Materials and Methods for All-Ceramic Dental Restorations Using Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) Technologies—A Brief Review
Abstract
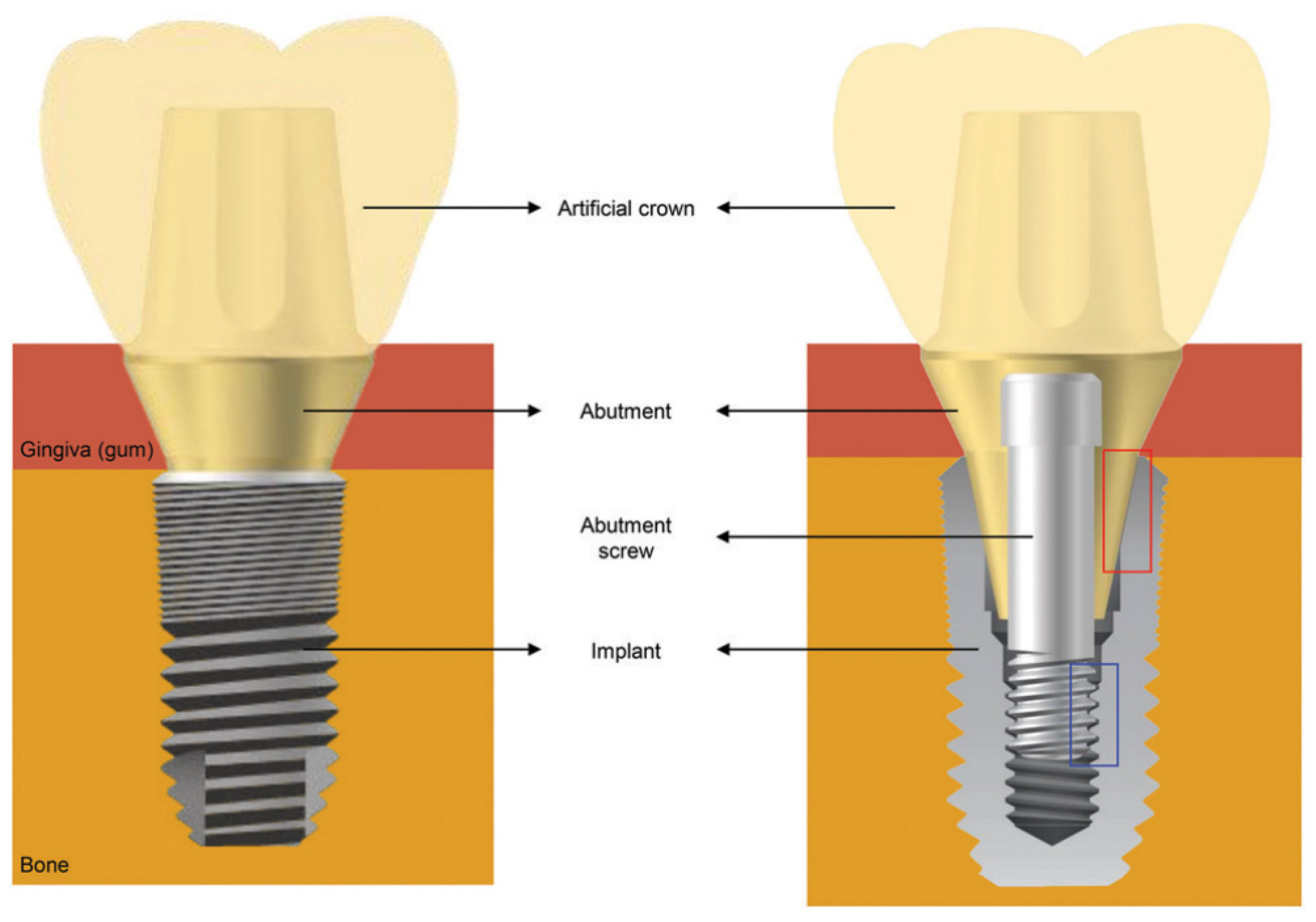
1. Introduction
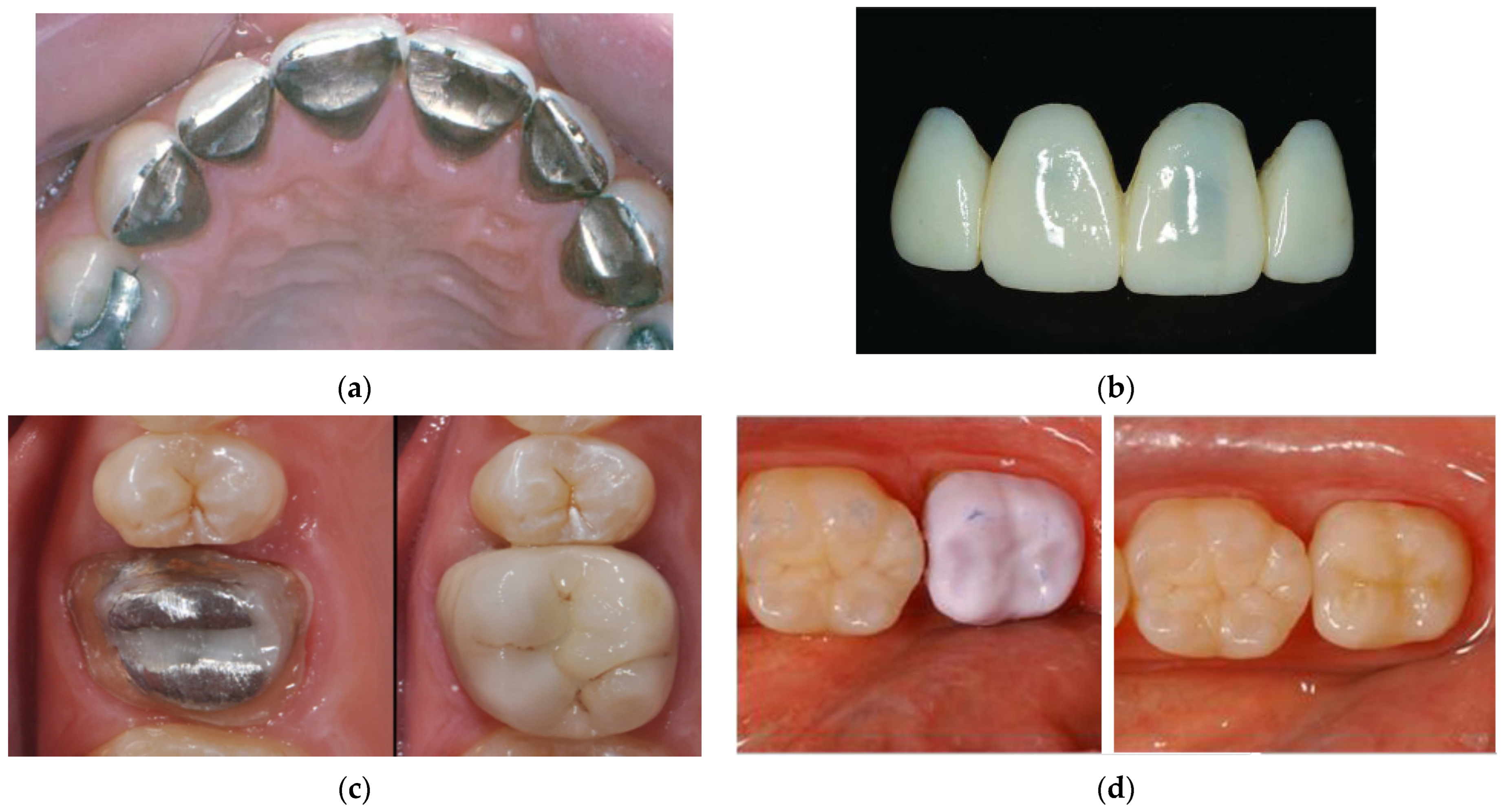
