Retrospective Study of Functional and Esthetic Outcomes Using Narrow-Diameter Implants for Single Upper Central Incisor Replacements
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgical Procedure
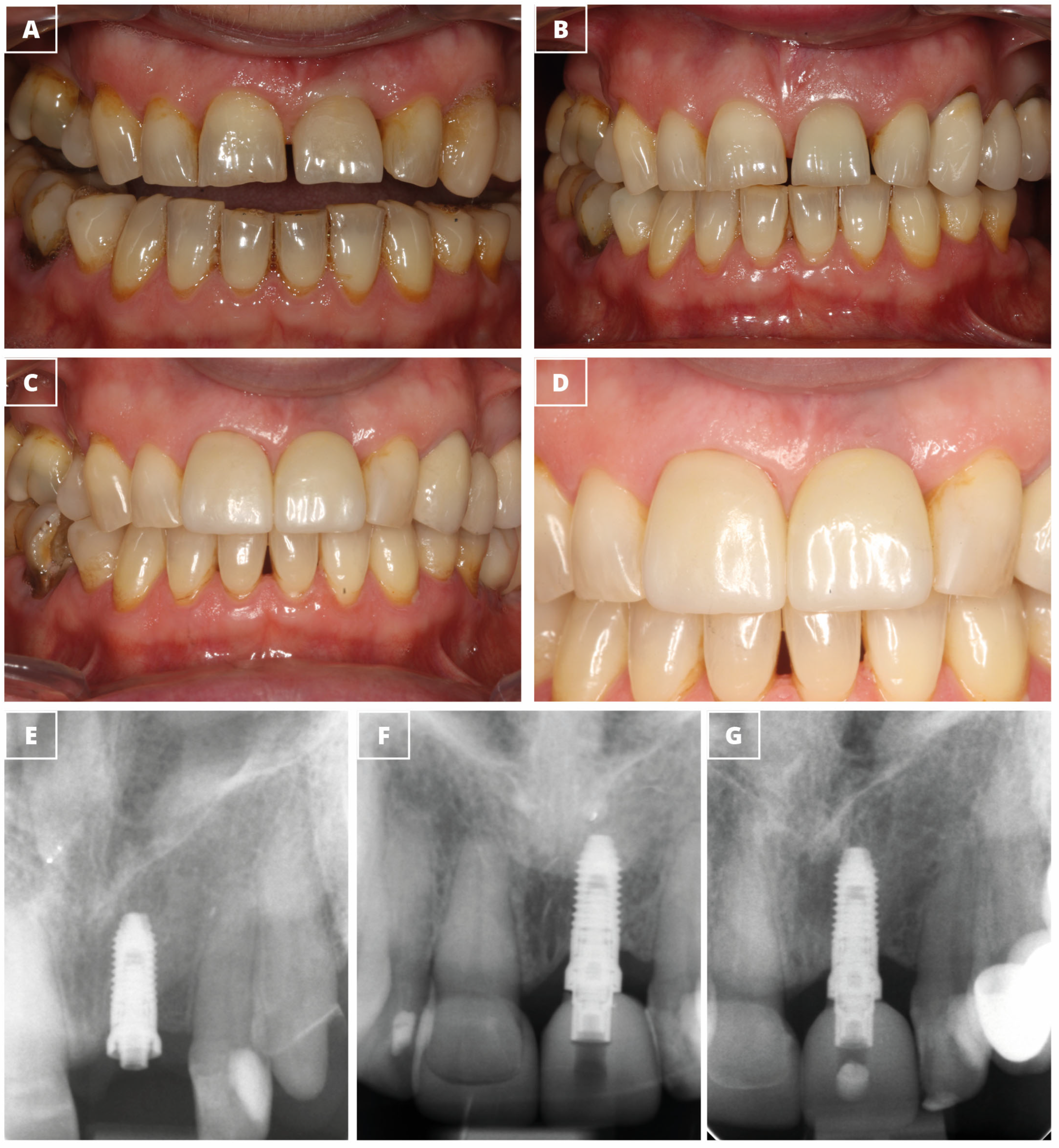
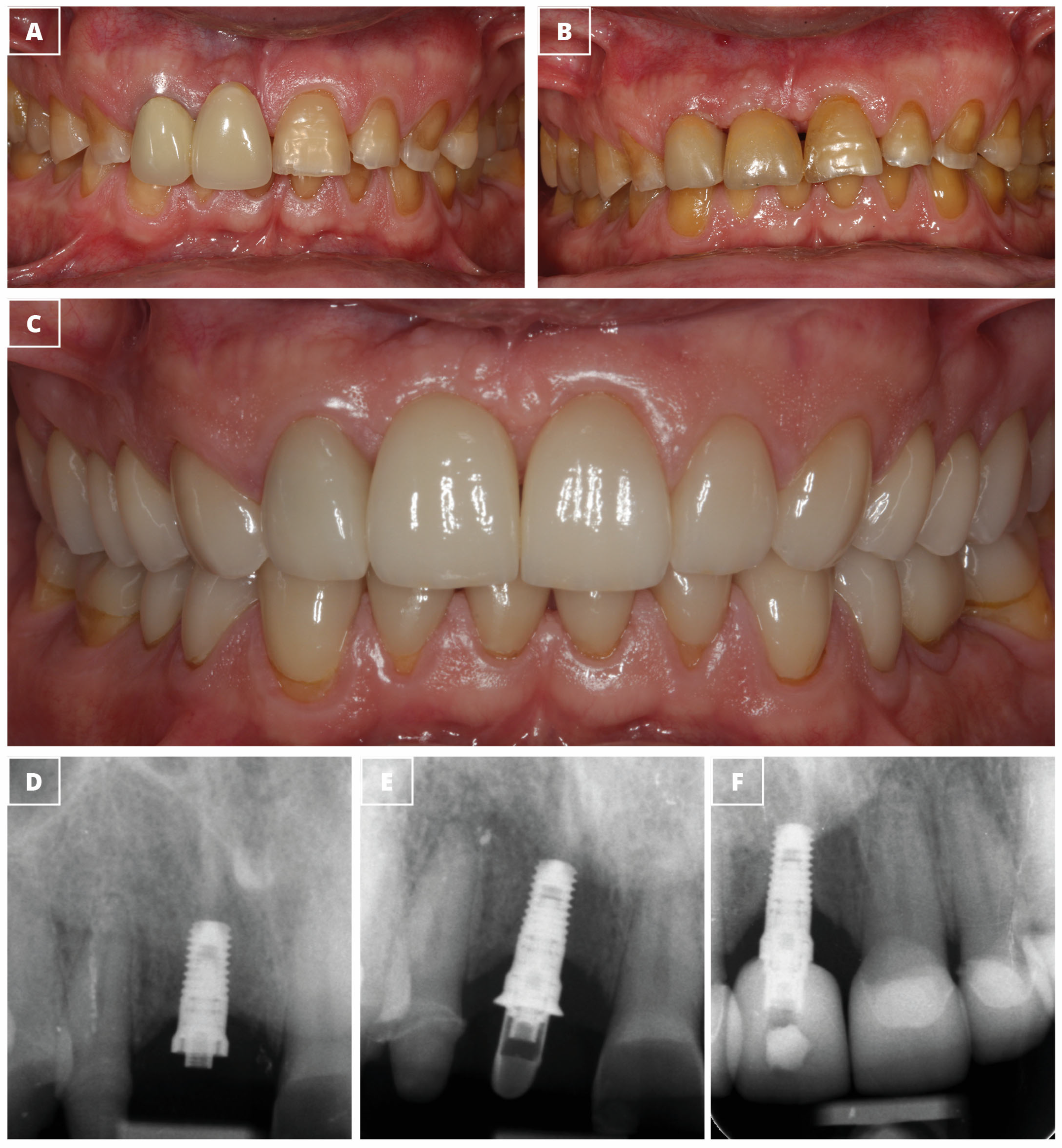
2.2. Prosthetic Rehabilitation
2.3. Study Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Del Monte, S.; Afrashtehfar, K.I.; Emami, E.; Abi Nader, S.; Tamimi, F. Lay preferences for dentogingival esthetic parameters: A systematic review. J. Prosthet. Dent. 2017, 118, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Gautam, R.; Nene, P.; Mehta, K.; Nene, S.; Hegde, A.; Jaju, R. Treatment strategies for missing maxillary central incisor—An orthodontist’s perspective. J. Prosthodont. 2014, 23, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Pithon, M.M.; Vargas, E.O.A.; da Silva Coqueiro, R.; Lacerda-Santos, R.; Tanaka, O.M.; Maia, L.C. Impact of oral-health-related quality of life and self-esteem on patients with missing maxillary lateral incisor after orthodontic space closure: A single-blinded, randomized, controlled trial. Eur. J. Orthod. 2021, 43, 208–214. [Google Scholar] [CrossRef]
- Jivraj, S.; Chee, W. Treatment planning of implants in the aesthetic zone. Br. Dent. J. 2006, 201, 77–89. [Google Scholar] [CrossRef]
- Giglio, G.D.; Giglio, A.B. Achieving optimal implant esthetics using a team approach Part 1 a review of evidence-based criteria in implant treatment. J. Prosthet. Dent. 2023, 130, 661–662. [Google Scholar] [CrossRef]
- Schincaglia, G.P.; Nowzari, H. Surgical treatment planning for the single-unit implant in aesthetic areas. Periodontol. 2000 2001, 27, 162–182. [Google Scholar] [CrossRef]
- Zhang, W.; Skrypczak, A.; Weltman, R. Anterior maxilla alveolar ridge dimension and morphology measurement by cone beam computerized tomography (CBCT) for immediate implant treatment planning. BMC Oral Health 2015, 15, 65. [Google Scholar] [CrossRef]
- Monje, A.; Roccuzzo, A.; Buser, D.; Wang, H.L. Influence of buccal bone wall thickness on the peri-implant hard and soft tissue dimensional changes: A systematic review. Clin. Oral Implant. Res. 2023, 34 (Suppl. S26), 8–27. [Google Scholar] [CrossRef]
- Avila-Ortiz, G.; Chambrone, L.; Vignoletti, F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46 (Suppl. S21), 195–223. [Google Scholar] [CrossRef]
- Couso-Queiruga, E.; Mansouri, C.J.; Alade, A.A.; Allareddy, T.V.; Galindo-Moreno, P.; Avila-Ortiz, G. Alveolar ridge preservation reduces the need for ancillary bone augmentation in the context of implant therapy. J. Periodontol. 2022, 93, 847–856. [Google Scholar] [CrossRef]
