakki. 2021. "Hardness of Resin Cements Polymerized through Glass-Ceramic Veneers" Dentistry Journal 9, no. 8: 92. https://doi.org/10.3390/dj9080092
APA StyleAldryhim, H., El-Mowafy, O., McDermott, P., & Prakki, A. (2021). Hardness of Resin Cements Polymerized through Glass-Ceramic Veneers. Dentistry Journal, 9(8), 92. https://doi.org/10.3390/dj9080092