2. Materials Involved in the Manufacturing Process of All-Ceramic Dental Restorations
2.1. Porcelain
2.2. Alumina
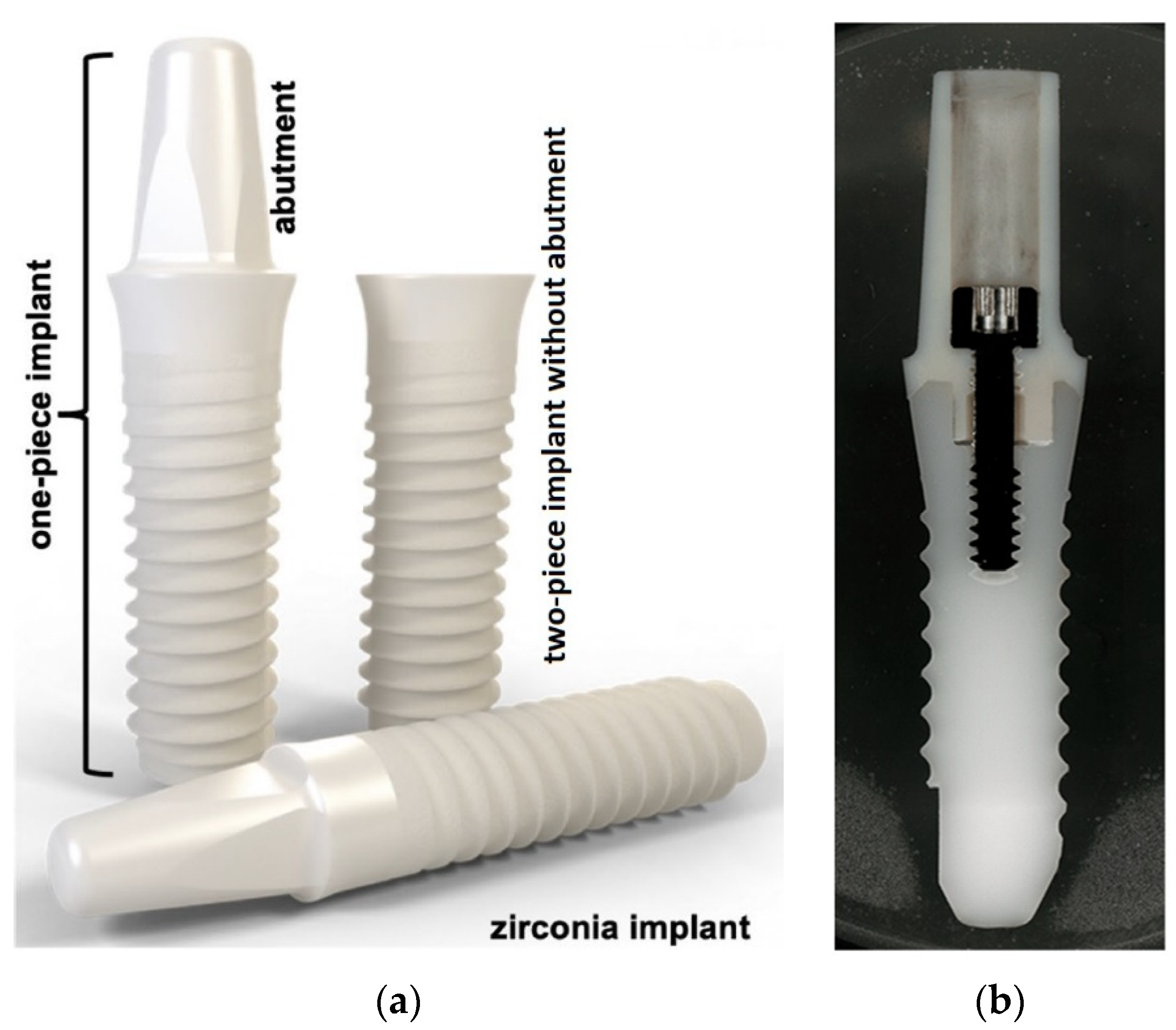
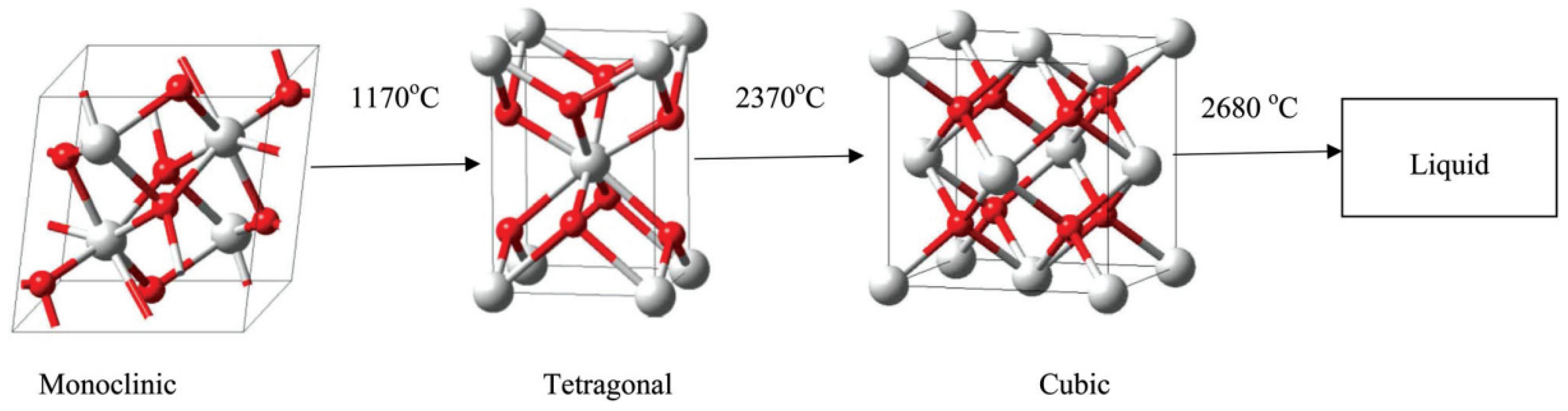
2.3. Zirconium Dioxide
2.4. Lithium Disilicate
3. Methods for the Fabrication of All-Ceramic Restorations