- Zhang, Y.; Wen, G.; Dong, W. Clinical outcomes of narrow- and regular-diameter implants with bone augmentation in the anterior maxilla: A systematic review and meta-analysis. Clin. Oral Investig. 2024, 28, 196. [Google Scholar] [CrossRef] [PubMed]
- Cao, R.; Chen, B.; Xu, H.; Fan, Z. Clinical outcomes of titanium-zirconium alloy narrow-diameter implants for single-crown restorations: A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2023, 61, 403–410. [Google Scholar] [CrossRef]
- Ivanoff, C.J.; Sennerby, L.; Johansson, C.; Rangert, B.; Lekholm, U. Influence of implant diameters on the integration of screw implants. An experimental study in rabbits. Int. J. Oral Maxillofac. Surg. 1997, 26, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Shemtov-Yona, K.; Rittel, D.; Machtei, E.E.; Levin, L. Effect of dental implant diameter on fatigue performance. Part II: Failure analysis. Clin. Implant Dent. Relat. Res. 2014, 16, 178–184. [Google Scholar] [CrossRef]
- Telles, L.H.; Portella, F.F.; Rivaldo, E.G. Longevity and marginal bone loss of narrow-diameter implants supporting single crowns: A systematic review. PLoS ONE 2019, 14, e0225046. [Google Scholar] [CrossRef]
- Parize, H.N.; Bohner, L.O.L.; Gama, L.T.; Porporatti, A.L.; Mezzomo, L.A.M.; Martin, W.C.; Goncalves, T. Narrow-diameter implants in the anterior region: A meta-analysis. Int. J. Oral Maxillofac. Implant. 2019, 34, 1347–1358. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Tapia, R.; Luzuriaga, F.; Orive, G. Influence of implant length, diameter, and geometry on stress distribution: A finite element analysis. Int. J. Periodontics Restor. Dent. 2010, 30, 89–95. [Google Scholar]
- Pierrisnard, L.; Renouard, F.; Renault, P.; Barquins, M. Influence of implant length and bicortical anchorage on implant stress distribution. Clin. Implant Dent. Relat. Res. 2003, 5, 254–262. [Google Scholar] [CrossRef]
- Roccuzzo, A.; Imber, J.C.; Lempert, J.; Hosseini, M.; Jensen, S.S. Narrow diameter implants to replace congenital missing maxillary lateral incisors: A 1-year prospective, controlled, clinical study. Clin. Oral Implant. Res. 2022, 33, 844–857. [Google Scholar] [CrossRef]
- Trbakovic, A.; Bongenhielm, U.; Thor, A. A clinical and radiological long-term follow-up study of narrow diameter implants in the aesthetic area. Clin. Implant Dent. Relat. Res. 2018, 20, 598–605. [Google Scholar] [CrossRef]
- Pieri, F.; Siroli, L.; Forlivesi, C.; Corinaldesi, G. Clinical, esthetic, and radiographic evaluation of small-diameter (3.0-mm) implants supporting single crowns in the anterior region: A 3-year prospective study. Int. J. Periodontics Restor. Dent. 2014, 34, 825–832. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Nardi, D.; Piattelli, A. Immediate versus one-stage restoration of small-diameter implants for a single missing maxillary lateral incisor: A 3-year randomized clinical trial. J. Periodontol. 2009, 80, 1393–1398. [Google Scholar] [CrossRef]
