Oral Side Effects of the Most Commonly Prescribed Drugs in Germany
Abstract
1. Introduction
2. Materials and Methods
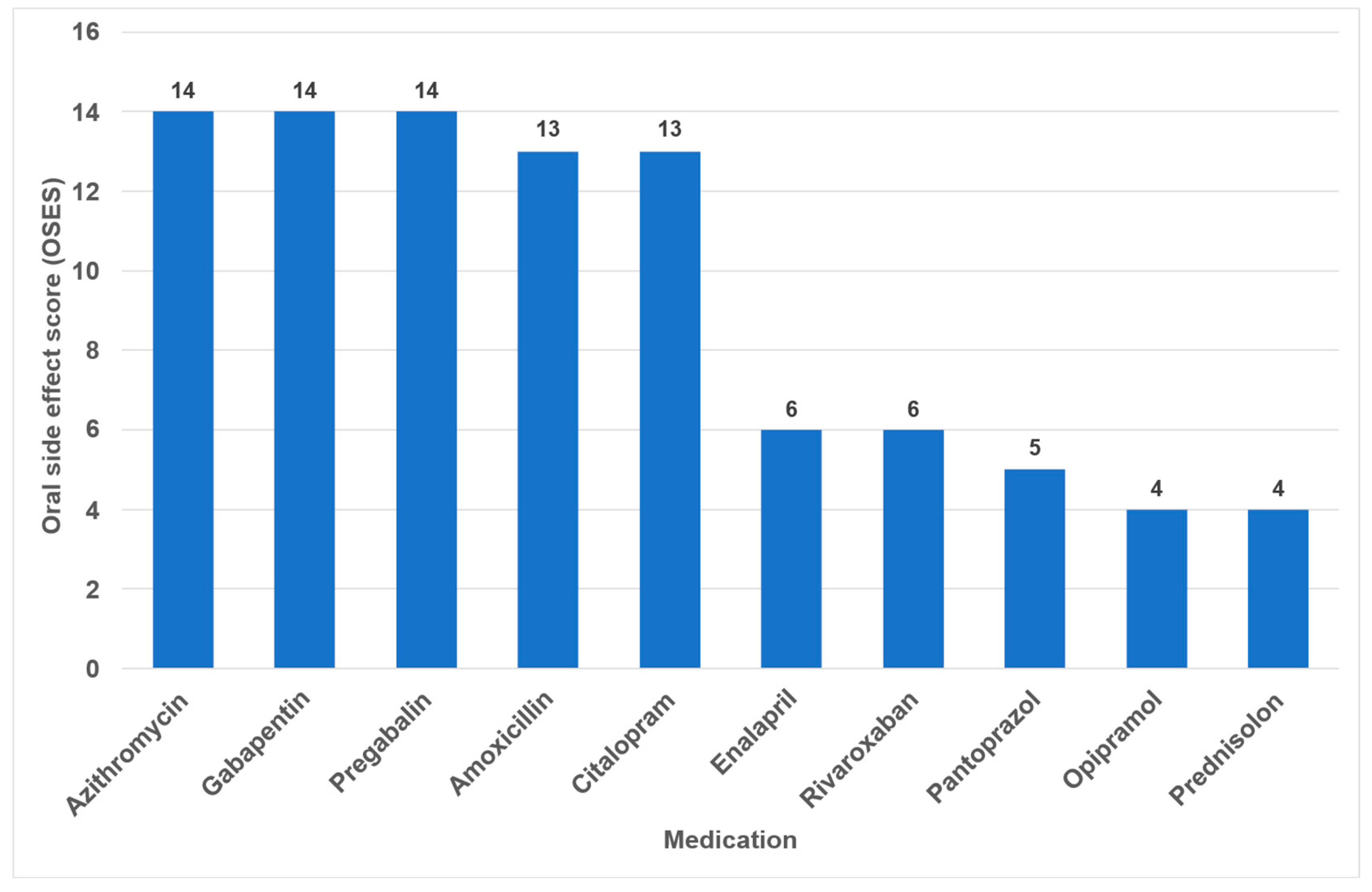
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schumacher, A.E.; Kyu, H.H.; Aali, A.; Abbafati, C.; Abbas, J.; Abbasgholizadeh, R.; Abbasi, M.A.; Abbasian, M.; Abd ElHafeez, S.; Abdelmasseh, M.; et al. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: A comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 1989–2056. [Google Scholar] [CrossRef]
- Deaton, A.S. Health in an Age of Globalization; Princeton University Research Program in Development Studies Working Paper; The Brookings Institution: Washington, DC, USA, 2004. [Google Scholar] [CrossRef]
- McMichael, A.J.; McKee, M.; Shkolnikov, V.; Valkonen, T. Mortality trends and setbacks: Global convergence or divergence? Lancet 2004, 363, 1155–1159. [Google Scholar] [CrossRef]
- Vågerö, D. Health inequalities across the globe demand new global policies. Scand. J. Public Health 2007, 35, 113–115. [Google Scholar] [CrossRef]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef]
- Soto, A.P.; Meyer, S.L. Oral Implications of Polypharmacy in Older Adults. Dent. Clin. N. Am. 2021, 65, 323–343. [Google Scholar] [CrossRef] [PubMed]
- Johnston, M.C.; Crilly, M.; Black, C.; Prescott, G.J.; Mercer, S.W. Defining and measuring multimorbidity: A systematic review of systematic reviews. Eur. J. Public Health 2019, 29, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.R.; Chandra Das, D.; Sunna, T.C.; Beyene, J.; Hossain, A. Global and regional prevalence of multimorbidity in the adult population in community settings: A systematic review and meta-analysis. eClinicalMedicine 2023, 57, 101860. [Google Scholar] [CrossRef] [PubMed]
- Salive, M.E. Multimorbidity in Older Adults. Epidemiol. Rev. 2013, 35, 75–83. [Google Scholar] [CrossRef]
- Aggarwal, P.; Woolford, S.J.; Patel, H.P. Multi-Morbidity and Polypharmacy in Older People: Challenges and Opportunities for Clinical Practice. Geriatrics 2020, 5, 85. [Google Scholar] [CrossRef]
