Changes in the Position of Anatomical Points, Cranio-Cervical Posture, and Nasopharyngeal Airspace Dimensions in Complete Denture Wearers—A Cephalometric Pilot Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Predictor and Outcome Variables
2.4. Data Collection and Measurement
2.5. Statistical Analysis
3. Results
3.1. Demographic Data
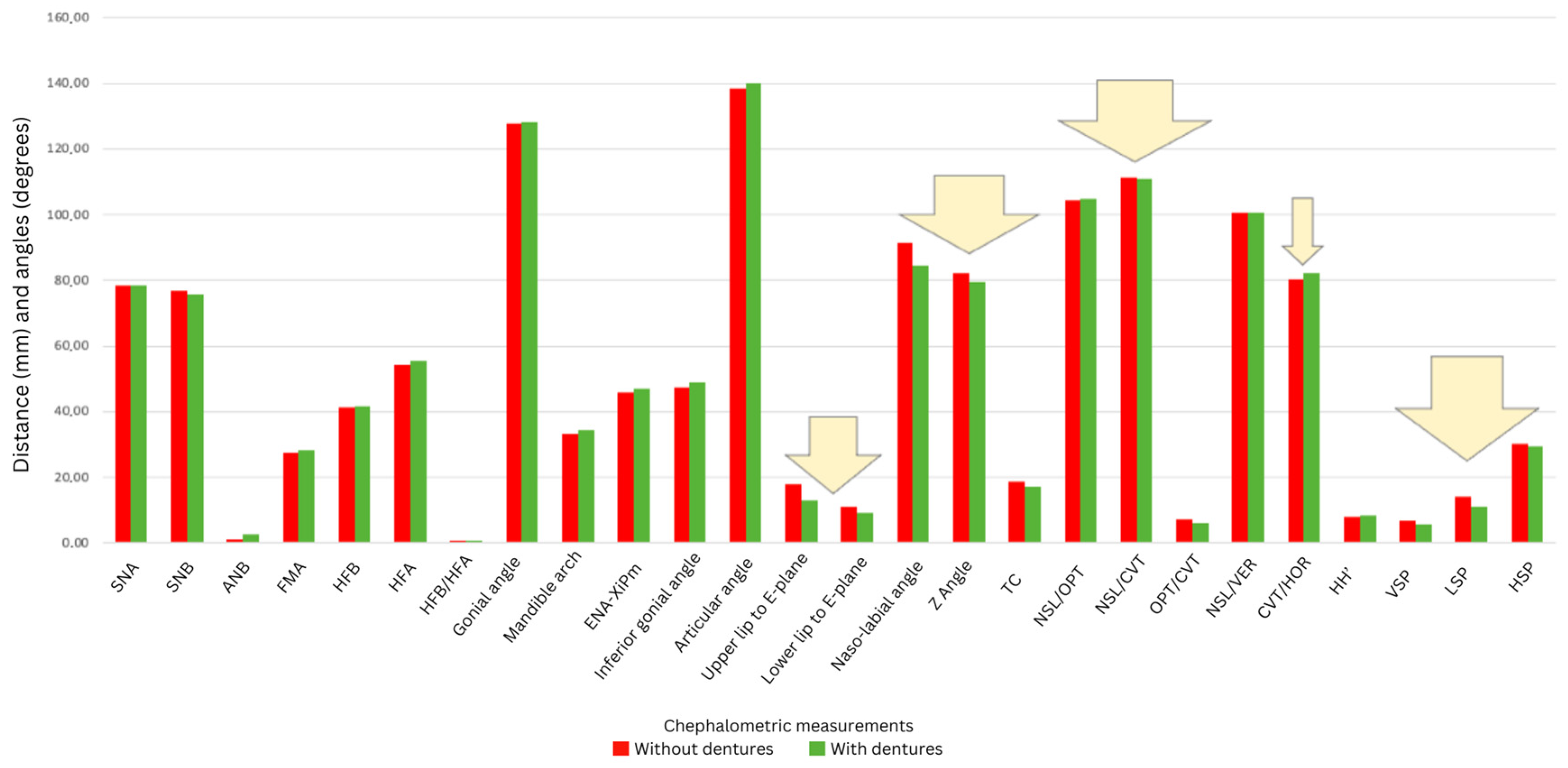
3.2. Overview of Cephalometric Changes
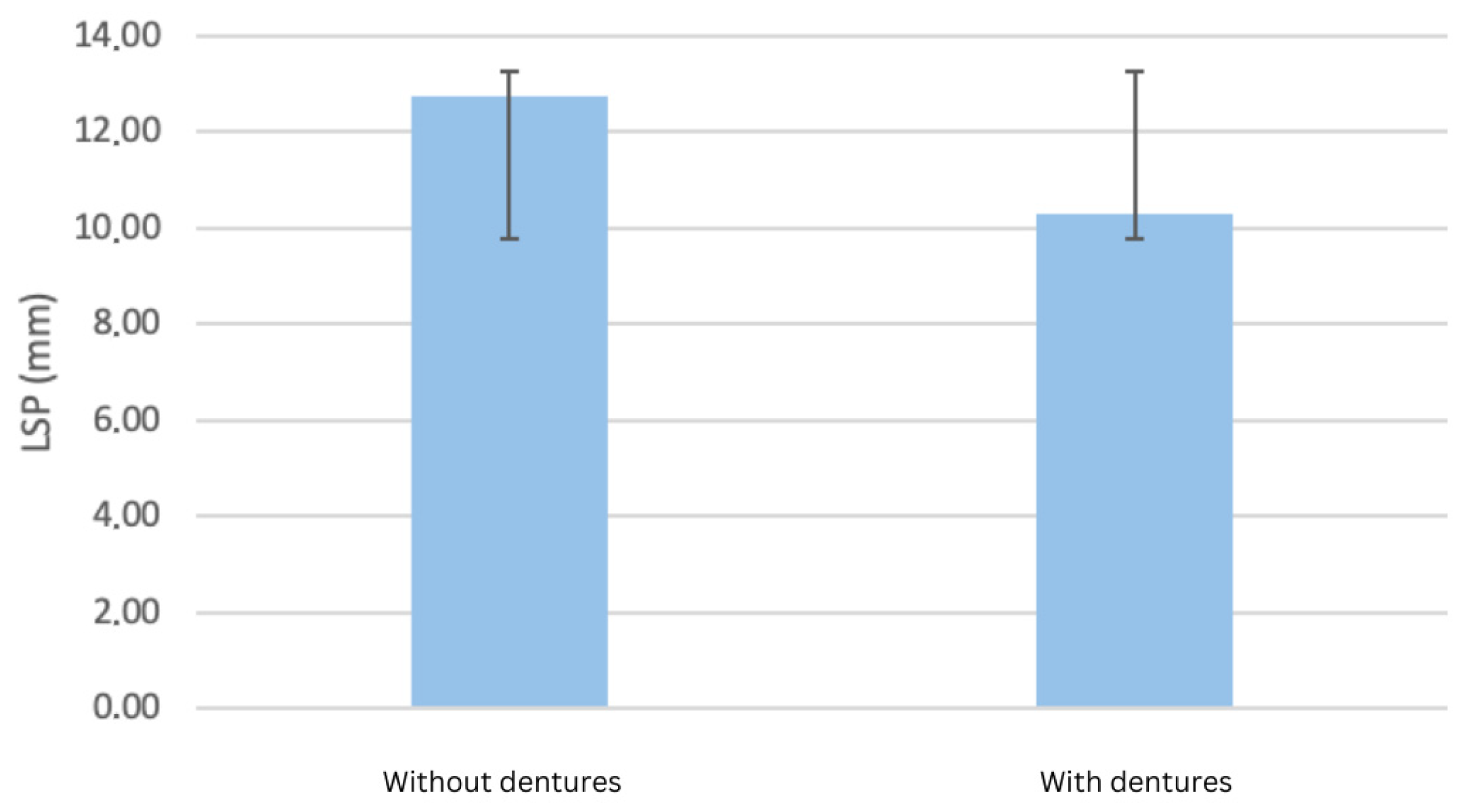
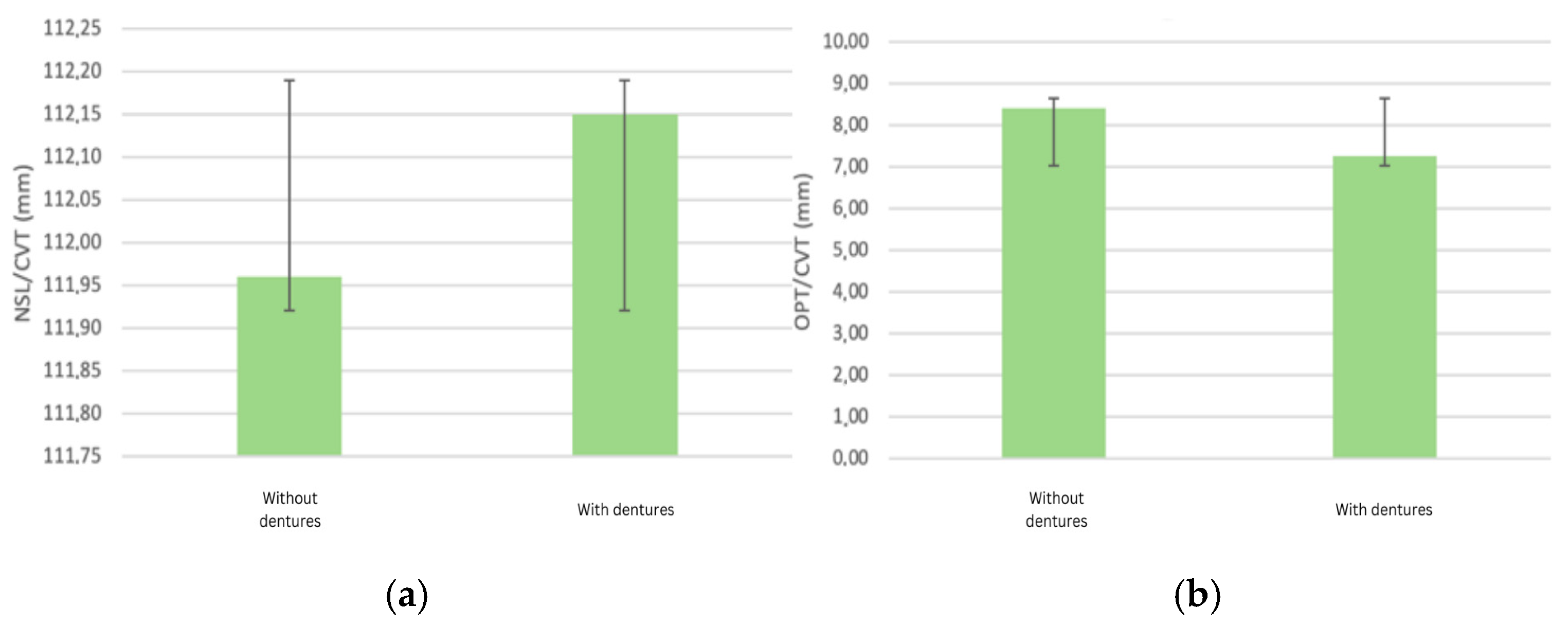
