An In-Vitro Investigation into the Fracture Resistance of Prefabricated and Custom-Made Zirconia Crowns for Permanent Molars in Children
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
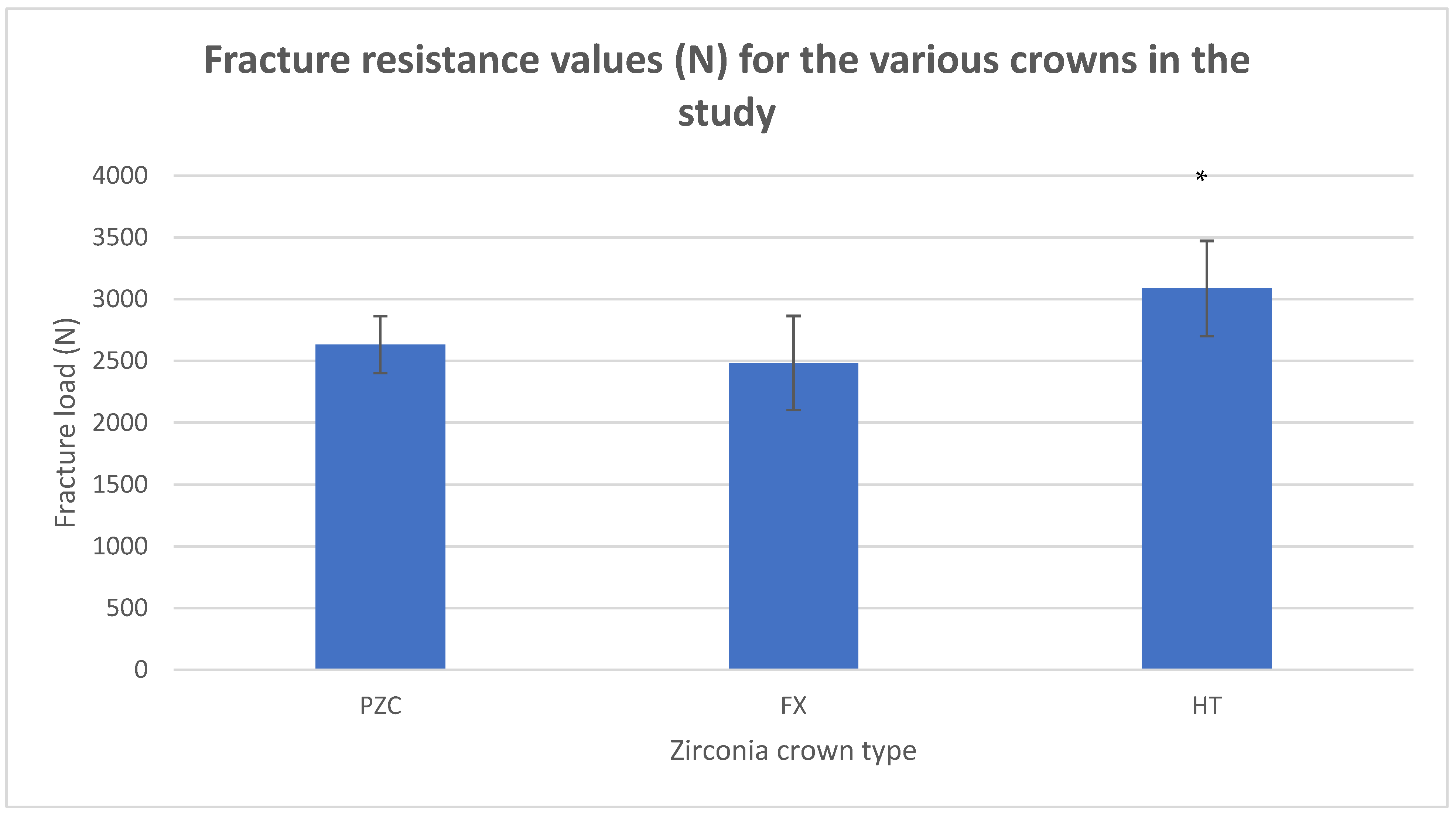
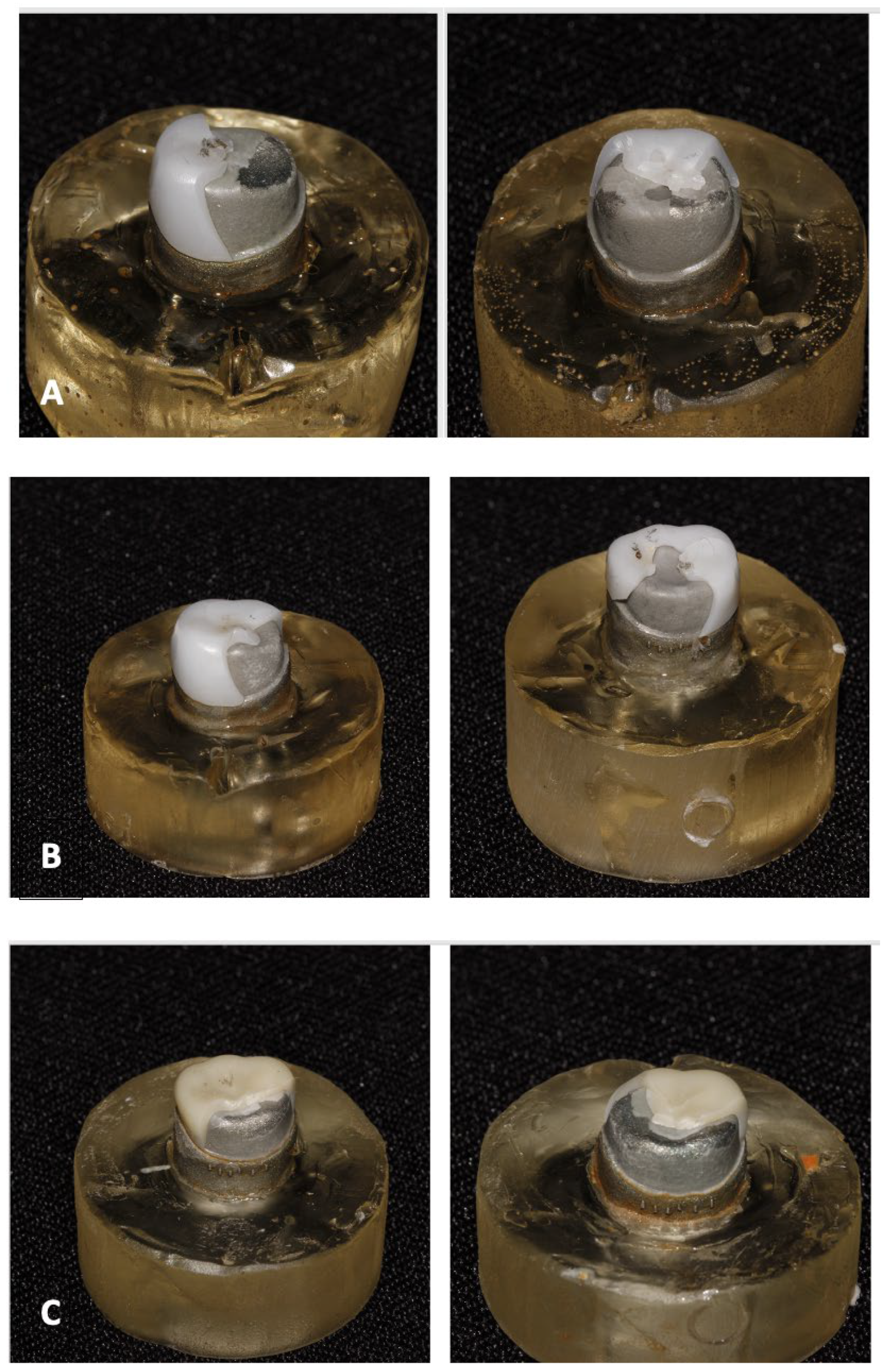
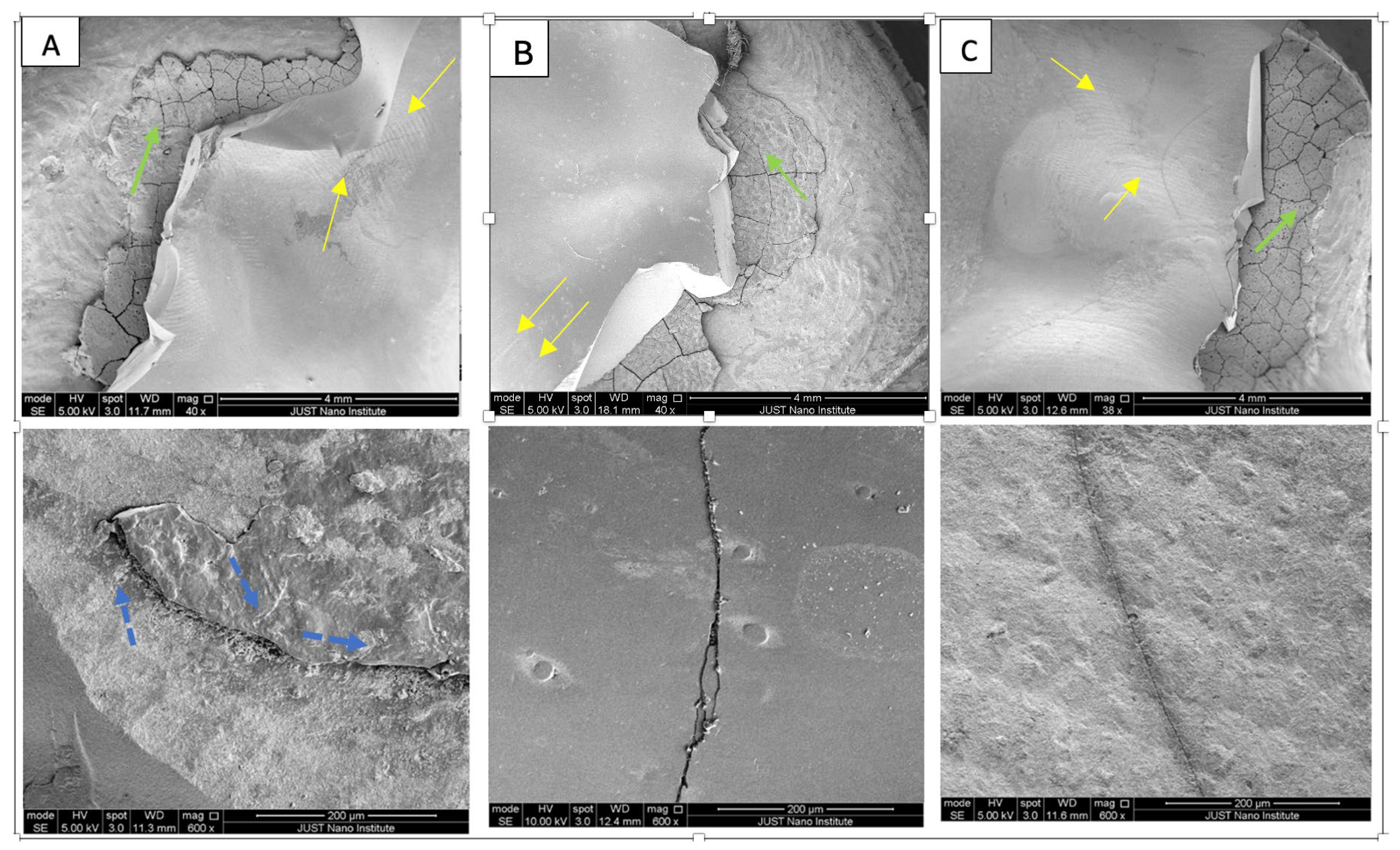
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Innes, N.P.; Ricketts, D.; Chong, L.Y.; Keightley, A.J.; Lamont, T.; Santamaria, R.M. Preformed crowns for decayed primary molar teeth. Cochrane Database Syst. Rev. 2015, 31, CD005512. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Cazaux, S.; Aiem, E.; Velly, A.M.; Muller-Bolla, M. Preformed pediatric zirconia crown versus preformed pediatric metal crown: Study protocol for a randomized clinical trial. Trials 2019, 20, 530. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, J.A.; Feigal, R.J.; Till, M.J.; Hodges, J.S. Parental attitudes on restorative materials as factors influencing current use in pediatric dentistry. Pediatr. Dent. 2009, 31, 63–70. [Google Scholar] [PubMed]
- Taylor, G.D. Aesthetic preformed crowns for primary teeth. Evid. Based Dent. 2017, 18, 43–44. [Google Scholar] [CrossRef]
- El Makawi, Y.; Khattab, N. In Vitro Comparative Analysis of Fracture Resistance of Lithium Disilicate Endocrown and Prefabricated Zirconium Crown in Pulpotomized Primary Molars. Open Access Maced. J. Med. Sci. 2019, 7, 4094–4100. [Google Scholar] [CrossRef]
- Holsinger, D.M.; Wells, M.H.; Scarbecz, M.; Donaldson, M. Clinical Evaluation and Parental Satisfaction with Pediatric Zirconia Anterior Crowns. Pediatr. Dent. 2016, 38, 192–197. [Google Scholar]
