Association of Connective Tissue Grafts in Immediate Implants: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
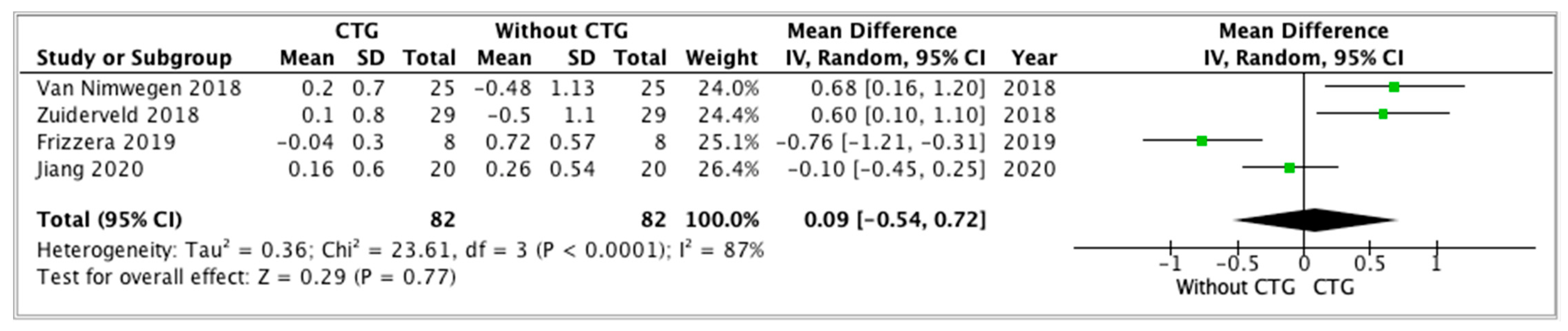
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ST | Soft Tissue. |
| IIP | Immediate Implant Placement. |
| CTG | Connective Tissue Graft. |
| RCT | Randomized Control Trial. |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses. |
| OCEBM | Oxford Classification of Evidence Levels. |
| CI | Confidence Interval. |
| CG | Control Group. |
| SG | Study Group. |
| PES | Pink Esthetic Score. |
| ICAI | Crown Aesthetic Index. |
| Nw | Newtons. |
References
- Olsson, M.; Lindhe, J. Periodontal characteristics in individuals with varying form of the upper central incisors. J. Clin. Periodontol. 1991, 18, 78–82. [Google Scholar] [CrossRef]
- Puzio, M.; Hadzik, J.; Błaszczyszyn, A.; Gedrange, T.; Dominiak, M. Soft tissue augmentation around dental implants with connective tissue graft (CTG) and xenogenic collagen matrix (XCM). 1-year randomized control trail. Ann. Anat. 2020, 230, 151484. [Google Scholar] [CrossRef] [PubMed]
- Thoma, D.S.; Cosyn, J.; Fickl, S.; Jensen, S.S.; Jung, R.E.; Raghoebar, G.M.; Rocchietta, I.; Roccuzzo, M.; Sanz, M.; Sanz-Sánchez, I.; et al. Soft tissue management at implants: Summary and consensus statements of group 2. The 6th EAO Consensus Conference 2021. Clin. Oral Implants Res. 2021, 32, 174–180. [Google Scholar] [CrossRef]
- Poli, P.P.; Maridati, P.C.; Stoffella, E.; Beretta, M.; Maiorana, C. Influence of Timing on the Horizontal Stability of Connective Tissue Grafts for Buccal Soft Tissue Augmentation at Single Implants: A Prospective Controlled Pilot Study. J. Oral Maxillofac. Surg. 2019, 77, 1170–1179. [Google Scholar] [CrossRef]
- Rojo, E.; Stroppa, G.; Sanz-Martin, I.; Gonzalez-Martín, O.; Nart, J. Soft tissue stability around dental implants after soft tissue grafting from the lateral palate or the tuberosity area—A randomized controlled clinical study. J. Clin. Periodontol. 2020, 47, 892–899. [Google Scholar] [CrossRef]
- Aldhohrah, T.; Qin, G.; Liang, D.; Song, W.; Ge, L.; Ahmed Mashrah, M.I.; Wang, L. Does simultaneous soft tissue augmentation around immediate or delayed dental implant placement using sub-epithelial connective tissue graft provide better outcomes compared to other treatment options? A systematic review and meta-analysis. PLoS ONE 2022, 17, E0261513. [Google Scholar] [CrossRef]
- Lin, C.Y.; Chen, Z.; Pan, W.L.; Wang, H.L. Impact of timing on soft tissue augmentation during implant treatment: A systematic review and meta-analysis. Clin. Oral Implants Res. 2018, 29, 508–521. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, P.; Manicone, P.F.; Rella, E.; Liguori, M.G.; De Angelis, S.; Tancredi, S.; D’Addona, A. The effect of soft tissue augmentation on the clinical and radiographical outcomes following immediate implant placement and provisionalization: A systematic review and meta-analysis. Int. J. Implant Dent. 2021, 7, 86. [Google Scholar] [CrossRef]