- Afrashteh, S.; Nicholson, K.; Salerno, J.; Borhan, S.; Cossette, B.; Guenter, D.; Vanstone, M.; Queenan, J.; Greiver, M.; Howard, M.; et al. The co-occurrence of multimorbidity and polypharmacy among middle-aged and older adults in Canada: A cross-sectional study using the Canadian Longitudinal Study on Aging (CLSA) and the Canadian Primary Care Sentinel Surveillance Network (CPCSSN). PLoS ONE 2025, 20, e0312873. [Google Scholar] [CrossRef]
- Kim, J.; Parish, A.L. Polypharmacy and Medication Management in Older Adults. Nurs. Clin. N. Am. 2017, 52, 457–468. [Google Scholar] [CrossRef]
- Wastesson, J.W.; Morin, L.; Tan, E.C.K.; Johnell, K. An update on the clinical consequences of polypharmacy in older adults: A narrative review. Expert Opin. Drug Saf. 2018, 17, 1185–1196. [Google Scholar] [CrossRef]
- Halling, F.; Weigl, K. Medical status of elderly patients consulting two oral and maxillofacial surgery departments in Germany. Br. J. Oral Maxillofac. Surg. 2022, 60, 1097–1101. [Google Scholar] [CrossRef]
- Hung, A.; Kim, Y.H.; Pavon, J.M. Deprescribing in older adults with polypharmacy. BMJ 2024, 385, e074892. [Google Scholar] [CrossRef] [PubMed]
- Lavan, A.H.; Gallagher, P. Predicting risk of adverse drug reactions in older adults. Ther. Adv. Drug Saf. 2015, 7, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Ouanounou, A.; Haas, D.A. Pharmacotherapy for the Elderly Dental Patient. J. Can. Dent. Assoc. 2015, 80, f18. [Google Scholar] [PubMed]
- Glick, A.; Sista, V.; Johnson, C. Oral Manifestations of Commonly Prescribed Drugs. Am. Fam. Physician 2020, 102, 613–621. [Google Scholar]
- Shinkai, R.S.; Hatch, J.P.; Schmidt, C.B.; Sartori, E.A. Exposure to the oral side effects of medication in a community-based sample. Spec. Care Dent. 2006, 26, 116–120. [Google Scholar] [CrossRef]
- Smith, R.G.; Burtner, A.P. Oral side-effects of the most frequently prescribed drugs. Spec. Care Dent. 1994, 14, 96–102. [Google Scholar] [CrossRef]
- Zavras, A.I.; Rosenberg, G.E.; Danielson, J.D.; Cartsos, V.M. Adverse drug and device reactions in the oral cavity. J. Am. Dent. Assoc. 2013, 144, 1014–1021. [Google Scholar] [CrossRef]
- IQVIA. Top 10 Pharmaceutical Markets Worldwide, 2024. Available online: https://www.iqvia.com/-/media/iqvia/pdfs/canada/2024-trends/english/top10worldwidesales_24.pdf (accessed on 2 October 2025).