- MacLean, S.; Hermans, M.; Villata, L.; Polizzi, G.; Sisodia, N.; Cherry, J.E. A retrospective multicenter case series evaluating a novel 3.0-mm expanding tapered body implant for the rehabilitation of missing incisors. Quintessence Int. 2016, 47, 297–306. [Google Scholar] [CrossRef]
- Polizzi, G.; Fabbro, S.; Furri, M.; Herrmann, I.; Squarzoni, S. Clinical application of narrow Branemark System implants for single-tooth restorations. Int. J. Oral Maxillofac. Implant. 1999, 14, 496–503. [Google Scholar]
- Oyama, K.; Kan, J.Y.; Rungcharassaeng, K.; Lozada, J. Immediate provisionalization of 3.0-mm-diameter implants replacing single missing maxillary and mandibular incisors: 1-year prospective study. Int. J. Oral Maxillofac. Implant. 2012, 27, 173–180. [Google Scholar]
- King, P.; Maiorana, C.; Luthardt, R.G.; Sondell, K.; Oland, J.; Galindo-Moreno, P.; Nilsson, P. Clinical and Radiographic Evaluation of a Small-Diameter Dental Implant Used for the Restoration of Patients with Permanent Tooth Agenesis (Hypodontia) in the Maxillary Lateral Incisor and Mandibular Incisor Regions: A 36-Month Follow-Up. Int. J. Prosthodont. 2016, 29, 147–153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Galindo-Moreno, P.; Nilsson, P.; King, P.; Becktor, J.; Speroni, S.; Schramm, A.; Maiorana, C. Clinical and radiographic evaluation of early loaded narrow diameter implants—1-year follow-up. Clin. Oral Implant. Res. 2012, 23, 609–616. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Padial-Molina, M.; Nilsson, P.; King, P.; Worsaae, N.; Schramm, A.; Maiorana, C. The influence of the distance between narrow implants and the adjacent teeth on marginal bone levels. Clin. Oral Implant. Res. 2017, 28, 704–712. [Google Scholar] [CrossRef]
- Kolinski, M.; Hess, P.; Leziy, S.; Friberg, B.; Bellucci, G.; Trisciuoglio, D.; Wagner, W.; Moergel, M.; Pozzi, A.; Wiltfang, J.; et al. Immediate provisionalization in the esthetic zone: 1-year interim results from a prospective single-cohort multicenter study evaluating 3.0-mm-diameter tapered implants. Clin. Oral Investig. 2018, 22, 2299–2308. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Anitua, E. Plasma rich in growth factors: Preliminary results of use in the preparation of future sites for implants. Int. J. Oral Maxillofac. Implant. 1999, 14, 529–535. [Google Scholar]