- Elian El Hayek, J.; El Osta, N.; Farhat Mchayleh, N. Fracture strength of preformed zirconia crown and new custom-made zirconia crown for the restoration of deciduous molars: In vitro study. Eur. Arch. Paediatr. Dent. 2022, 23, 333–339. [Google Scholar] [CrossRef]
- Alzanbaqi, S.D.; Alogaiel, R.M.; Alasmari, M.A.; Al Essa, A.M.; Khogeer, L.N.; Alanazi, B.S.; Hawsah, E.S.; Shaikh, A.M.; Ibrahim, M.S. Zirconia Crowns for Primary Teeth: A Systematic Review and Meta-Analyses. Int. J. Environ. Res. Public Health 2022, 19, 2838. [Google Scholar] [CrossRef]
- Kelly, N.; Lamont, T. Are zirconia crowns the superior choice when restoring primary posterior molars? Evid. Based Dent. 2022, 23, 72–73. [Google Scholar] [CrossRef]
- Albakry, M. Insightful Understanding of the Role of the Mechanical Properties in Defining the Reliability of All-Ceramic Dental Restorations: A Review. J. Biomater. Nanobiotechnol. 2021, 12, 57–78. [Google Scholar] [CrossRef]
- Cumerlato, C.B.D.F.; Demarco, F.F.; Barros, A.J.D.; Peres, M.A.; Peres, K.G.; Morales Cascaes, A.; de Camargo, M.B.J.; da Silva Dos Santos, I.; Matijasevich, A.; Corrêa, M.B. Reasons for direct restoration failure from childhood to adolescence: A birth cohort study. J. Dent. 2019, 89, 103183. [Google Scholar] [CrossRef] [PubMed]
- Schlenz, M.A.; Schmidt, A.; Rehmann, P.; Wöstmann, B. Fatigue damage of monolithic posterior computer aided designed/computer aided manufactured crowns. J. Prosthodon Res. 2019, 63, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Al-Halabi, M.N.; Bshara, N.; Comisi, J.C.; Abou