- Bianchi, S.; Bernardi, S.; Mattei, A.; Cristiano, L.; Mancini, L.; Torge, D.; Varvara, G.; Macchiarelli, G.; Marchetti, E. Morphological and Biological Evaluations of Human Periodontal Ligament Fibroblasts in Contact with Different Bovine Bone Grafts Treated with Low-Temperature Deproteinisation Protocol. Int. J. Mol. Sci. 2022, 9, 5273. [Google Scholar] [CrossRef]
- Ashurko, I.; Tarasenko, S.; Magdalyanova, M.; Bokareva, S.; Balyasin, M.; Galyas, A.; Khamidova, M.; Zhornik, M.; Unkovskiy, A. Comparative analysis of xenogeneic collagen matrix and autogenous subepithelial connective tissue graft to increase soft tissue volume around dental implants: A systematic review and meta-analysis. BMC Oral Health 2023, 23, 741. [Google Scholar] [CrossRef]
- D’Elia, C.; Baldini, N.; Cagidiaco, E.; Nofri, G.; Goracci, C.; de Sanctis, M. Peri-implant Soft Tissue Stability After Single Implant Restorations Using Either Guided Bone Regeneration or a Connective Tissue Graft: A Randomized Clinical Trial. Int. J. Periodontics Restor. Dent. 2017, 37, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Zuiderveld, E.G.; Meijer, H.J.A.; Vissink, A.; Raghoebar, G.M. The influence of different soft-tissue grafting procedures at single implant placement on esthetics: A randomized controlled trial. J. Periodontol. 2018, 89, 903–914. [Google Scholar] [CrossRef]
- Cairo, F.; Barbato, L.; Tonelli, P.; Batalocco, G.; Pagavino, G.; Nieri, M. Xenogeneic collagen matrix versus connective tissue graft for buccal soft tissue augmentation at implant site. A randomized, controlled clinical trial. J. Clin. Periodontol. 2017, 44, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Puisys, A.; Deikuviene, J.; Vindasiute-Narbute, E.; Razukevicus, D.; Zvirblis, T.; Linkevicius, T. Connective tissue graft vs porcine collagen matrix after immediate implant placement in esthetic area: A randomized clinical trial. Clin. Implant Dent. Relat. Res. 2022, 24, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Ferrantino, L.; Camurati, A.; Gambino, P.; Marzolo, M.; Trisciuoglio, D.; Santoro, G.; Farina, V.; Fontana, F.; Asa’ad, F.; Simion, M. Aesthetic outcomes of non-functional immediately restored single post-extraction implants with and without connective tissue graft: A multicentre randomized controlled trial. Clin. Oral Implants Res. 2021, 32, 684–694. [Google Scholar] [CrossRef] [PubMed]
- Wychowański, P.; Starzynska, A.; Osiak, M.; Kowalski, J.; Jereczek-Fossa, B.A.; Seklecka, B.; Morawiec, T.; Adamska, P.; Wolinski, J. The Anatomical Conditions of the Alveolar Process of the Anterior Maxilla in Terms of Immediate Implantation—Radiological Retrospective Case Series Study. J. Clin. Med. 2021, 10, 1688. [Google Scholar] [CrossRef] [PubMed]