- Anitua, E.; Alkhraisat, M.H.; Pinas, L.; Orive, G. Efficacy of biologically guided implant site preparation to obtain adequate primary implant stability. Ann. Anat. 2015, 199, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Carda, C.; Andia, I. A novel drilling procedure and subsequent bone autograft preparation: A technical note. Int. J. Oral Maxillofac. Implant. 2007, 22, 138–145. [Google Scholar]
- Furhauser, R.; Florescu, D.; Benesch, T.; Haas, R.; Mailath, G.; Watzek, G. Evaluation of soft tissue around single-tooth implant crowns: The pink esthetic score. Clin. Oral Implant. Res. 2005, 16, 639–644. [Google Scholar] [CrossRef]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- Chen, S.T.; Buser, D.; Sculean, A.; Belser, U.C. Complications and treatment errors in implant positioning in the aesthetic zone: Diagnosis and possible solutions. Periodontol. 2000 2023, 92, 220–234. [Google Scholar] [CrossRef]
- Anitua, E.; Alkhraisat, M.H. Is Alveolar Ridge Split a Risk Factor for Implant Survival? J. Oral Maxillofac. Surg. 2016, 74, 2182–2191. [Google Scholar] [CrossRef]
- Anitua, E.; Fernandez-de-Retana, S.; Anitua, B.; Alkhraisat, M.H. Long-Term Retrospective Study of 3.0-mm-Diameter Implants Supporting Fixed Multiple Prostheses: Immediate Versus Delayed Implant Loading. Int. J. Oral Maxillofac. Implant. 2020, 35, 1229–1238. [Google Scholar] [CrossRef]
- Anitua, E.; Saracho, J.; Begona, L.; Alkhraisat, M.H. Long-Term Follow-Up of 2.5-mm Narrow-Diameter Implants Supporting a Fixed Prostheses. Clin. Implant Dent. Relat. Res. 2016, 18, 769–777. [Google Scholar] [CrossRef]
- Antiua, E.; Escuer, V.; Alkhraisat, M.H. Short Narrow Dental Implants versus Long Narrow Dental Implants in Fixed Prostheses: A Prospective Clinical Study. Dent. J. 2022, 10, 39. [Google Scholar] [CrossRef]
- Freitas-Junior, A.C.; Bonfante, E.A.; Martins, L.M.; Silva, N.R.; Marotta, L.; Coelho, P.G. Effect of implant diameter on reliability and failure modes of molar crowns. Int. J. Prosthodont. 2011, 24, 557–561. [Google Scholar] [PubMed]
- Javed, F.; Romanos, G.E. Role of implant diameter on long-term survival of dental implants placed in posterior maxilla: A systematic review. Clin. Oral Investig. 2015, 19, 1–10. [Google Scholar] [CrossRef]
- Esposito, M.; Barausse, C.; Pistilli, R.; Bellini, P.; Buti, J.; Felice, P. Immediate loading of 3 mm-diameter implants as an alternative to horizontal bone augmentation for placing 4 mm-diameter implants: One-year post-loading results from a multicentre randomised controlled trial. Clin. Trials Dent. 2020, 2, 61–76. [Google Scholar]
- Assaf, A.; Saad, M.; Daas, M.; Abdallah, J.; Abdallah, R. Use of narrow-diameter implants in the posterior jaw: A systematic review. Implant Dent. 2015, 24, 294–306. [Google Scholar] [CrossRef]
- Manfredini, M.; Poli, P.P.; Giboli, L.; Beretta, M.; Maiorana, C.; Pellegrini, M. Clinical Factors on Dental Implant Fractures: A Systematic Review. Dent. J. 2024, 12, 200. [Google Scholar] [CrossRef]