- Becker, D.E. Adverse drug reactions in dental practice. Anesth. Prog. 2014, 61, 26–33. [Google Scholar] [CrossRef]
- Hanlon, J.T.; Schmader, K.E.; Koronkowski, M.J.; Weinberger, M.; Landsman, P.B.; Samsa, G.P.; Lewis, I.K. Adverse Drug Events In High Risk Older Outpatients. J. Am. Geriatr. Soc. 2015, 45, 945–948. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, P.L.; Chavez, E.M. Clinical management of the dental patient taking multiple drugs. J. Contemp. Dent. Pract. 2005, 6, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Domagala-Rodacka, R.; Cibor, D.; Szczeklik, K.; Rodacki, T.; Mach, T.; Owczarek, D. Gastrointestinal tract as a side-effect target of medications. Przegl. Lek. 2016, 73, 652–658. [Google Scholar] [PubMed]
- Yuan, A.; Woo, S.-B. Adverse drug events in the oral cavity. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 35–47. [Google Scholar] [CrossRef]
- Abdollahi, M.; Rahimi, R.; Radfar, M. Current opinion on drug-induced oral reactions: A comprehensive review. J. Contemp. Dent. Pract. 2008, 9, 1–15. [Google Scholar] [CrossRef]
- Ciancio, S.G. Medications’ impact on oral health. J. Am. Dent. Assoc. 2004, 135, 1440–1448. [Google Scholar] [CrossRef]
- Petersen, P.E.; Kandelman, D.; Arpin, S.; Ogawa, H. Global oral health of older people—Call for public health action. Community Dent. Health 2010, 27, 257–267. [Google Scholar]
- Jacob, L.E.; Krishnan, M.; Mathew, A.; Mathew, A.L.; Baby, T.K.; Krishnan, A. Xerostomia—A Comprehensive Review with a Focus on Mid-Life Health. J. Mid-Life Health 2022, 13, 100–106. [Google Scholar] [CrossRef]
- Kiesel, E.K.; Hopf, Y.M.; Drey, M. An anticholinergic burden score for German prescribers: Score development. BMC Geriatr. 2018, 18, 239. [Google Scholar] [CrossRef]
- Rademacher, W.M.H.; Aziz, Y.; Hielema, A.; Cheung, K.C.; de Lange, J.; Vissink, A.; Rozema, F.R. Oral adverse effects of drugs: Taste disorders. Oral Dis. 2019, 26, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Schettler, D. Timing of definitive management of severe orbital and midfacial injuries. Fortschritte Kiefer-Und Gesichts-Chir. 1991, 36, 39–41. [Google Scholar]