- Van Nimwegen, W.G.; Raghoebar, G.M.; Zuiderveld, E.G.; Jung, R.E.; Meijer, H.J.A.; Mühlemann, S. Immediate placement and provisionalization of implants in the aesthetic zone with or without a connective tissue graft: A 1-year randomized controlled trial and volumetric study. Clin. Oral Implants Res. 2018, 29, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Zuiderveld, E.G.; van Nimwegen, W.G.; Meijer, H.J.; Jung, R.E.; Mühlemann, S.; Vissink, A.; Raghoebar, G.M. Effect of connective tissue grafting on buccal bone changes based on cone beam computed tomography scans in the esthetic zone of single immediate implants: A 1-year randomized controlled trial. J. Periodontol. 2021, 92, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Fujii, M.; Nakano, T.; Ishigaki, S. Pre- and Postoperative Evaluation of Immediate and Early Implant Placement in Esthetic Areas with Pre-Extraction Facial Dehiscence: A Retrospective Clinical Study. J. Clin. Med. 2023, 12, 6616. [Google Scholar] [CrossRef]
- Papapetros, D.; Vassilis, K.; Antonis, K.; Danae, A.A. Interim tissue changes following connective tissue grafting and two-stage implant placement. A randomized clinical trial. J. Clin. Periodontol. 2019, 46, 958–968. [Google Scholar] [CrossRef]
- Chokaree, P.; Poovarodom, P.; Chaijareenont, P.; Rungsiyakull, P. Effect of Customized and Prefabricated Healing Abutments on Peri-Implant Soft Tissue and Bone in Immediate Implant Sites: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 886. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Manterola, C.D.; Zavando, D.M.; Mincir, G. Cómo interpretar los «Niveles de Evidencia» en los diferentes escenarios clínicos* Evidence-based clinical practice, levels of evidence. Rev. Chil. Cir. 2009, 61, 582–595. [Google Scholar] [CrossRef]
- Esposito, M.; Maghaireh, H.; Grusovin, M.G.; Ziounas, I.; Worthington, H.V. Soft tissue management for dental implants: What are the most effective techniques? A Cochrane systematic review. Eur. J. Oral Implantol. 2012, 5, 221–238. [Google Scholar] [PubMed]
- Rojo, E.; Stroppa, G.; Sanz-Martin, I.; Gonzalez-Martín, O.; Alemany, A.S.; Nart, J. Soft tissue volume gain around dental implants using autogenous subepithelial connective tissue grafts harvested from the lateral palate or tuberosity area. A randomized controlled clinical study. J. Clin. Periodontol. 2018, 45, 495–503. [Google Scholar] [CrossRef]
- Hutton, C.G.; Johnson, G.K.; Barwacz, C.A.; Allareddy, V.; Avila-Ortiz, G. Comparison of two different surgical approaches to increase peri-implant mucosal thickness: A randomized controlled clinical trial. J. Periodontol. 2018, 89, 807–814. [Google Scholar] [CrossRef] [PubMed]
- Zuiderveld, E.G.; Meijer, H.J.A.; den Hartog, L.; Vissink, A.; Raghoebar, G.M. Effect of connective tissue grafting on peri-implant tissue in single immediate implant sites: A RCT. J. Clin. Periodontol. 2018, 45, 253–264. [Google Scholar] [CrossRef]