- Lee, D.-W.; Kim, N.-H.; Lee, Y.; Oh, Y.-A.; Lee, J.-H.; You, H.-K. Implant fracture failure rate and potential associated risk indicators: An up to 12-year retrospective study of implants in 5,124 patients. Clin. Oral Implant. Res. 2019, 30, 206–217. [Google Scholar] [CrossRef]
- Lee, J.-H.; Kim, Y.-T.; Jeong, S.-N.; Kim, N.-H.; Lee, D.-W. Incidence and pattern of implant fractures: A long-term follow-up multicenter study. Clin. Implant Dent. Relat. Res. 2018, 20, 463–469. [Google Scholar] [CrossRef]
- Zhang, X.M.; Liu, B.L.; Qian, S.J.; Shi, J.Y.; Zhang, X.; Lai, H.C. Clinical evaluation of narrow-diameter implants versus standard-diameter implants with lateral bone augmentation in posterior jaws: Three-year results of a randomized controlled trial. Clin. Oral Implant. Res. 2022, 33, 1245–1253. [Google Scholar] [CrossRef]
- Zadrożny, Ł.; Górski, B.; Baldoni, E.; Lumbau, A.I.; Meloni, S.M.; Pisano, M.; Tallarico, M. Minimally Invasive Treatment of Lateral Incisors with Guided One-Piece or Two-Piece Titanium-Made Narrow Diameter Implants: A Retrospective Comparative Study with Up to Two Years Follow-Up. J. Clin. Med. 2023, 12, 3711. [Google Scholar] [CrossRef]
- Anitua, E. Implant Dentistry from One-Way Direction to the Reversibility of the Osseointegration. Eur. J. Dent. 2022, 16, 464. [Google Scholar] [CrossRef]
- Anitua, E.; Flores, C.; Pinas, L.; Alkhraisat, M.H. Frequency of Technical Complications in Fixed Implant Prosthesis: The Effect of Prosthesis Screw Emergence Correction by Computer-Aided Design/Computer-Aided Manufacturing. J. Oral Implantol. 2018, 44, 427–431. [Google Scholar] [CrossRef] [PubMed]
- Andersen, E.; Saxegaard, E.; Knutsen, B.M.; Haanaes, H.R. A prospective clinical study evaluating the safety and effectiveness of narrow-diameter threaded implants in the anterior region of the maxilla. Int. J. Oral Maxillofac. Implant. 2001, 16, 217–224. [Google Scholar]
- Ioannidis, A.; Gallucci, G.O.; Jung, R.E.; Borzangy, S.; Hammerle, C.H.; Benic, G.I. Titanium-zirconium narrow-diameter versus titanium regular-diameter implants for anterior and premolar single crowns: 3-year results of a randomized controlled clinical study. J. Clin. Periodontol. 2015, 42, 1060–1070. [Google Scholar] [CrossRef]
- de Souza, A.B.; Sukekava, F.; Tolentino, L.; Cesar-Neto, J.B.; Garcez-Filho, J.; Araujo, M.G. Narrow- and regular-diameter implants in the posterior region of the jaws to support single crowns: A 3-year split-mouth randomized clinical trial. Clin. Oral Implant. Res. 2018, 29, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Benic, G.I.; Gallucci, G.O.; Mokti, M.; Hammerle, C.H.; Weber, H.P.; Jung, R.E. Titanium-zirconium narrow-diameter versus titanium regular-diameter implants for anterior and premolar single crowns: 1-year results of a randomized controlled clinical study. J. Clin. Periodontol. 2013, 40, 1052–1061. [Google Scholar] [CrossRef]