- Tiisanoja, A.; Syrjälä, A.M.H.; Kullaa, A.; Ylöstalo, P. Anticholinergic Burden and Dry Mouth in Middle-Aged People. JDR Clin. Transl. Res. 2019, 5, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Boer, C.C.; Correa, M.E.; Miranda, E.C.; de Souza, C.A. Taste disorders and oral evaluation in patients undergoing allogeneic hematopoietic SCT. Bone Marrow Transpl. 2010, 45, 705–711. [Google Scholar] [CrossRef]
- Mortazavi, H.; Shafiei, S.; Sadr, S.; Safiaghdam, H. Drug-related Dysgeusia: A Systematic Review. Oral Health Prev. Dent. 2018, 16, 499–507. [Google Scholar] [CrossRef]
- Jeon, S.; Kim, Y.; Min, S.; Song, M.; Son, S.; Lee, S. Taste Sensitivity of Elderly People Is Associated with Quality of Life and Inadequate Dietary Intake. Nutrients 2021, 13, 1693. [Google Scholar] [CrossRef]
- Zhu, R.; Wang, R.; He, J.; Zhang, L.; An, P.; Li, K.; Ren, F.; Xu, W.; Guo, J. Perceived Taste Loss From Early Adulthood to Mid to Late Adulthood and Mortality. JAMA Otolaryngol. Head Neck Surg. 2025, 151, 335. [Google Scholar] [CrossRef]
- Barbe, A.G. Medication-Induced Xerostomia and Hyposalivation in the Elderly: Culprits, Complications, and Management. Drugs Aging 2018, 35, 877–885. [Google Scholar] [CrossRef]
- Gupta, A.; Epstein, J.B.; Sroussi, H. Hyposalivation in elderly patients. J. Can. Dent. Assoc. 2006, 72, 841–846. [Google Scholar]
- Stoopler, E.T.; Villa, A.; Bindakhil, M.; Diaz, D.L.O.; Sollecito, T.P. Common Oral Conditions: A Review. JAMA 2024, 331, 1045–1054. [Google Scholar] [CrossRef]
- Wang, T.; Glendinning, J.; Grushka, M.; Hummel, T.; Mansfield, K. From the Cover: Drug-Induced Taste Disorders in Clinical Practice and Preclinical Safety Evaluation. Toxicol. Sci. 2017, 156, 315–324. [Google Scholar] [CrossRef]
