Resin Composite Surface Pre-Reacted Glass-Ionomer (S-PRG) Filler for Non-Carious Cervical Lesions: A Double-Blinded, Randomized, Split-Mouth Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Considerations
2.2. Sample Size Calculation and Randomization
2.3. Inclusion and Exclusion Criteria
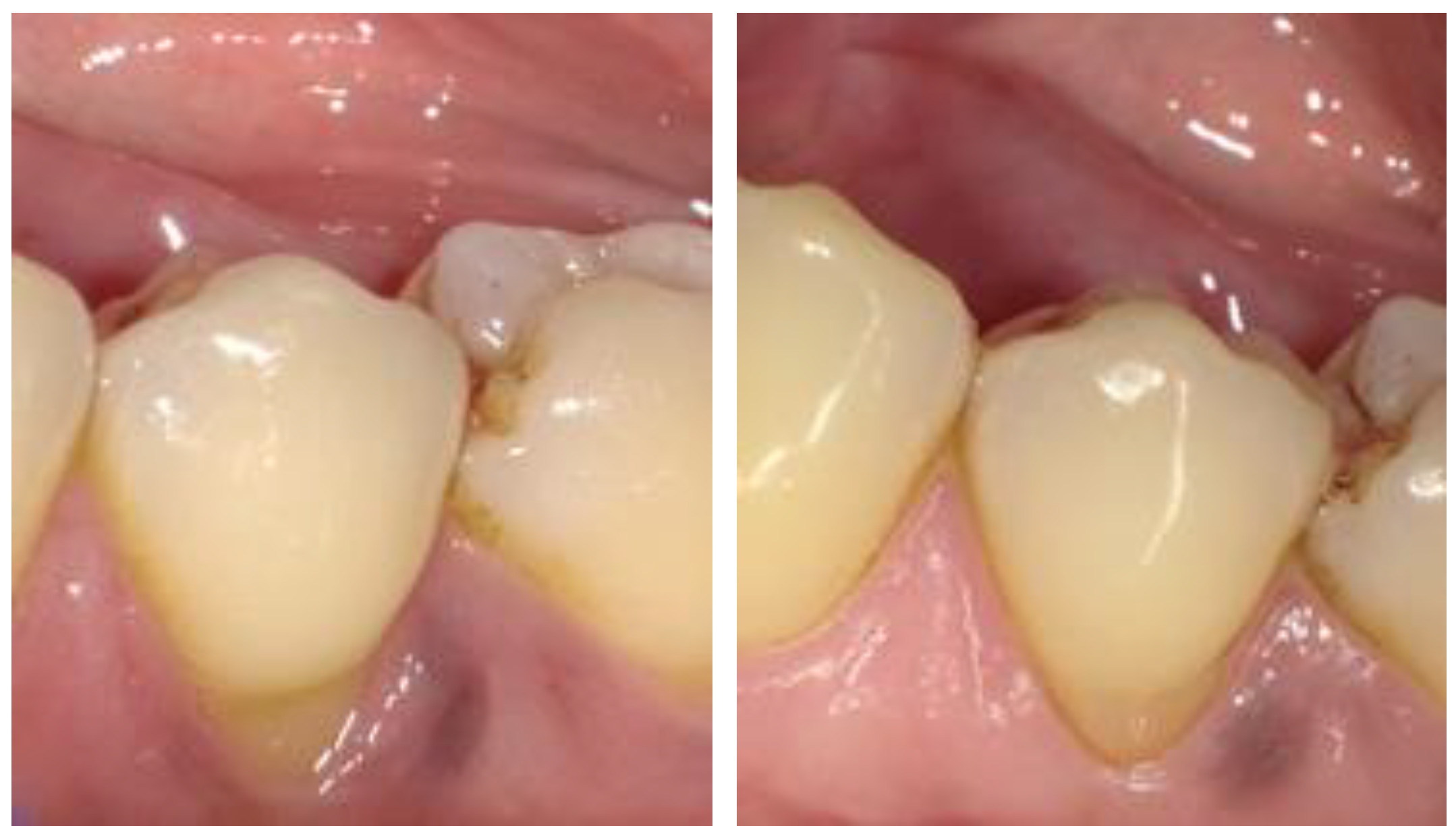
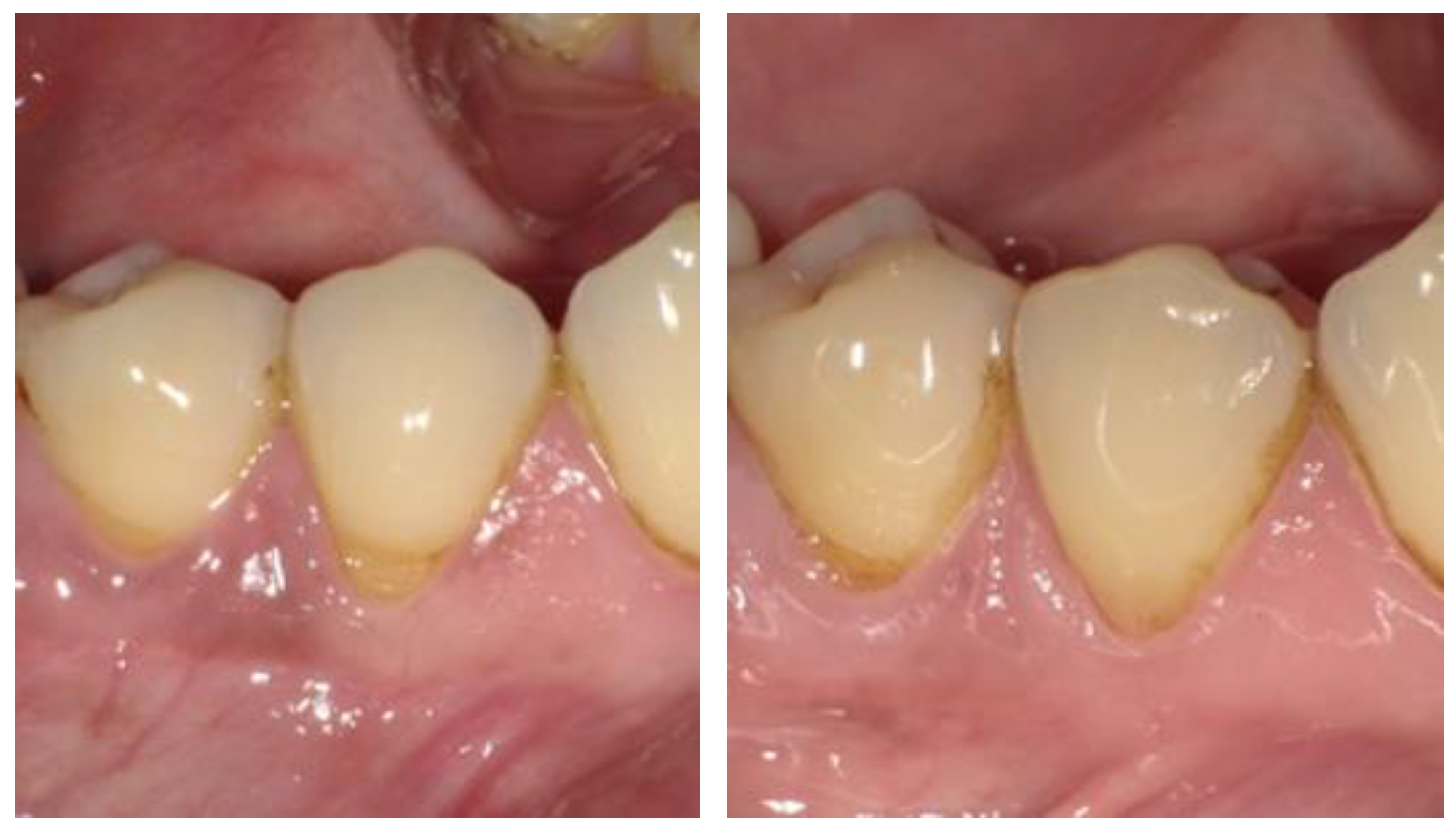
2.4. Recruitment of Subjects and Clinical Procedures
| Shofu BL II LS [11] | 3M FS Supreme Universal [13] |
|---|---|
| Low-shrinkage urethane diacrylate, Bis-GMA, Bis-MPEPP, TEGDMA, S-PRG filler, multi-functional glass filler, pre-polymerized filler, nano-filler, photoinitiator, etc. | Bis-GMA, UDMA, TEGDMA, Bis-EMA(6) non-agglomerated/non-aggregated 20 nm silica filler, non-agglomerated/non-aggregated zirconia filler, and aggregated zirconia/silica cluster filler |
| BeautiBond [14] | 3M Scotch Universal Bond [15] |
| Acetone, Bis-GMA, TEGDMA, phosphonic acid monomer, carboxylic acid monomer, water, photoinitiator, polymeric monomer, HEMA-free, etc. | MDP phosphate monomer, dimethacrylate resins, HEMA, Vitrebond™ copolymer, filler, ethanol, water, initiators, silane |
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yoshizaki, K.; Francisconi-dos-Rios, L.F.; Sobral, M.A.P.; Aranha, A.C.C.; Mendes, F.M.; Scaramucci, T. Clinical Features and Factors Associated With Non-carious Cervical Lesions and Dentin Hypersensitivity. J. Oral Rehabil. 