3.3. Cranio-Cervical Posture Changes
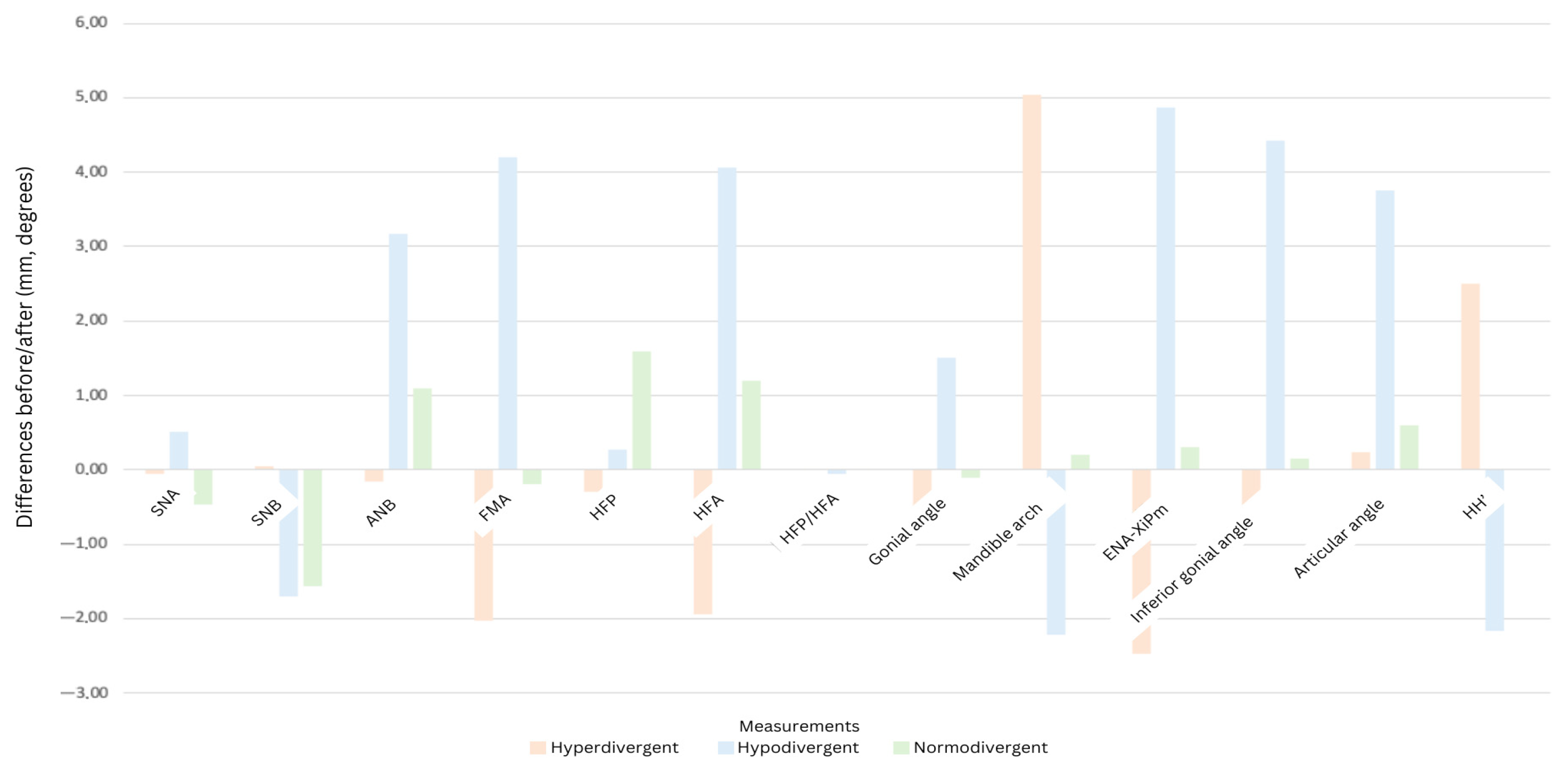
3.4. Skeletal Typology-Dependent Changes
3.5. Limitations
4. Discussion
4.1. Limitations of This Study
4.2. Future Research Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations Population Fund. Caring for Our Elders: Early Responses; United Nations Population Fund: New Delhi, India, 2017. [Google Scholar]
- Cunha-Cruz, J.; Hujoel, P.P.; Nadanovsky, P. Secular Trends in Socio-Economic Disparities in Edentulism: USA, 1972–2001. J. Dent. Res. 2007, 86, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Mckenna, G.; Burke, F.M. Age-Related Oral Changes. Dent. Update 2010, 37, 519–523. [Google Scholar] [CrossRef] [PubMed]
- Sunstar GUM. Prevalence and Burden of Periodontitis and Edentulism. Available online: https://professional.sunstargum.com/en-en/news-events/prevalence-and-burden-of-periodontitis-and-edentulism.html (accessed on 2 June 2025).
- Chen, H.M.; Shen, K.; Ji, L.; McGrath, C.; Chen, H. Global and Regional Patterns in Edentulism (1990–2021) with Projections to 2040. Int. Dent. J. 2025, 75, 735–743. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC11976601/ (accessed on 2 June 2025). [CrossRef] [PubMed]
- World Health Organization. Oral Health Country Profile: Romania; World Health Organization: Geneva, Switzerland, 2022; Available online: https://cdn.who.int/media/docs/default-source/country-profiles/oral-health/oral-health-rou-2022-country-profile.pdf (accessed on 2 June 2025).