Nassar, J. Evaluation of Fracture Resistance Force in Three Types of Primary Molar Crowns: Milled by CAD\CAM, 3D Dental Printed, and Composite Celluloid Crowns. Eur. Dent. Res. Biomater. J. 2020, 1, 33–39. [Google Scholar] [CrossRef]
- Papadiochou, S.; Pissiotis, A.L. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef]
- Hanafi, L.; Altinawi, M.; Comisi, J.C. Evaluation and comparison two types of prefabricated zirconia crowns in mixed and primary dentition: A randomized clinical trial. Heliyon 2021, 7, e06240. [Google Scholar] [CrossRef]
- Townsend, J.A.; Knoell, P.; Yu, Q.; Zhang, J.F.; Wang, Y.; Zhu, H.; Beattie, S.; Xu, X. In vitro fracture resistance of three commercially available zirconia crowns for primary molars. Pediatr. Dent. 2014, 36, 125–129. [Google Scholar]
- Al Shobber, M.Z.; Alkhadra, T.A. Fracture resistance of different primary anterior esthetic crowns. Saudi Dent. J. 2017, 29, 179–184. [Google Scholar] [CrossRef]
- Abushanan, A.; Sharanesha, R.B.; Aljuaid, B.; Alfaifi, T.; Aldurayhim, A. Fracture Resistance of Primary Zirconia Crowns: An In Vitro Study. Children 2022, 9, 77. [Google Scholar] [CrossRef]
- Kist, S.; Stawarczyk, B.; Kollmuss, M.; Hickel, R.; Huth, K.C. Fracture load and chewing simulation of zirconia and stainless-steel crowns for primary molars. Eur. J. Oral Sci. 2019, 127, 369–375. [Google Scholar] [CrossRef]
- Morresi, A.L.; D’Amario, M.; Capogreco, M.; Gatto, R.; Marzo, G.; D’Arcangelo, C.; Monaco, A. Thermal cycling for restorative materials: Does a standardized protocol exist in laboratory testing? A literature review. J. Mech. Behav. Biomed. Mater. 2014, 29, 295–308. [Google Scholar] [CrossRef]