2017, 44, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Haralur, S.B.; Alqahtani, A.S.; AlMazni, M.S.; Alqahtani, M.K. Association of Non-Carious Cervical Lesions with Oral Hygiene Habits and Dynamic Occlusal Parameters. Diagnostics 2019, 9, 43. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Lima, R.; Ribeiro, S.N.; de Moura, J.N.; Lopes, A.; Silva, I.Q.; da Rocha, D.M.; de Oliveira-Vanderlei, K.M. Biomechanics of Non-Carious Cervical Lesions in Finite Element Models: An Integrative Review. Rev. Flum. Odontol. 2021, 74–87. [Google Scholar] [CrossRef]
- Dige, I.; Grønkjær, L.; Nyvad, B. Molecular Studies of the Structural Ecology of Natural Occlusal Caries. Caries Res. 2014, 48, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Rojas, P.A.D. Relationship Between Extrinsic Factors and Non-Carious Cervical Lesions in Patients of the National Hospital “Hipólito Unánue”. Braz. J. Oral Sci. 2021, 20, e211632. [Google Scholar] [CrossRef]
- Teixeira, D.N.R.; Zeola, L.F.; Machado, A.C.; Gomes, R.R.; Souza, P.G.; Mendes, D.C.; Soares, P.V. Relationship Between Noncarious Cervical Lesions, Cervical Dentin Hypersensitivity, Gingival Recession, and Associated Risk Factors: A Cross-Sectional Study. J. Dent. 2018, 76, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Vandana, K.L.; Haneet, R.K. Cementoenamel Junction: An Insight. J. Indian Soc. Periodontol. 2014, 18, 549. [Google Scholar] [CrossRef] [PubMed]