- Basno, A.; Maxim, A.; Savin, C.; Balcos, C.; Tatarciuc, M.S. Prevalence of Edentulism and Related Social-Behavioural Factors among Young Adults of Iași, Romania. Int. J. Med. Dent. 2016, 20, 214–222. [Google Scholar]
- Michelotti, A.; Buonocore, G.; Manzo, P.; Pellegrino, G.; Farella, M. Dental Occlusion and Posture: An Overview. Prog. Orthod. 2011, 12, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Manni, B.; Neri, M.; Chiesa, R.; Rossi, F.; Presicce, M.C.; Martini, E. Postural Sways Related to Stomatognathic Proprioception in Elderly. Arch. Gerontol. Geriatr. 2007, 44, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, I. Influence of Wearing Complete Dentures on Body Balance in Edentulous Elderly. Kokubyo Gakkai Zasshi 1999, 66, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Fujinami, Y.; Hayakawa, I.; Hirano, S.; Watanabe, I. Changes in Postural Control of Complete Denture Wearers After Receiving New Dentures—Gait and Body Sway. Prosthodont. Res. Pract. 2003, 2, 11–19. [Google Scholar] [CrossRef][Green Version]
- Okubo, M.; Fujinami, Y.; Minakuchi, S. Effect of Complete Dentures on Body Balance During Standing and Walking in Elderly People. J. Prosthodont. Res. 2010, 54, 42–47. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, L.; Cajaiba, F.; Costa, W.; Rocabado, M.; Lazo-Osorio, R.; Ribeiro, S. Comparative analysis of assessment of the craniocervical equilibrium through two methods: Cephalomotry of Rocabado and cervical range of Motion. Work 2012, 41, 2563–2568. [Google Scholar] [CrossRef] [PubMed]
- Cimmy, A.; Anil, K.G.; Nayana, P.; Sowmya, N.; Raghavendra, S. Prosthetic Rehabilitation and Its Effect on Head Posture. Cureus 2011, 14, 4. [Google Scholar]
- Abduo, J.K. Lyons. Clinical Considerations for Increasing Occlusal Vertical Dimension: A Review. Aust. Dent. J. 2012, 57, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Hasan Suat, G.; Gokce, S.M.; Akin, E.; Bengi, O. Effects of Complete Denture Wearing on the Head Posture and Posterior Airway Space: A Cephalometric Study. J. Dent. Sci. 2011, 6, 6–13. [Google Scholar] [CrossRef]
- Orthlieb, J.-D.; Laurent, M.; Laplanche, O. Cephalometric Estimation of Vertical Dimension of Occlusion. J. Oral Rehabil. 2000, 27, 802–807. [Google Scholar] [CrossRef] [PubMed]
- Neves, B.R.; Leão, R.S.; da Silva, A.S.C.; Junior, J.F.S.; do Egito Vasconcelos, B.C.; Pellizzer, E.P.; Moraes, S.L.D. Influence of complete denture use on respiratory capacity: A systematic review. J. Contemp. Dent. Pract. 2021, 22, 1197–1205. [Google Scholar] [PubMed]
- Gowda, M.; Sahoo, N.K.; Guruprasada, N.K.; Verma, K. Evaluation of Denture Wear on Upper Airway Dimensions and Oxygen Saturation in Completely Edentulous Patients. J. Sleep. Disord. Ther. 2016, 5, 254. [Google Scholar]
- Joanna, K.; Teresa, S.; Maria, G. Evaluation of functional parameters in the occlusion of complete denture wearers before and after prosthetic treatment. J. Prosthodont. Res. 2017, 61, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Tecco, S.; Tete, S.; Festa, F. Relation Between Cervical Posture on Lateral Skull Radiographs and Electromyographic Activity of Masticatory Muscles in Caucasian Adult Women: A Cross-Sectional Study. J. Oral Rehabil. 2007, 34, 652–662. [Google Scholar] [CrossRef] [PubMed]