- Kongkiatkamon, S.; Rokaya, D.; Kengtanyakich, S.; Peampring, C. Current classification of zirconia in dentistry: An updated review. PeerJ 2023, 11, e15669. [Google Scholar] [CrossRef] [PubMed]
- Kongkiatkamon, S.; Booranasophone, K.; Tongtaksin, A.; Kiatthanakorn, V.; Rokaya, D. Comparison of Fracture Load of the Four Translucent Zirconia Crowns. Molecules 2021, 26, 5308. [Google Scholar] [CrossRef] [PubMed]
- El Shahawy, O.I.; Azab, M.M. Fracture resistance of prefabricated versus custom-made zirconia crowns after thermo-mechanical aging: An in-vitro study. BMC Oral Health 2022, 22, 587. [Google Scholar] [CrossRef] [PubMed]
- Hassouneh, L.; Jum’ah, A.A.; Ferrari, M.; Wood, D.J. Post-fatigue fracture resistance of premolar teeth restored with endocrowns: An in vitro investigation. J. Dent. 2020, 100, 103426. [Google Scholar] [CrossRef]
- Preis, V.; Behr, M.; Hahnel, S.; Rosentritt, M. Influence of cementation on in vitro performance, marginal adaptation and fracture resistance of CAD/CAM-fabricated ZLS molar crowns. Dent. Mater. 2015, 31, 1363–1369. [Google Scholar] [CrossRef]
- Mathew, M.G.; Roopa, K.B.; Soni, A.J.; Khan, M.M.; Kauser, A. Evaluation of Clinical Success, Parental and Child Satisfaction of Stainless Steel Crowns and Zirconia Crowns in Primary Molars. J. Fam. Med. Prim. Care 2020, 9, 1418–1423. [Google Scholar] [CrossRef]
- Braun, S.; Hnat, W.P.; Freudenthaler, J.W.; Marcotte, M.R.; Hönigle, K.; Johnson, B.E. A study of maximum bite force during growth and development. Angle Orthod. 1996, 66, 261–264. [Google Scholar]