- Nederfors, T.; Isaksson, R.; Mörnstad, H.; Dahlöf, C. Prevalence of perceived symptoms of dry mouth in an adult Swedish population-relation to age, sex and pharmacotherapy. Community Dent. Oral Epidemiol. 2006, 25, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Prado-Mel, E.; Ciudad-Gutiérrez, P.; Rodríguez-Ramallo, H.; Sánchez-Fidalgo, S.; Santos-Ramos, B.; Villalba-Moreno, A.M. Association between anticholinergic activity and xerostomia and/or xerophthalmia in the elderly: Systematic review. BMC Pharmacol. Toxicol. 2022, 23, 94. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, L.; Naidoo, P. Prescription Drugs and Their Effects on Swallowing. Dysphagia 2008, 24, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Arany, S.; Kopycka-Kedzierawski, D.T.; Caprio, T.V.; Watson, G.E. Anticholinergic medication: Related dry mouth and effects on the salivary glands. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 132, 662–670. [Google Scholar] [CrossRef]
- Tan, E.C.K.; Lexomboon, D.; Sandborgh-Englund, G.; Haasum, Y.; Johnell, K. Medications That Cause Dry Mouth as an Adverse Effect in Older People: A Systematic Review and Metaanalysis. J. Am. Geriatr. Soc. 2018, 66, 76–84. [Google Scholar] [CrossRef]
- Kesh, S.; Bernstein, J.A. Isolated angioedema: A review of classification and update on management. Ann. Allergy Asthma Immunol. 2022, 129, 692–702. [Google Scholar] [CrossRef]
- Rohart, J.; Bouillet, L.; Moizan, H. Prise en charge des patients atteints d’angiœdèmes bradykiniques en chirurgie orale et maxillo-faciale. J. Stomatol. Oral Maxillofac. Surg. 2017, 118, 109–114. [Google Scholar] [CrossRef]
- Lerch, M. Drug-Induced Angioedema. In Adverse Cutaneous Drug Eruptions; Chemical Immunology and Allergy; Karger AG: Basel, Switzerland, 2012; pp. 98–105. [Google Scholar]
- Sportiello, L.; La Mantia, G.; Panzarella, V.; Colella, G.; Potenza, S.; Oteri, G.; Sottosanti, L.; Bellavia, G.; Gaio, M.; Zinzi, A.; et al. Oropharyngeal Adverse Events to Drugs and Vaccines: Pharmacovigilance Data From Italy (2019–2021). Oral Dis. 2024, 31, 993–1005. [Google Scholar] [CrossRef]