- Heasman, P.A.; Holliday, R.; Bryant, A.; Preshaw, P.M. Evidence for the Occurrence of Gingival Recession and Non-carious Cervical Lesions as a Consequence of Traumatic Toothbrushing. J. Clin. Periodontol. 2015, 42, S237–S255. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Wu, C.; Abrams, W.; Li, Y. Structural and Functional Characteristics of the Microbiome in Deep-Dentin Caries. J. Dent. Res. 2020, 99, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Kubo, S.; Yokota, H.; Yokota, H.; Hayashi, Y. Three-Year Clinical Evaluation of a Flowable and a Hybrid Resin Composite in Non-Carious Cervical Lesions. J. Dent. 2010, 38, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Gordan, V.V.; Blaser, P.K.; Watson, R.E.; Mjör, I.A.; McEdward, D.L.; Sensi, L.G.; Riley, J.L., III. A clinical evaluation of a giomer restorative system containing surface prereacted glass ionomer filler: Results from a 13-year recall examination. J. Am. Dent. Assoc. 2014, 145, 1036–1043. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.H.; Magnuson, B.E.; Singh, M.L.S.; Tran, D.L.; Pagni, S.E.; Perry, R.D.; Kugel, G. 18-Month Clinical Comparison of Giomer Based and Nano Technology Based Materials in Non-Carious Cervical Lesion Class V Restorations. J. Dent. Sci. 2021, 6, 1–17. [Google Scholar] [CrossRef]
- Filtek. Supreme Ultra Technical Product Profile. Available online: https://multimedia.3m.com/mws/media/1363018O/3m-filtek-supreme-ultra-universal-restorative-technical-product-profile.pdf (accessed on 18 September 2024).