- De Bruyckere, T.; Cabeza, R.G.; Eghbali, A.; Younes, F.; Cleymaet, R.; Cosyn, J. A randomized controlled study comparing guided bone regeneration with connective tissue graft to reestablish buccal convexity at implant sites: A 1-year volumetric analysis. Clin. Implant Dent. Relat. Res. 2020, 22, 468–476. [Google Scholar] [CrossRef]
- De Bruyckere, T.; Cosyn, J.; Younes, F.; Hellyn, J.; Bekx, J.; Cleymaet, R.; Eghbali, A. A randomized controlled study comparing guided bone regeneration with connective tissue graft to re-establish buccal convexity: One-year aesthetic and patient-reported outcomes. Clin. Oral Implants Res. 2020, 31, 507–516. [Google Scholar] [CrossRef]
- De Bruyckere, T.; Eeckhout, C.; Eghbali, A.; Younes, F.; Vandekerckhove, P.; Cleymaet, R.; Cosyn, J. A randomized controlled study comparing guided bone regeneration with connective tissue graft to re-establish convexity at the buccal aspect of single implants: A one-year CBCT analysis. J. Clin. Periodontol. 2018, 45, 1375–1387. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.; Di, P.; Ren, S.; Zhang, Y.; Lin, Y. Hard and soft tissue alterations during the healing stage of immediate implant placement and provisionalization with or without connective tissue graft: A randomized clinical trial. J. Clin. Periodontol. 2020, 47, 1006–1015. [Google Scholar] [CrossRef] [PubMed]
- Frizzera, F.; de Freitas, R.; Muñoz-Chávez, O.; Cabral, G.; Shibli, J.; Marcantonio, E. Impact of Soft Tissue Grafts to Reduce Peri-implant Alterations After Immediate Implant Placement and Provisionalization in Compromised Sockets. Int. J. Periodontics Restor. Dent. 2019, 39, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Puisys, A.; Auzbikaviciute, V.; Vindasiute-Narbute, E.; Pranskunas, M.; Razukevicus, D.; Linkevicius, T. Immediate implant placement vs. early implant treatment in the esthetic area. A 1-year randomized clinical trial. Clin. Oral Implants Res. 2022, 33, 634–655. [Google Scholar] [CrossRef] [PubMed]
- Cosyn, J.; De Lat, L.; Lorenz Seyssens, L.; Doornewaard, R.; Deschepper, E.; Vervaeke, S. The effectiveness of immediate implant placement for single tooth replacement compared to delayed implant placement: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 224–241. [Google Scholar] [CrossRef] [PubMed]
- Esquivel, J.; Meda, R.; Blatz, M. The Impact of 3D Implant Position on Emergence Profile Design. Int. J. Periodontics Restor. Dent. 2021, 41, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Steigmann, M.; Monje, A.; Chan, H.L.; Wang, H.L. Emergence Profile Design Based on Implant Position in the Esthetic Zone. Int. J. Periodontics Restor. Dent. 2014, 34, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Martins da Rosa, J.C.; Pértile de Oliveira Rosa, A.C.; Francischone, C.E.; Salles Sotto-Maior, B. Esthetic Outcomes and Tissue Stability of Implant Placement in Compromised Sockets Following Immediate Dentoalveolar Restoration: Results of a Prospective Case Series at 58 Months Follow-up. Int. J. Periodontics Restor. Dent. 2014, 34, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Hassani, A.; Hassani, M.; Bitaraf, T. Immediate vs Delayed Restorations of Immediately Placed Single Implants in the Anterior Maxilla: A Nonrandomized Clinical Study. Int. J. Oral Maxillofac. Implants 2021, 36, 1159–1164. [Google Scholar] [CrossRef]