- Singh, R.; Singh, S.; Jha, A.; Jha, S.; Singh, A.K.; Kumar, S. Comparative evaluation of bite force in paediatric patients. J. Fam. Med. Prim. Care 2020, 9, 2002–2005. [Google Scholar]
- Sonnesen, L.; Bakke, M. Molar bite force in relation to occlusion, craniofacial dimensions, and head posture in pre-orthodontic children. Eur. J. Orthod. 2005, 27, 58–63. [Google Scholar] [CrossRef]
- Owais, A.I.; Al-Battah, A.H.; Alhaija, S.A. Changes in occlusal bite force following placement of preformed metal crowns on primary molars in 4–6 years old children: A 6 months’ follow-up pilot study. Eur. Arch. Paediatr. Dent. 2019, 20, 9–14. [Google Scholar] [CrossRef]
| Crown Brand | Chemical Composition | Manufacturer |
|---|---|---|
| Ceramill Zolid-FX white (FX) | ZrO2 + HfO2 + Y2O3 ≥ 99%, Y2O3 9.15–9.55%, HfO2 ≤ 5%, Al2O3 ≤ 0.5%, other oxides ≤ 1% | Amann Girrbach AG Koblach, Austria |
| Ceramill Zolid HT (HT) | ZrO2 + HfO2 + Y2O3 ≥ 99%, Y2O3 6.7–7.2%, HfO2 ≤ 5%, Al2O3 ≤ 0.5%, other oxides ≤ 1% | Amann Girrbach AG Koblach, Austria |
| NuSmile PZC | ZrO2 88–96% Y2O3 4–6% HfO2 5% | NuSmile, Houston, TX, USA |
| Group | Mean (N) | Standard Deviation | 95% Confidence Interval Lower Upper | ANOVA Test F Value and Significance | |
|---|---|---|---|---|---|
| PZC (n = 10) | 2633 | 230 | 2468 | 2797 | 8.6 (0.001) *** |
| FX (n = 10) | 2483 | 381 | 2211 | 2755 | |
| HT (n = 10) | 3087 | 385 | 2811 | 3362 | |
| Total (n = 30) | 2734 | 419 | 2578 | 2891 | |