- Shofu. Giomer Technology. Available online: https://www.shofu.com/wp-content/uploads/Giomer-Brochure.pdf (accessed on 18 September 2024).
- 3M. 3MTM ScotchbondTM Universal Adhesive: Technical Product Profile. Available online: https://multimedia.3m.com/mws/media/1279638O/3m-scotchbond-universal-adhesive-technical-product-profile.pdf (accessed on 18 September 2024).
- Hickel, R.; Peschke, A.; Tyas, M.; Mjör, I.; Bayne, S.; Peters, M.; Hiller, K.A.; Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation: Clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin. Oral Investig. 2010, 14, 349–366. [Google Scholar] [CrossRef] [PubMed]
- Patano, A.; Marinelli, G.; Santis, M.D.; Morolla, R.; Settanni, V.; Piras, F.; Inchingolo, A.D.; Mancini, A.; Inchingolo, F.; Dipalma, G.; et al. Conservative Treatment of Dental Non-Carious Cervical Lesions: A Scoping Review. Biomedicines 2023, 11, 1530. [Google Scholar] [CrossRef] [PubMed]
- Battancs, E.; Fráter, M.; Sáry, T.; Gál, E.; Braunitzer, G.; Szabó, B.; Garoushi, S. Fracture Behavior and Integrity of Different Direct Restorative Materials to Restore Noncarious Cervical Lesions. Polymers 2021, 13, 4170. [Google Scholar] [CrossRef] [PubMed]
- Imazato, S.; Nakatsuka, T.; Kitagawa, H.; Sasaki, J.I.; Yamaguchi, S.; Ito, S.; Takeuchi, H.; Nomura, R.; Nakano, K. Multiple-Ion Releasing Bioactive Surface Pre-Reacted Glass-Ionomer (S-PRG) Filler: Innovative Technology for Dental Treatment and Care. J. Funct. Biomater. 2023, 14, 236. [Google Scholar] [CrossRef] [PubMed]

| Participants | n = 34 |
|---|---|
| Sex | |
| Male | 18 |
| Female | 16 |
| Age (years), Mean ± Standard Deviation | 55.88 ± 14.72 |
| Smoker | 5 |
| Ethnicity | |
| Native American | 0 |
| Hispanic/Latino | 3 |
| Asian | 5 |
| Black | 7 |
| White | 16 |
| Prefer Not to Answer | 3 |
| Hickel Criteria | Visit | BL Hickel Scores | FS Hickel Scores | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| Esthetic Properties | Surface Luster | Baseline | 49 | 49 | ||||||||
| 48 months | 30 | 3 | 27 | 4 | 1 | |||||||
| Surface Staining | Baseline | 49 | 49 | |||||||||
| 48 months | 26 | 6 | 1 | 26 | 5 | 1 | ||||||
| Marginal Staining | Baseline | 49 | 48 | 1 | ||||||||
| 48 months | 22 | 7 | 3 | 1 | 22 | 7 | 1 | 2 | ||||
| Color Match | Baseline | 46 | 3 | 44 | 5 | |||||||
| 48 months | 24 | 6 | 2 | 1 | 23 | 6 | 2 | 1 | ||||
| Anatomical Form | Baseline | 48 | 1 | 49 | ||||||||
| 48 months | 33 | 30 | 1 | 1 | ||||||||
| Functional Properties | Fracture of Material and Retention | Baseline | 49 | 49 | ||||||||
| 48 months | 33 | 1 | 31 | 1 | 1 | |||||||
| Marginal Adaptation | Baseline | 48 | 1 | 49 | ||||||||
| 48 months | 19 | 13 | 1 | 18 | 12 | 1 | 1 | |||||
| Patient’s View | Baseline | 49 | 49 | |||||||||
| 48 months | 32 | 1 | 31 | 1 | ||||||||
| Biological Properties | Recurrence of Caries | Baseline | 49 | 49 | ||||||||
| 48 months | 27 | 1 | 1 | 3 | 1 | 26 | 4 | 1 | 1 | |||
| Tooth Integrity | Baseline | 49 | 49 | |||||||||
| 48 months | 32 | 1 | 32 | |||||||||
| Adjacent Mucosa | Baseline | 48 | 1 | 48 | 1 | |||||||