- Yoshino, S.; Kan, J.Y.K.; Rungcharassaeng, K.; Roe, P.; Lozada, J.L. Effects of Connective Tissue Grafting on the Facial Gingival Level Following Single Immediate Implant Placement and Provisionalization in the Esthetic Zone: A 1-Year Randomized Controlled Prospective Study. Int. J. Oral Maxillofac. Implants 2014, 29, 432–440. [Google Scholar] [CrossRef]
- Migliorati, M.; Amorfini, L.; Signori, A.; Biavati, A.S.; Benedicenti, S. Clinical and Aesthetic Outcome with Post-Extractive Implants with or without Soft Tissue Augmentation: A 2-Year Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2015, 17, 983–995. [Google Scholar] [CrossRef] [PubMed]
- Seyssens, L.; De Lat, L.; Cosyn, J. Immediate implant placement with or without connective tissue graft: A systematic review and meta-analysis. J. Clin. Periodontol. 2021, 48, 284–301. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Buser, D. Esthetic Outcomes Following Immediate and Early Implant Placement in the Anterior Maxilla—A Systematic Review. Int. J. Oral Maxillofac. Implants 2014, 29, 186–215. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.G.; da Silva, J.C.C.; de Mendonça, A.F.; Lindhe, J. Ridge alterations following grafting of fresh extraction sockets in man: A randomized clinical trial. Clin. Oral Implant. Res. 2015, 26, 407–412. [Google Scholar] [CrossRef]
- ElAskary, A.; Elfana, A.; Meabed, M.; Abd-ElWahab Radi, I.; Akram, M.; Fawzy El-Sayed, K. Immediate implant placement utilizing vestibular socket therapy versus early implant placement with contour augmentation for rehabilitation of compromised extraction sockets in the esthetic zone: A randomized controlled clinical trial. Clin. Implant Dent. Relat. Res. 2022, 24, 559–568. [Google Scholar] [CrossRef]
- Sanz-Martín, I.; Rojo, E.; Maldonado, E.; Stroppa, G.; Nart, J.; Sanz, M. Structural and histological differences between connective tissue grafts harvested from the lateral palatal mucosa or from the tuberosity area. Clin. Oral Investig. 2019, 23, 957–964. [Google Scholar] [CrossRef]

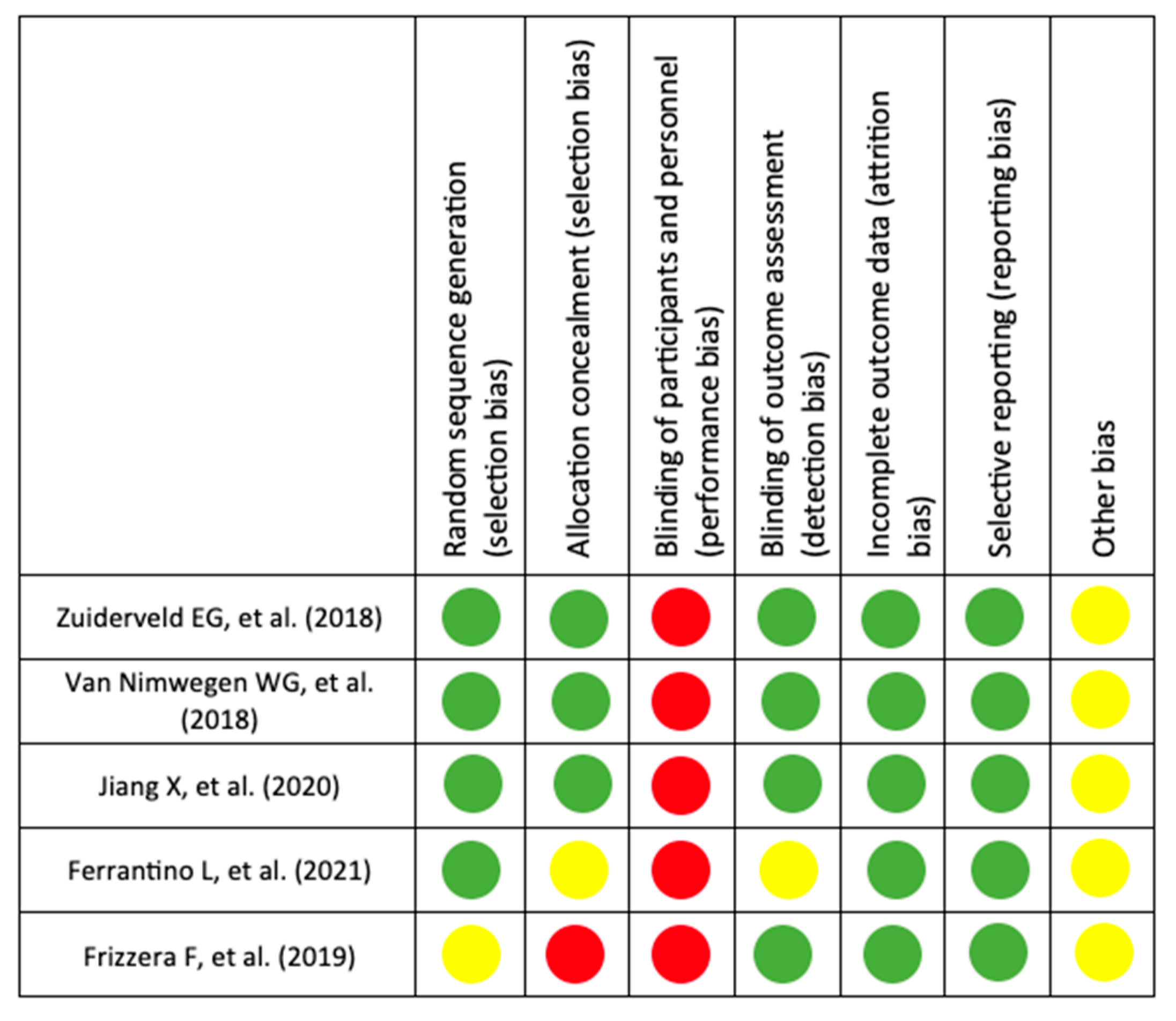
| Author, Year | JADAD | Level of Evidence (OCEBM) | |||||
|---|---|---|---|---|---|---|---|
| Randomization | Adequate Randomization? | Double-Blind | Adequate Masking? | Description of Dropouts | TOTAL (0–5) | ||
| Zuiderveld EG et al. (2018) [28]. | +1 | +1 | 0 | +1 | +1 | 4 | 1 B |
| Van Nimwegen WG et al. (2018) [17]. | +1 | +1 | 0 | +1 | +1 | 4 | 1 B |
| Jiang X et al. (2020) [32]. | +1 | +1 | 0 | +1 | +1 | 4 | 1 B |
| Ferrantino L et al. (2021) [15]. | +1 | +1 | 0 | +1 | +1 | 4 | 1 B |
| Frizzera F et al. (2019) [33]. | +1 | −1 | 0 | +1 | +1 | 2 | 1 B |