- Zarone, F.; Sorrentino, R.; Vaccaro, F.; Russo, S. Prosthetic treatment of maxillary lateral incisor agenesis with osseointegrated implants: A 24-39-month prospective clinical study. Clin. Oral Implant. Res. 2006, 17, 94–101. [Google Scholar] [CrossRef]
- Spinato, S.; Galindo-Moreno, P.; Bernardello, F.; Zaffe, D. Minimum Abutment Height to Eliminate Bone Loss: Influence of Implant Neck Design and Platform Switching. Int. J. Oral Maxillofac. Implant. 2018, 33, 405–411. [Google Scholar] [CrossRef]
- Tajti, P.; Solyom, E.; Vancsa, S.; Matrai, P.; Hegyi, P.; Varga, G.; Hermann, P.; Borbely, J.; Sculean, A.; Mikulas, K. Less marginal bone loss around bone-level implants restored with long abutments: A systematic review and meta-analysis. Periodontol. 2000 2024, 94, 627–638. [Google Scholar] [CrossRef]
- Abrahamsson, I.; Berglundh, T.; Lindhe, J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J. Clin. Periodontol. 1997, 24, 568–572. [Google Scholar] [CrossRef]
- Koutouzis, T.; Gholami, F.; Reynolds, J.; Lundgren, T.; Kotsakis, G.A. Abutment Disconnection/Reconnection Affects Peri-implant Marginal Bone Levels: A Meta-Analysis. Int. J. Oral Maxillofac. Implant. 2017, 32, 575–581. [Google Scholar] [CrossRef]
- Romanos, G.E.; Traini, T.; Johansson, C.B.; Piattelli, A. Biologic width and morphologic characteristics of soft tissues around immediately loaded implants: Studies performed on human autopsy specimens. J. Periodontol. 2010, 81, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Kuppusamy, M.; Watanabe, H.; Kasugai, S.; Kuroda, S. Effects of Abutment Removal and Reconnection on Inflammatory Cytokine Production Around Dental Implants. Implant Dent. 2015, 24, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Coelho, A.L.; Suzuki, M.; Dibart, S.; DA Silva, N.; Coelho, P.G. Cross-sectional analysis of the implant-abutment interface. J. Oral Rehabil. 2007, 34, 508–516. [Google Scholar] [CrossRef] [PubMed]
- Duarte, A.R.; Rossetti, P.H.; Rossetti, L.M.; Torres, S.A.; Bonachela, W.C. In vitro sealing ability of two materials at five different implant-abutment surfaces. J. Periodontol. 2006, 77, 1828–1832. [Google Scholar] [CrossRef]
- Dibart, S.; Warbington, M.; Su, M.F.; Skobe, Z. In vitro evaluation of the implant-abutment bacterial seal: The locking taper system. Int. J. Oral Maxillofac. Implant. 2005, 20, 732–737. [Google Scholar]