- Muto, T.; Yamazaki, S.; Takeda, A. A Cephalometric Evaluation of the Pharyngeal Airway Space in Patients with Mandibular Retrognathia and Prognathia, and Normal Subjects. Int. J. Oral Maxillofac. Surg. 2008, 37, 228–231. [Google Scholar] [CrossRef] [PubMed]
- Almășan, O.; Kui, A.; Duncea, I.; Manea, A.; Buduru, S. Temporomandibular Joint Disk Displacements in Class II Malocclusion and Cervical Spine Alterations: Systematic Review and Report of a Hypodivergent Case with MRI Bone and Soft Tissue Changes. Life 2022, 12, 908. [Google Scholar] [CrossRef] [PubMed]
- Anegawa, E.; Tsuyama, H.; Kusukawa, J. Lateral Cephalometric Analysis of the Pharyngeal Airway Space Affected by Head Posture. Int. J. Oral Maxillofac. Surg. 2008, 37, 805–809. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Zhang, S.; Xu, J. Impact of Occlusal Reconstruction Positions on Airway Dimensions in Patients with Edentulism and Long Centric Occlusion. BMC Oral Health 2023, 23, 215. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Masayasu, I.; Yasuhiko, K. Dentures Wearing Reduce Motion Artifacts Related to Tongue Movement in Magnetic Resonance Imaging. J. Prosthodont. Res. 2018, 62, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, G.; Sorrentino, R.; Grande, F.; Nuytens, P.; Zarone, F. Jaw Motion Tracking with Open-Source Tools: A Dental Technique. J. Prosthet. Dent. 2025, in press. [Google Scholar] [CrossRef] [PubMed]
- Gismondi, S.; Ruggiero, G.; Bollero, R.; Ferrarelli, E.; Zarone, F.; Sorrentino, R. A Digital Technique for Fabricating a Diagnostic Occlusal Device Using Mandibular Motion Tracking. Digit. Dent. J. 2025, 1, 100012. [Google Scholar] [CrossRef]
| Abbreviation | Full Description |
|---|---|
| NSL | Nasion-sella line (cranial base reference line) |
| CVT | Cervical vertebra tangent (line tangent to cervical vertebrae curvature) |
| OPT | Odontoid process tangent (line tangent to odontoid process curvature) |
| VDO | Vertical dimension of occlusion |
| VPS | Velopharyngeal space (nasopharynx) |
| LPS | Lingual pharyngeal space (oropharynx) |
| HPS | Hypopharyngeal space (laryngopharynx) |
| FMA | Frankfort–mandibular plane angle |
| HFP/HFA | Height facial posterior/height facial anterior ratio |
| ENA-Xi-Pm | Angle formed by anterior nasal spine, Xi point, and protuberance mentis |
| HH’ | Distance between hyoid bone and mandibular plane |
| SNB | Angle formed by the sella-nasion and nasion-B point |
| Pn | Pronasale |
| Pog’ | Soft tissue pogonion |
| Characteristic | Value |
|---|---|
| Number of participants | 12 |
| Age (mean ± SD) | 65 ± 5.2 years (range: 55–75) |
| Gender | Male: 5 (41.7%), Female: 7 (58.3%) |
| Skeletal typology | Hyperdivergent: 4 (33.3%) Normodivergent: 2 (16.7%) Hypodivergent: 6 (50.0%) |
| Follow-up period | 6 months (post-treatment evaluation) |
| Measurement | Hyperdivergent Without | Hyperdivergent With | Hypodivergent Without | Hypodivergent With | Normodivergent Without | Normodivergent With | Difference Hyper. | Difference Hypo. | Difference Normo. |
|---|---|---|---|---|---|---|---|---|---|
| SNA | 77.98 | 77.93 | 78.59 | 79.10 | 78.15 | 77.68 | −0.05 | 1.70 | −0.47 |
| SNB | 75.16 | 75.21 | 75.37 | 73.67 | 79.70 | 78.14 | 0.05 | −1.70 | −1.56 |
| ANB | 2.83 | 2.67 | 2.22 | 5.39 | −1.60 | −0.50 | −0.16 | 3.17 | 1.10 |
| FMA | 34.35 | 32.33 | 30.23 | 24.83 | 27.60 | 27.40 | −2.02 | −5.40 | −0.20 |
| HFP | 40.55 | 40.55 | 43.97 | 44.23 | 39.40 | 41.00 | 0.00 | 0.27 | 1.60 |