| Author (Year), Country. [Type of Study] | Population (Mean Age) | Surgical Procedure and Provisionalization | Parameters Evaluated and Results | Follow-Up | |||||
|---|---|---|---|---|---|---|---|---|---|
| Buccal Gingiva Level (Mean ± ds) | Gum Thickness | Probing Depth (Mean ± ds) | Vestibular Cortical Thickness (Mean ± ds) | Aesthetic Result (Mean ± ds) | Conclusions | ||||
| Zuiderveld EG et al. (2018), Netherlands [28]. [RCT] | 60 SG: 30 (45.5 ± 15.5) CTG of the tuberosity. CG: 30 (47.8 ± 16.5) without CTG. | 1:1 mixture of autologous bone from the tuberosity and xenograft to fill the gap. Provisional crown the same day of surgery, at 20 Nw, and free of contact. After 3 months, the final zirconia crown at 35 Nw. | 12 m −0.5 ± 1.1 mm in the CG and 0.1 ± 0.8 mm in the SG (p = 0.03). | 1st m SG 2.6 ± 1.4 and CG: 2.2 ± 0.9 12 m SG 2.5 ± 1.2 CG: 2.3 ± 0.9. | 12 m PES total mean change at 12 months of 6.8 ± 1.5 in the CG and 6.4 ± 1.5 in the SG. | 1 m and 12 m | Immediately placed and provisionalized implants lead to less recession of the peri-implant soft tissue at the mid-buccal aspect, irrespective of the gingival biotype | ||
| Van Nimwegen WG et al. (2018), Netherlands [17]. [RCT] | 60 SG: 30 (45.5 ± 15.5) with CTG of the tuberosity. CG: 30 (47.8 ± 16.5) without CTG. | 1:1 mixture of autologous bone and bovine xenograft to fill the gap. A provisional crown was placed on the same day of surgery, free of contact. After 3 m, a definitive zirconia crown was placed. | SG: 0.20 ± 0.70 mm CG: −0.48 ± 1.13 mm. | SG −0.68 ± 0.59 mm CG: −0.49 ± 0.54 mm | SG: 2.28 ± 0.79 mm CG: 2.44 ± 1.19 mm | SG Change in level gingival marginal 1.80 ± 0.50 Texture 1.80 ± 0.50 PES total score: 11.28 ± 1.67 CG: Change in level gingival marginal 1.44 ± 0.71 Texture 2.00 ± 0.00 PES total score: 11.36 ± 1.65 | 12 m | CTG cannot fully compensate for the underlying facial bone loss, although a significantly more coronally located mid-facial mucosa level was found when a CTG was performed | |
| Frizzera F et al. (2019), Brazil [33]. [RCT] | 24 SG 1: 8 collagen matrix (Mucograft Geistlich) SG 2: 8 CTG of the palate. CG: 8 | Collagen membrane (bio-guide®) and Bovine bone with 10% porcine collagen (Bio-oss®) to fill the gap between the membrane and the implant. Prefabricated resin crown on the same day of surgery, at 20 N and in infra-occlusion. After 6 m, the final crown was placed. | At 12 m SG 1 −0.28 ± 2.51 mm SG 2 −0.55 ± 3.51 mm CG 0.35 ± 3.69 mm, | SG 1: Baseline of 0.98 ± 0.21 mm, at 6 m of 2.05 ± 0.41 mm, and at 12 m of 2.1 ± 0.54 SG 2: Baseline of 0.98 ± 0.29, at 6 m of 2.82 ± 0.40 and at 12 m of 3.04 ± 0.61 CG: Baseline of 1 ± 0.18, at 6 m of 2.04 ± 0.43, and at 12 m of 2.11 ± 0.60 | SG 1: 1.35 ± 1.38 at 6 m 1.14 ± 1.34 at 12 m SG 2: 1.04 ± 1.01 at 6 m, 1.06 ± 0.87 at 12 m CG: 1.22 ± 0.85 at 6 m, 1.28 ± 0.92 at 12 m | SG 1: At baseline 10.63 ± 1.84 and at 12 m of 10 ± 1.3 SG 2 At baseline 9.37 ± 1.9 and at 12 m of 10.75 ± 1.38 CG 1: Baseline of 10.75 ± 2.05 and at 12 m of 9.87 ± 1.64 | 12 m | The use of a CTG avoided MPR and provided better contour of the alveolar ridge and greater thickness of the soft tissue at the implant facial aspect. | |