- Jansen, V.K.; Conrads, G.; Richter, E.J. Microbial leakage and marginal fit of the implant-abutment interface. Int. J. Oral Maxillofac. Implant. 1997, 12, 527–540. [Google Scholar]
- Welander, M.; Abrahamsson, I.; Berglundh, T. Subcrestal placement of two-part implants. Clin. Oral Implant. Res. 2009, 20, 226–231. [Google Scholar] [CrossRef]
- Maeda, Y.; Satoh, T.; Sogo, M. In vitro differences of stress concentrations for internal and external hex implant-abutment connections: A short communication. J. Oral Rehabil. 2006, 33, 75–78. [Google Scholar] [CrossRef]
- Gomez-Meda, R.; Esquivel, J.; Blatz, M.B. The esthetic biological contour concept for implant restoration emergence profile design. J. Esthet. Restor. Dent. 2021, 33, 173–184. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Steigmann, M.; Vindasiute, E.; Linkeviciene, L. Influence of Vertical Soft Tissue Thickness on Crestal Bone Changes Around Implants with Platform Switching: A Comparative Clinical Study. Clin. Implant Dent. Relat. Res. 2015, 17, 1228–1236. [Google Scholar] [CrossRef]
- van Brakel, R.; Noordmans, H.J.; Frenken, J.; de Roode, R.; de Wit, G.C.; Cune, M.S. The effect of zirconia and titanium implant abutments on light reflection of the supporting soft tissues. Clin. Oral Implant. Res. 2011, 22, 1172–1178. [Google Scholar] [CrossRef]
- Dash, S.; Srivastava, G.; Padhiary, S.K.; Samal, M.; Cakmak, G.; Roccuzzo, A.; Molinero-Mourelle, P. Validation of the pink esthetic score/white esthetic score at single tooth-supported prostheses in the esthetic zone: A randomized clinical trial. J. Esthet. Restor. Dent. 2024, 36, 976–984. [Google Scholar] [CrossRef]
- Gehrke, P.; Lobert, M.; Dhom, G. Reproducibility of the pink esthetic score—Rating soft tissue esthetics around single-implant restorations with regard to dental observer specialization. J. Esthet. Restor. Dent. 2008, 20, 375–384, discussion 385. [Google Scholar] [CrossRef] [PubMed]
- Altay, M.A.; Sindel, A.; Tezerisener, H.A.; Yildirimyan, N.; Ozarslan, M.M. Esthetic evaluation of implant-supported single crowns: A comparison of objective and patient-reported outcomes. Int. J. Implant Dent. 2019, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Maia, N.G.; Normando, D.; Maia, F.A.; Ferreira, M.A.; do Socorro Costa Feitosa Alves, M. Factors associated with long-term patient satisfaction. Angle Orthod. 2010, 80, 1155–1158. [Google Scholar] [CrossRef]
- Kolerman, R.; Mijiritsky, E.; Barnea, E.; Dabaja, A.; Nissan, J.; Tal, H. Esthetic Assessment of Implants Placed into Fresh Extraction Sockets for Single-Tooth Replacements Using a Flapless Approach. Clin. Implant Dent. Relat. Res. 2017, 19, 351–364. [Google Scholar] [CrossRef] [PubMed]
- Palmer, R.M. Risk management in clinical practice. Part 9. Dental implants. Br. Dent. J. 2010, 209, 499–506. [Google Scholar] [CrossRef]