| 48 months | 21 | 8 | 5 | 23 | 6 | 4 | ||||||
| BL Hickel Scores | FS Hickel Scores | ||||||
|---|---|---|---|---|---|---|---|
| Hickel Criteria | Baseline Median (IQR) | 48 Months Median (IQR) | p-Value | Baseline Median (IQR) | 48 Months Median (IQR) | p-Value | |
| Esthetic | Surface Luster | 1 (0) | 1 (0) | 0.11 | 1 (0) | 1 (0) | 0.07 |
| Surface Staining | 1 (0) | 1 (0) | 0.8 | 1 (0) | 1 (0) | 0.03 * | |
| Marginal Staining | 1 (0) | 1 (1) | <0.001 * | 1 (0) | 1 (1) | 0.008 * | |
| Color Match | 1 (0) | 1 (0) | 0.12 | 1 (0) | 1 (0.5) | 0.09 | |
| Anatomical Form | 1 (0) | 1 (0) | >0.99 | 1 (0) | 1 (0) | >0.99 | |
| Functional | Fracture of Material and Retention | 1 (0) | 1 (0) | >0.99 | 1 (0) | 1 (0) | >0.99 |
| Marginal Adaptation | 1 (0) | 1 (1) | <0.001 * | 1 (0) | 1 (1) | <0.001 * | |
| Patient’s View | 1 (0) | 1 (1) | >0.99 | 1 (0) | 1 (1) | >0.99 | |
| Biological | Recurrence of Caries | 1 (0) | 1 (0) | 0.01 * | 1 (0) | 1 (0) | 0.04 * |
| Tooth Integrity | 1 (0) | 1 (0) | >0.99 | 1 (0) | 1 (0) | >0.99 | |
| Adjacent Mucosa | 1 (0) | 1 (1) | <0.001 * | 1 (0) | 1 (1) | <0.001 * | |
| 0 Month | 48 Months | |
|---|---|---|
| Surface Luster | = | FS |
| Surface Stain | = | BL |
| Marginal Stain | FS | FS |
| Color Match and Translucency | FS | FS |
| Esthetic Anatomical Form | BL | FS |
| Fracture of Material and Retention | = | FS |
| Marginal Adaptation | BL | FS |
| Radiographic Examination (when applicable) | n/a | = |
| Patient’s View | = | = |
| Postoperative (Hyper-)Sensitivity and Tooth Vitality | n/a | = |
| Recurrence of Caries, Erosion, Abfraction | = | = |
| Tooth Integrity (Enamel Cracks, Tooth Fractures) | = | = |
| Adjacent Mucosa | = | BL |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lowenstein, A.; Mourão, C.F.; Singh, M.L.; Pagni, S.E.; Perry, R.D.; Kugel, G. Resin Composite Surface Pre-Reacted Glass-Ionomer (S-PRG) Filler for Non-Carious Cervical Lesions: A Double-Blinded, Randomized, Split-Mouth Clinical Trial. Dent. J. 2025, 13, 156. https://doi.org/10.3390/dj13040156
Lowenstein A, Mourão CF, Singh ML, Pagni SE, Perry RD, Kugel G. Resin Composite Surface Pre-Reacted Glass-Ionomer (S-PRG) Filler for Non-Carious Cervical Lesions: A Double-Blinded, Randomized, Split-Mouth Clinical Trial. Dentistry Journal. 2025; 13(4):156. https://doi.org/10.3390/dj13040156
Chicago/Turabian StyleLowenstein, Adam, Carlos Fernando Mourão, Mabi L. Singh, Sarah E. Pagni, Ronald D. Perry, and Gerard Kugel. 2025. "Resin Composite Surface Pre-Reacted Glass-Ionomer (S-PRG) Filler for Non-Carious Cervical Lesions: A Double-Blinded, Randomized, Split-Mouth Clinical Trial" Dentistry Journal 13, no. 4: 156. https://doi.org/10.3390/dj13040156
APA StyleLowenstein, A., Mourão, C. F., Singh, M. L., Pagni, S. E., Perry, R. D., & Kugel, G. (2025). Resin Composite Surface Pre-Reacted Glass-Ionomer (S-PRG) Filler for Non-Carious Cervical Lesions: A Double-Blinded, Randomized, Split-Mouth Clinical Trial. Dentistry Journal, 13(4), 156. https://doi.org/10.3390/dj13040156