| HFA | 57.75 | 55.80 | 49.80 | 53.87 | 55.80 | 57.00 | −1.95 | 4.07 | 1.20 |
| HFP/HFA | 0.71 | 0.73 | 0.88 | 0.82 | 0.71 | 0.73 | 0.02 | −0.06 | 0.02 |
| Gonial angle | 133.61 | 133.11 | 120.33 | 121.74 | 129.40 | 129.30 | −0.50 | 1.51 | −0.10 |
| Mandibular arch | 26.05 | 31.09 | 38.66 | 36.43 | 35.40 | 35.50 | 5.04 | −2.22 | 0.20 |
| ENA-XiPm | 52.89 | 50.42 | 40.76 | 45.63 | 45.63 | 44.50 | −2.47 | 4.87 | −1.13 |
| Lower gonial angle | 51.38 | 50.75 | 44.35 | 48.78 | 46.90 | 47.05 | −0.63 | 4.43 | 0.15 |
| Articular angle | 137.18 | 137.42 | 138.73 | 142.48 | 139.10 | 139.70 | 0.24 | 3.75 | 0.60 |
| Upper lip to E-plane | 18.87 | 15.17 | 15.26 | 12.20 | 19.80 | 13.88 | −3.70 | −3.06 | −5.92 |
| Lower lip to E-plane | 9.66 | 10.15 | 13.80 | 8.22 | 8.22 | 8.90 | 0.49 | −5.58 | −1.30 |
| Nasolabial angle | 99.96 | 88.13 | 91.21 | 100.90 | 83.50 | 65.00 | −11.83 | 9.69 | −18.50 |
| Angle Z | 84.20 | 86.25 | 82.86 | 74.49 | 78.00 | 78.20 | 2.05 | −8.37 | −2.20 |
| TC | 23.30 | 21.91 | 16.73 | 14.77 | 15.70 | 15.20 | −1.40 | −1.97 | −0.50 |
| NSL/OPT | 105.88 | 105.70 | 101.20 | 104.30 | 106.00 | 105.00 | −0.18 | 3.10 | −1.00 |
| NSL/CVT | 118.13 | 114.95 | 109.97 | 111.73 | 106.50 | 106.00 | −3.18 | 2.07 | −0.50 |
| OPT/CVT | 12.30 | 9.35 | 8.47 | 7.43 | 10.50 | 9.00 | −2.95 | −1.03 | −1.50 |
| NSL/VER | 100.18 | 100.10 | 101.07 | 101.87 | 99.50 | 99.50 | −0.08 | 0.80 | 0.00 |
| CVT/HOR | 72.90 | 75.20 | 85.67 | 85.03 | 82.60 | 86.50 | 2.30 | −0.64 | 3.90 |
| HH’ | 9.00 | 11.50 | 5.00 | 2.83 | 5.10 | 3.10 | 2.50 | −2.17 | −1.90 |
| VSP | 4.30 | 4.40 | 4.70 | 5.80 | 8.40 | 7.10 | 0.10 | 1.50 | −1.30 |
| LSP | 11.95 | 10.10 | 10.83 | 9.23 | 20.10 | 13.70 | −1.85 | −1.60 | −6.40 |
| HSP | 33.00 | 31.79 | 26.20 | 26.00 | 31.70 | 30.80 | −1.22 | −0.20 | −0.90 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chisnoiu, A.M.; Hedeșiu, M.; Chira, O.; Bara, I.; Iacob, S.; Kui, A.; Buduru, S.; Păstrav, M.; Fluerașu, M.; Chisnoiu, R. Changes in the Position of Anatomical Points, Cranio-Cervical Posture, and Nasopharyngeal Airspace Dimensions in Complete Denture Wearers—A Cephalometric Pilot Study. Dent. J. 2025, 13, 335. https://doi.org/10.3390/dj13080335
Chisnoiu AM, Hedeșiu M, Chira O, Bara I, Iacob S, Kui A, Buduru S, Păstrav M, Fluerașu M, Chisnoiu R. Changes in the Position of Anatomical Points, Cranio-Cervical Posture, and Nasopharyngeal Airspace Dimensions in Complete Denture Wearers—A Cephalometric Pilot Study. Dentistry Journal. 2025; 13(8):335. https://doi.org/10.3390/dj13080335
Chicago/Turabian StyleChisnoiu, Andrea Maria, Mihaela Hedeșiu, Oana Chira, Iris Bara, Simona Iacob, Andreea Kui, Smaranda Buduru, Mihaela Păstrav, Mirela Fluerașu, and Radu Chisnoiu. 2025. "Changes in the Position of Anatomical Points, Cranio-Cervical Posture, and Nasopharyngeal Airspace Dimensions in Complete Denture Wearers—A Cephalometric Pilot Study" Dentistry Journal 13, no. 8: 335. https://doi.org/10.3390/dj13080335
APA StyleChisnoiu, A. M., Hedeșiu, M., Chira, O., Bara, I., Iacob, S., Kui, A., Buduru, S., Păstrav, M., Fluerașu, M., & Chisnoiu, R. (2025). Changes in the Position of Anatomical Points, Cranio-Cervical Posture, and Nasopharyngeal Airspace Dimensions in Complete Denture Wearers—A Cephalometric Pilot Study. Dentistry Journal, 13(8), 335. https://doi.org/10.3390/dj13080335