| (I) GR | (J) GR | Mean Difference (I–J) | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| PZC | FX | 149.6 | 1.000 | −238.0158 | 537.2158 |
| HT | −453.8 * | 0.018 * | −841.4158 | −66.1842 | |
| FX | PZC | −149.6 | 1.000 | −537.2158 | 238.0158 |
| HT | −603.4 * | 0.001 * | −991.0158 | −215.7842 | |
| HT | PZC | 453.8 * | 0.018 * | 66.1842 | 841.4158 |
| FX | 603.4 * | 0.001 * | 215.7842 | 991.0158 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bani-Hani, T.; Al-Fodeh, R.S.; Al-Wahadni, A.M.; Abu-Alhaija, E.S.; Al-Hakam, M. An In-Vitro Investigation into the Fracture Resistance of Prefabricated and Custom-Made Zirconia Crowns for Permanent Molars in Children. Dent. J. 2025, 13, 64. https://doi.org/10.3390/dj13020064
Bani-Hani T, Al-Fodeh RS, Al-Wahadni AM, Abu-Alhaija ES, Al-Hakam M. An In-Vitro Investigation into the Fracture Resistance of Prefabricated and Custom-Made Zirconia Crowns for Permanent Molars in Children. Dentistry Journal. 2025; 13(2):64. https://doi.org/10.3390/dj13020064
Chicago/Turabian StyleBani-Hani, Thikrayat, Rami S. Al-Fodeh, Ahed M. Al-Wahadni, Elham S. Abu-Alhaija, and Mahmoud Al-Hakam. 2025. "An In-Vitro Investigation into the Fracture Resistance of Prefabricated and Custom-Made Zirconia Crowns for Permanent Molars in Children" Dentistry Journal 13, no. 2: 64. https://doi.org/10.3390/dj13020064
APA StyleBani-Hani, T., Al-Fodeh, R. S., Al-Wahadni, A. M., Abu-Alhaija, E. S., & Al-Hakam, M. (2025). An In-Vitro Investigation into the Fracture Resistance of Prefabricated and Custom-Made Zirconia Crowns for Permanent Molars in Children. Dentistry Journal, 13(2), 64. https://doi.org/10.3390/dj13020064