- Ferrara, F.; Zovi, A.; Nava, E.; Langella, R.; Vitiello, A. Great Sustainability Results From Appropriate Antihypertensive Therapy. Curr. Probl. Cardiol. 2023, 48, 101857. [Google Scholar] [CrossRef]
- Telrandhe, A.; Phadnis, K.; Dhoble, N.; Padole, N.; Baheti, J. A Review: A Comparative Study of Branded and Generic Anti-Hypertensive Drugs. Asian J. Pharm. Res. Dev. 2024, 12, 42–51. [Google Scholar] [CrossRef]
- Bottiger, Y.; Ekenstrale, E. Adverse drug reactions in the oral cavity. Lakartidningen 2024, 121, 23205. [Google Scholar]
- Bakhtiari, S.; Sehatpour, M.; Mortazavi, H.; Bakhshi, M. Orofacial Manifestation of Adverse Drug Reactions: A Review Study. Med. Pharm. Rep. 2018, 91, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Scully, C.; Bagan, J.V. Adverse Drug Reactions in the Orofacial Region. Crit. Rev. Oral Biol. Med. 2004, 15, 221–239. [Google Scholar] [CrossRef] [PubMed]
- Viniol, A.; Ploner, T.; Hickstein, L.; Haasenritter, J.; Klein, K.M.; Walker, J.; Donner-Banzhoff, N.; Becker, A. Prescribing practice of pregabalin/gabapentin in pain therapy: An evaluation of German claim data. BMJ Open 2019, 9, e021535. [Google Scholar] [CrossRef] [PubMed]
- Schaffer, A.L.; Busingye, D.; Chidwick, K.; Brett, J.; Blogg, S. Pregabalin prescribing patterns in Australian general practice, 2012–2018: A cross-sectional study. BJGP Open 2021, 5, bjgpopen20X101120. [Google Scholar] [CrossRef]
- Wettermark, B.; Brandt, L.; Kieler, H.; Bodén, R. Pregabalin is increasingly prescribed for neuropathic pain, generalised anxiety disorder and epilepsy but many patients discontinue treatment. Int. J. Clin. Pract. 2014, 68, 104–110. [Google Scholar] [CrossRef]
- Yousefi, H.; Abdollahi, M. An Update on Drug-induced Oral Reactions. J. Pharm. Pharm. Sci. 2018, 21, 171–183. [Google Scholar] [CrossRef]
- Boulinguez, S.; Reix, S.; Bedane, C.; Debrock, C.; Bouyssou-Gauthier, M.L.; Sparsa, A.; Le Brun, V.; De Vencay, P.; Bernard, P.; Bonnetblanc, J.M. Role of drug exposure in aphthous ulcers: A case-control study. Br. J. Dermatol. 2000, 143, 1261–1265. [Google Scholar] [CrossRef]