- Patil, P.G. A technique for repairing a loosening abutment screw for a cement-retained implant prosthesis. J. Prosthodont. 2011, 20, 652–655. [Google Scholar] [CrossRef]
| Length (mm) | Total | ||||||
|---|---|---|---|---|---|---|---|
| 6.5 | 7.5 | 8.5 | 10.0 | 11.0 | |||
| Diameter (mm) | 3.3 | 5 | 10 | 10 | 2 | 0 | 27 |
| 3.5 | 5 | 14 | 14 | 3 | 1 | 37 | |
| Total | 10 | 24 | 24 | 5 | 1 | 64 | |
| Variable | Value | |
|---|---|---|
| Width of the alveolar bone at crest (mean ± SD) | 5.6 ± 1.5 | |
| Bone type (number) | Type I | 6 |
| Type II | 51 | |
| Type III | 7 | |
| Bone density (A.U) (mean ± SD) | 741 ± 152 | |
| Insertion torque (N.cm) (mean ± SD) | 28 ± 15 | |
| Overcorrection of the vestibular plate | Yes | 49 |
| No | 15 | |
| Intermediate abutment lengths | 1.5 mm | 3 |
| 2 mm | 27 | |
| 2.5 mm | 21 | |
| 3.0 mm | 11 | |
| 3.5 mm | 2 | |
| Variable | Value | |
|---|---|---|
| Follow-up time (months) | 42 ± 19 | |
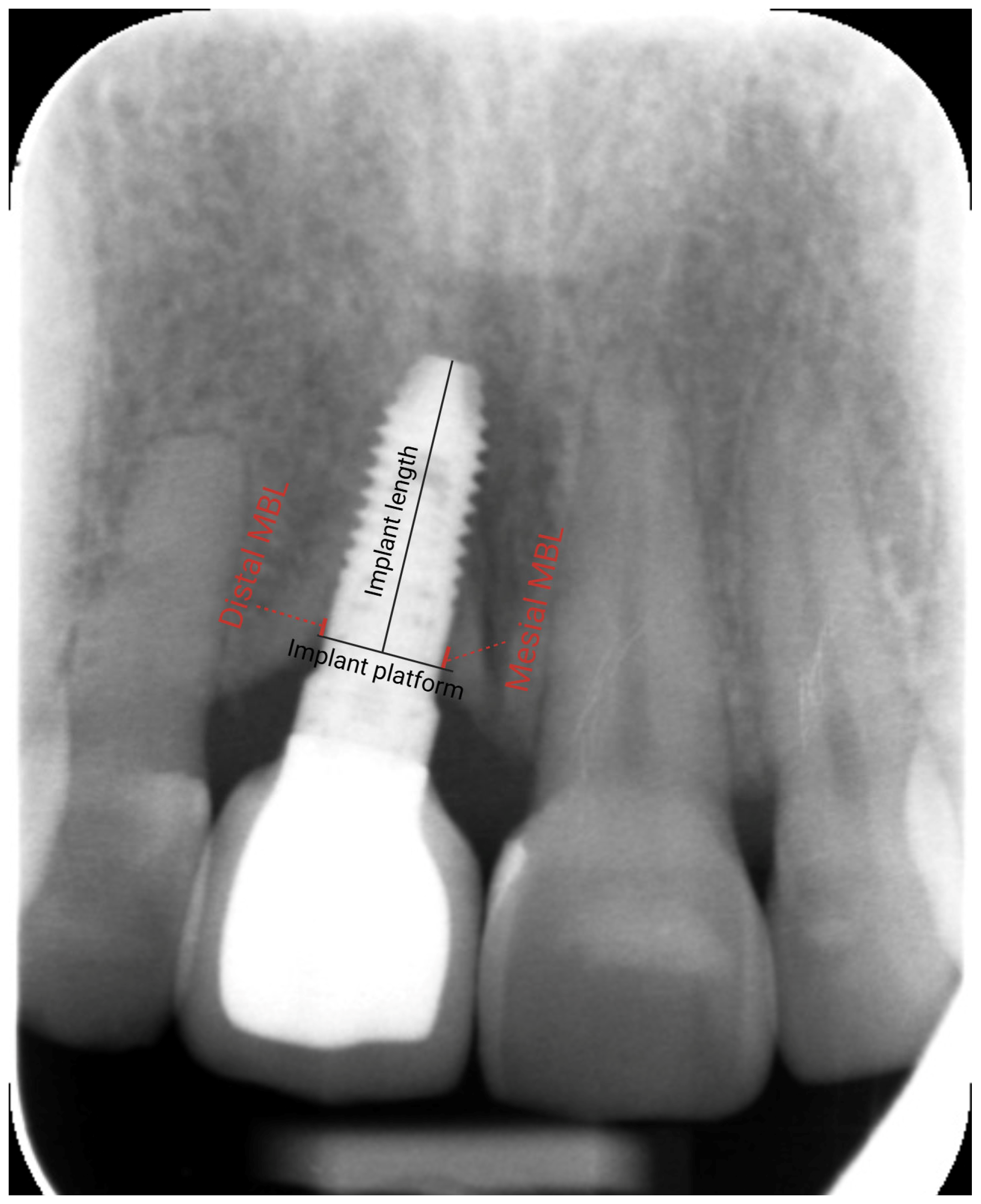
| Mesial MBL (mm) (mean ± SD) | Loading | 0.7 ± 1.0 |
| Distal MBL (mm) (mean ± SD) | 0.4 ± 0.9 | |
| Mesial MBL (mm) (mean ± SD) | Last radiograph | 0.0 ± 0.9 |
| Distal MBL (mm) (mean ± SD) | −0.1 ± 0.6 | |
| Variation in MBL–mesial (mm) (mean ± SD) | −0.7 ± 0.9 | |
| Variation in MBL–distal (mm) (mean ± SD) | −0.5 ± 0.7 | |
| Implant failure (frequency) | 0 | |
| Pink Esthetic Score | 7.0 ± 2.6 | |
| White Esthetic Score | 7.9 ± 2.0 |
| Variable | Value |
|---|---|
| Change the intermediate abutment | 4 |
| Pressure on peri-implant mucosa | 1 |
| Screw loosening | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anitua, E.; Tarazona, A.; Alkhraisat, M.H. Retrospective Study of Functional and Esthetic Outcomes Using Narrow-Diameter Implants for Single Upper Central Incisor Replacements. Dent. J. 2025, 13, 144. https://doi.org/10.3390/dj13040144
Anitua E, Tarazona A, Alkhraisat MH. Retrospective Study of Functional and Esthetic Outcomes Using Narrow-Diameter Implants for Single Upper Central Incisor Replacements. Dentistry Journal. 2025; 13(4):144. https://doi.org/10.3390/dj13040144
Chicago/Turabian StyleAnitua, Eduardo, Aitana Tarazona, and Mohammad Hamdan Alkhraisat. 2025. "Retrospective Study of Functional and Esthetic Outcomes Using Narrow-Diameter Implants for Single Upper Central Incisor Replacements" Dentistry Journal 13, no. 4: 144. https://doi.org/10.3390/dj13040144
APA StyleAnitua, E., Tarazona, A., & Alkhraisat, M. H. (2025). Retrospective Study of Functional and Esthetic Outcomes Using Narrow-Diameter Implants for Single Upper Central Incisor Replacements. Dentistry Journal, 13(4), 144. https://doi.org/10.3390/dj13040144