| Jiang X et al. (2020), China [32]. [RCT] | 42 SG: 21 (34.3 ± 7.0) CTG of the palate. CG: 21 (37.7 ± 13.3) | The gap was filled with DBBM xenograft (Bio-oss®). Provisionalization was placed in the first 24 h, without occlusal or eccentric contacts. Definitive crown 6 m after surgery. | Coordinates of gingival margin point. SG: (0.63 ± 0.53 mm, 0.16 ± 0.60 mm) at 6 m CG: (0.63 ± 0.55 mm, 0.26 ± 0.54 mm) at 6 m | The buccal plate thickness of the socket was 0.54 ± 0.20 mm for the SG and 0.69 ± 0.30 mm for the CG. | A week, 1 m and 6 m | The CTG used with IIP and provisionalization could compensate for the facial tissue collapse, but it did not benefit the maintenance of the mid-facial gingival margin position | |||
| Ferrantino L et al. (2021), Italy [15]. [RCT] | 60 SG: 31 (47.68 ± 16.50) CTG of the palate or tuberosity. CG: 28 (51.07 ± 14.67) | The gap between the implant and vestibular wall was filled with xenograft (Bio-oss®). A customized resin crown was placed after surgery, free of occlusal contacts. The final restoration was performed 6 m after surgery. | The mean ICAi at 12 m was 4.69 for the SG and 3.45 for the CG. For the items assessing mucosa aesthetics, the SG mean was 1.77, and the CG was 2.27. For the items assessing the ICAI crown, the SG mean was 2.92, and the CG was 1.18. | A week, 1 m, 6 m, and 12 m | CTG is not mandatory to achieve successful aesthetic outcomes for a well-planned immediate implant placement with immediate non-functional provisional restoration in a fresh extraction socket. | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torra-Moneny, M.; Mauri-Obradors, E.; Egido-Moreno, S.; Valls-Roca-Umbert, J.; Marí-Roig, A.; López-López, J. Association of Connective Tissue Grafts in Immediate Implants: Systematic Review and Meta-Analysis. Dent. J. 2024, 12, 183. https://doi.org/10.3390/dj12060183
Torra-Moneny M, Mauri-Obradors E, Egido-Moreno S, Valls-Roca-Umbert J, Marí-Roig A, López-López J. Association of Connective Tissue Grafts in Immediate Implants: Systematic Review and Meta-Analysis. Dentistry Journal. 2024; 12(6):183. https://doi.org/10.3390/dj12060183
Chicago/Turabian StyleTorra-Moneny, Marta, Elisabet Mauri-Obradors, Sonia Egido-Moreno, Joan Valls-Roca-Umbert, Antonio Marí-Roig, and José López-López. 2024. "Association of Connective Tissue Grafts in Immediate Implants: Systematic Review and Meta-Analysis" Dentistry Journal 12, no. 6: 183. https://doi.org/10.3390/dj12060183
APA StyleTorra-Moneny, M., Mauri-Obradors, E., Egido-Moreno, S., Valls-Roca-Umbert, J., Marí-Roig, A., & López-López, J. (2024). Association of Connective Tissue Grafts in Immediate Implants: Systematic Review and Meta-Analysis. Dentistry Journal, 12(6), 183. https://doi.org/10.3390/dj12060183