- Albrecht, H.; Schiegnitz, E.; Halling, F. Facts and trends in dental antibiotic and analgesic prescriptions in Germany, 2012–2021. Clin. Oral Investig. 2024, 28, 100. [Google Scholar] [CrossRef]
- Teoh, L.; Stewart, K.; Moses, G. Where are oral and dental adverse drug effects in product information? Int. J. Pharm. Pract. 2020, 28, 591–598. [Google Scholar] [CrossRef]
- Ziegler, A.; Hadlak, A.; Mehlbeer, S.; König, I.R. Comprehension of the Description of Side Effects in Drug Information Leaflets. Dtsch. Ärzteblatt Int. 2013, 110, 669–673. [Google Scholar] [CrossRef]
- Putri, R.A.; Ikawati, Z.; Rahmawati, F.; Yasin, N.M. An Awareness of Pharmacovigilance Among Healthcare Professionals Due to an Underreporting of Adverse Drug Reactions Issue: A Systematic Review of the Current State, Obstacles, and Strategy. Curr. Drug Saf. 2024, 19, 317–331. [Google Scholar] [CrossRef]
- Yip, J.; Radford, D.R.; Brown, D. How do UK dentists deal with adverse drug reaction reporting? Br. Dent. J. 2013, 214, E22. [Google Scholar] [CrossRef]
- Dubrall, D.; Christ, P.; Domgörgen, S.; Schmid, M.; Sachs, B. Factors associated with the completeness of information provided in adverse drug reaction reports of physicians, pharmacists and consumers from Germany. Sci. Rep. 2025, 15, 23751. [Google Scholar] [CrossRef]
- Hatahira, H.; Abe, J.; Hane, Y.; Matsui, T.; Sasaoka, S.; Motooka, Y.; Hasegawa, S.; Fukuda, A.; Naganuma, M.; Ohmori, T.; et al. Drug-induced gingival hyperplasia: A retrospective study using spontaneous reporting system databases. J. Pharm. Health Care Sci. 2017, 3, 19. [Google Scholar] [CrossRef]
- Pulito, C.; Cristaudo, A.; Porta, C.; Zapperi, S.; Blandino, G.; Morrone, A.; Strano, S. Oral mucositis: The hidden side of cancer therapy. J. Exp. Clin. Cancer Res. 2020, 39, 210. [Google Scholar] [CrossRef] [PubMed]
| Oral Side Effects | Oral ADRs in All Categories | Oral ADRs in the Categories ‘Very Common’ and ‘Common’ | ||
|---|---|---|---|---|
| n | Share in % | n | Share in % | |
| Xerostomia | 14 | 20.9 | 7 | 30.4 |
| Dysgeusia | 11 | 16.4 | 5 | 21.8 |
| Angioedema | 10 | 14.9 | - | - |
| Stomatitis | 7 | 10.4 | 2 | 8.7 |
| Thrush | 5 | 7.4 | 2 | 8.7 |
| Sialorrhea | 4 | 6.0 | 1 | 4.3 |
| Pharyngitis | 3 | 4.5 | 2 | 8.7 |
| Gingival bleeding | 3 | 4.5 | 2 | 8.7 |
| Dysphagia | 3 | 4.5 | - | - |
| Tooth discoloration | 2 | 3.0 | - | - |
| Sinusitis | 2 | 3.0 | 2 | 8.7 |
| Hypesthesia | 2 | 3.0 | - | - |
| Bruxism | 1 | 1.5 | - | - |
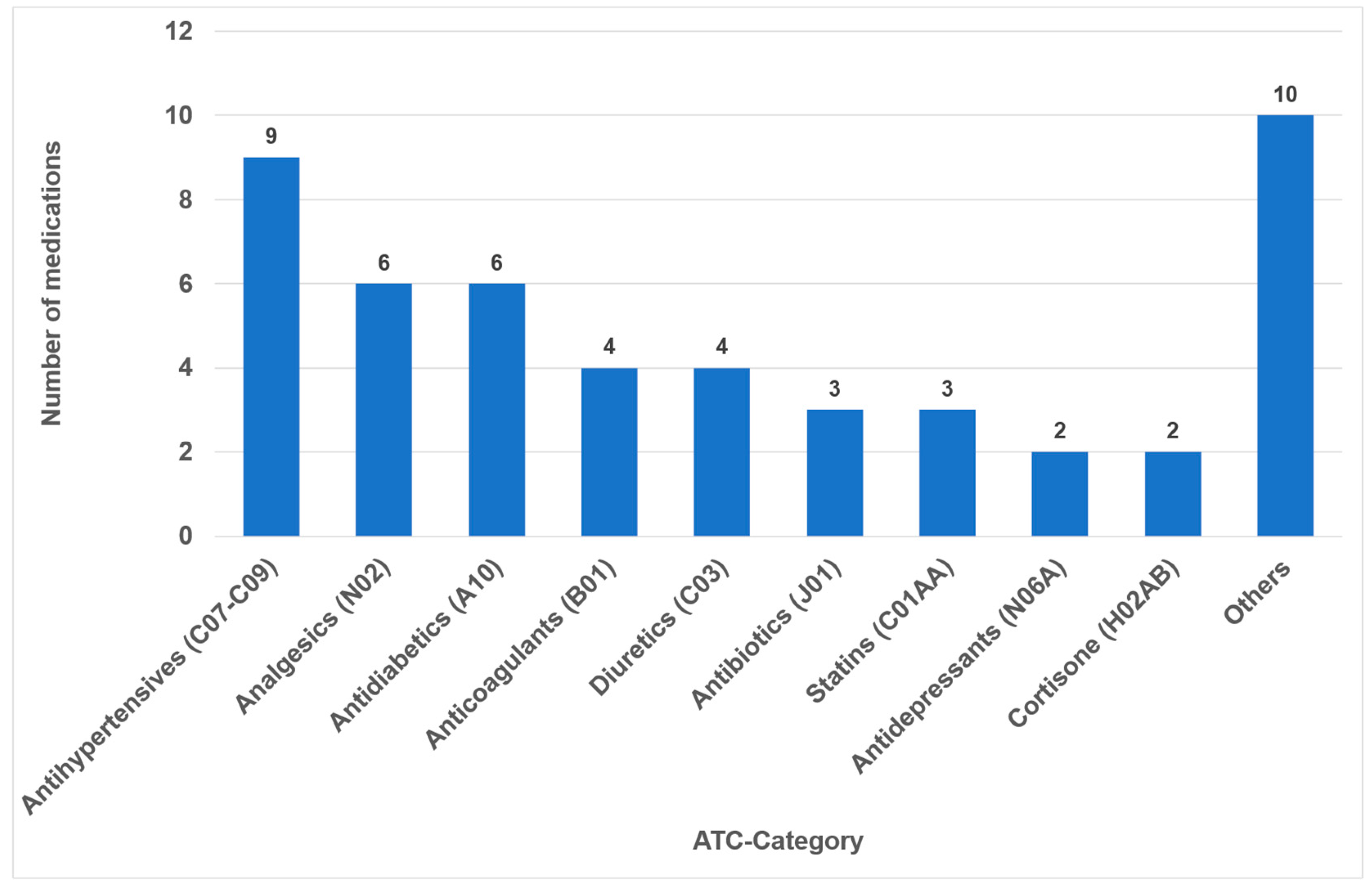
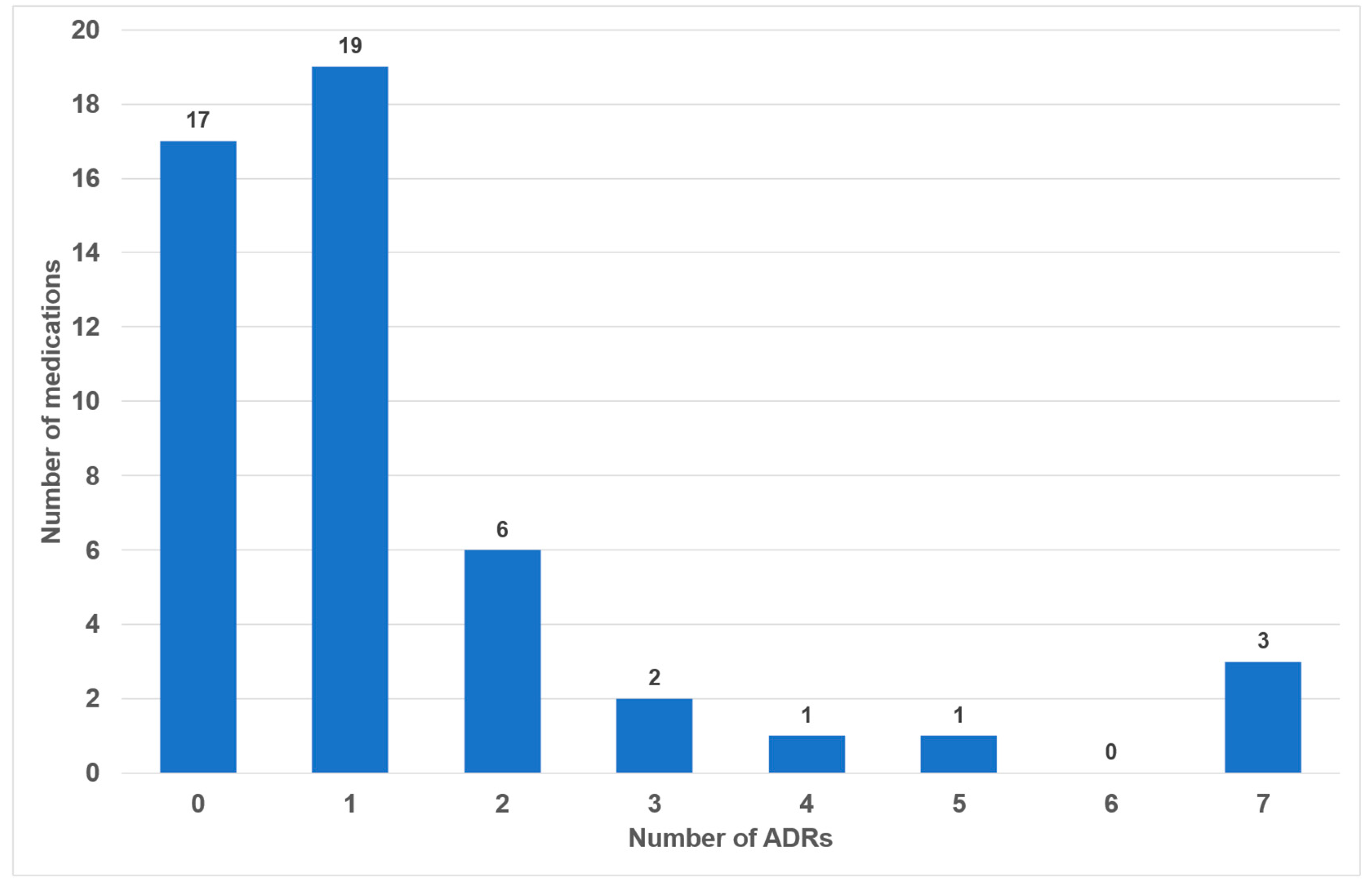
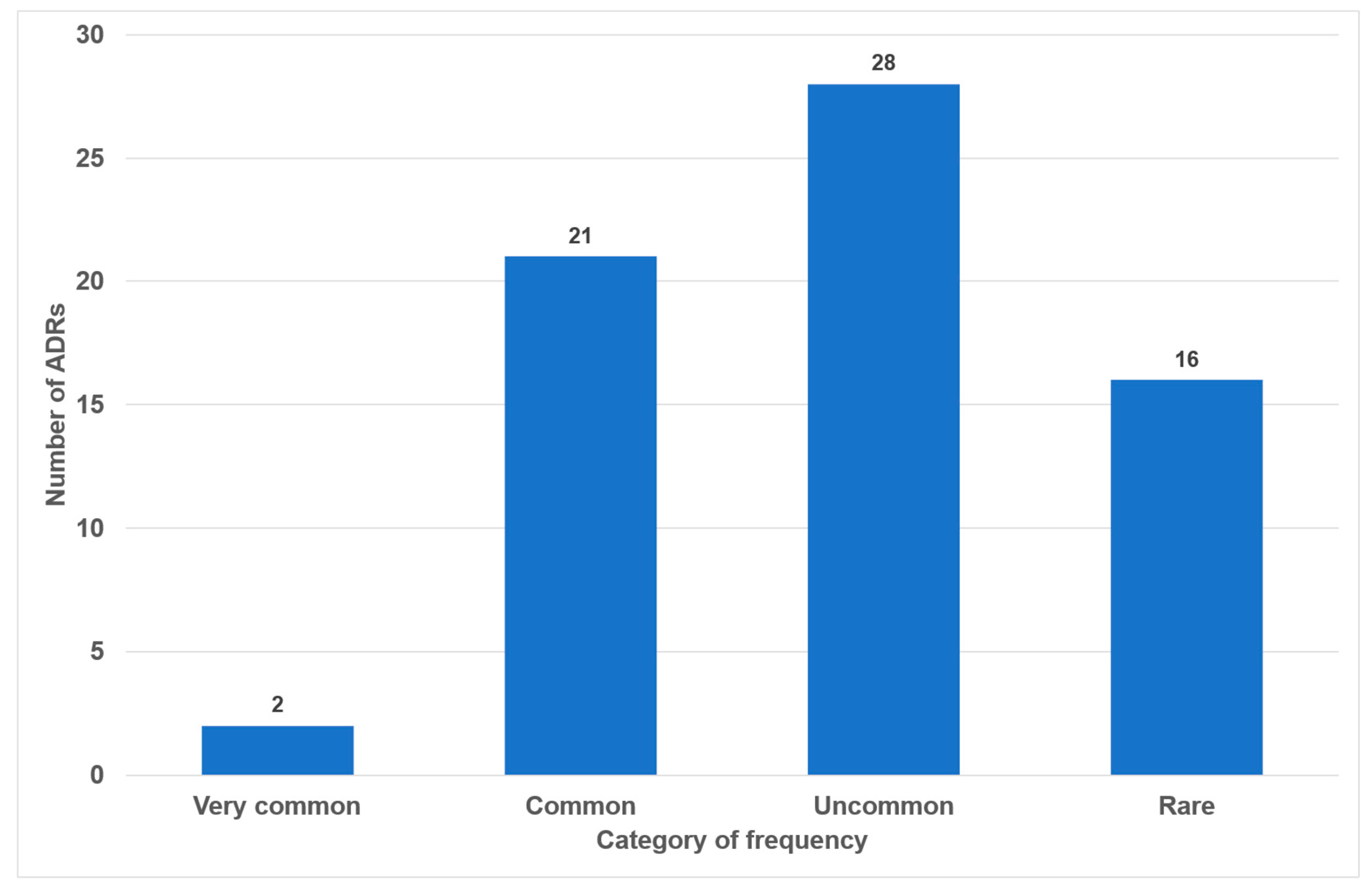
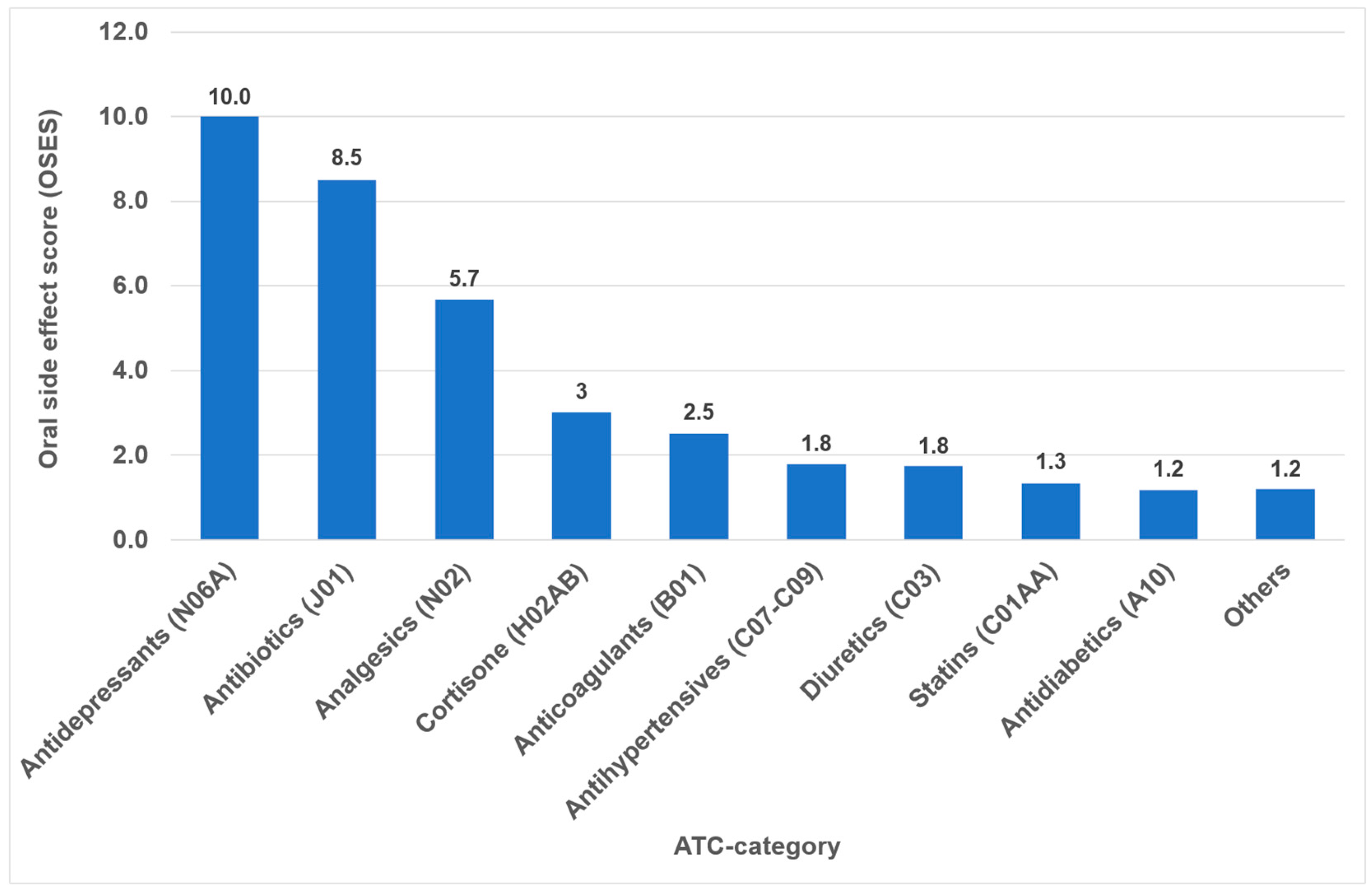
| Medication Classes (ATC-Category) | Medications (n = 49) | Oral ADRs (n = 67) | ||
|---|---|---|---|---|
| n | Share in % | n | Share in % | |
| Analgesics (N02) | 6 | 12.2 | 17 | 25.3 |
| Antibiotics (J01) | 3 | 6.1 | 13 | 19.4 |
| Antihypertensives (C07-C09) | 9 | 18.4 | 9 | 13.4 |
| Others | 10 | 20.4 | 7 | 10.4 |
| Antidepressants (N06A) | 2 | 4.1 | 6 | 9 |
| Anticoagulants (B01) | 4 | 8.2 | 4 | 6 |
| Antidiabetics (A10) | 6 | 12.2 | 3 | 4.5 |
| Cortisone (H02AB) | 2 | 4.1 | 3 | 4.5 |
| Diuretics (C03) | 4 | 8.2 | 3 | 4.5 |
| Statins (C01AA) | 3 | 6.1 | 2 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Halling, F.; Lutz, R.; Meisgeier, A. Oral Side Effects of the Most Commonly Prescribed Drugs in Germany. Dent. J. 2026, 14, 83. https://doi.org/10.3390/dj14020083
Halling F, Lutz R, Meisgeier A. Oral Side Effects of the Most Commonly Prescribed Drugs in Germany. Dentistry Journal. 2026; 14(2):83. https://doi.org/10.3390/dj14020083
Chicago/Turabian StyleHalling, Frank, Rainer Lutz, and Axel Meisgeier. 2026. "Oral Side Effects of the Most Commonly Prescribed Drugs in Germany" Dentistry Journal 14, no. 2: 83. https://doi.org/10.3390/dj14020083
APA StyleHalling, F., Lutz, R., & Meisgeier, A. (2026). Oral Side Effects of the Most Commonly Prescribed Drugs in Germany. Dentistry Journal, 14(2), 83. https://doi.org/10.3390/dj14020083