3.1. Conventional Technique
3.2. Heat Hot-Pressing Technique
3.3. Dry-Pressing Method
3.4. Slip-Casting and the Glass Infiltration Method
3.5. CAD/CAM
4. CAD/CAM Technique for Fabrication of Dental Restoration
5. Production of Ceramics Materials for CAD/CAM Dentistry
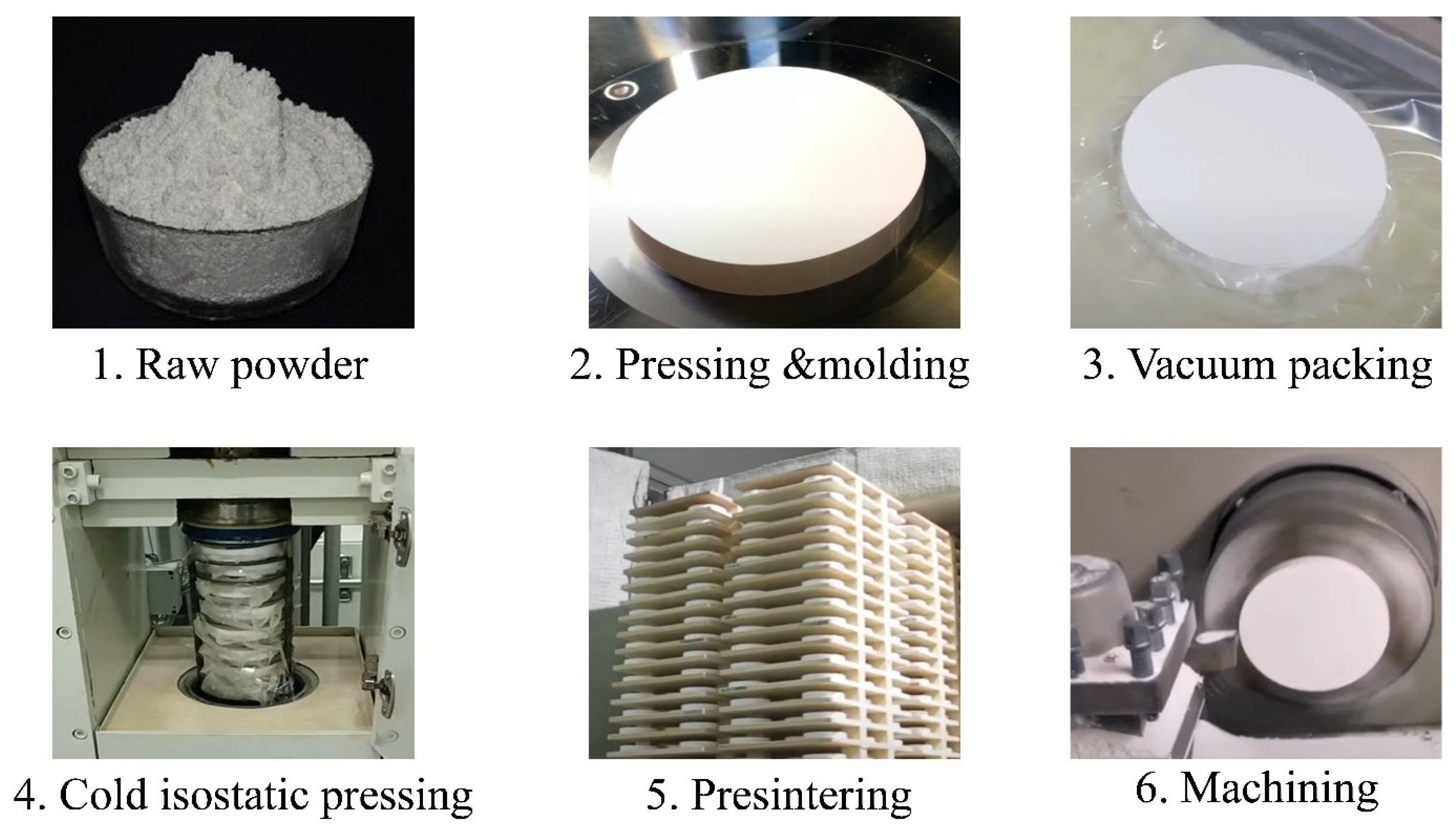
5.1. Production of Zirconium Dioxide CAD/CAM Blocks
5.1.1. Raw Material Process
5.1.2. Green-Forming Process
5.1.3. Pre-Sintering
5.1.4. Block Forming Process
5.1.5. Inspection and Packing
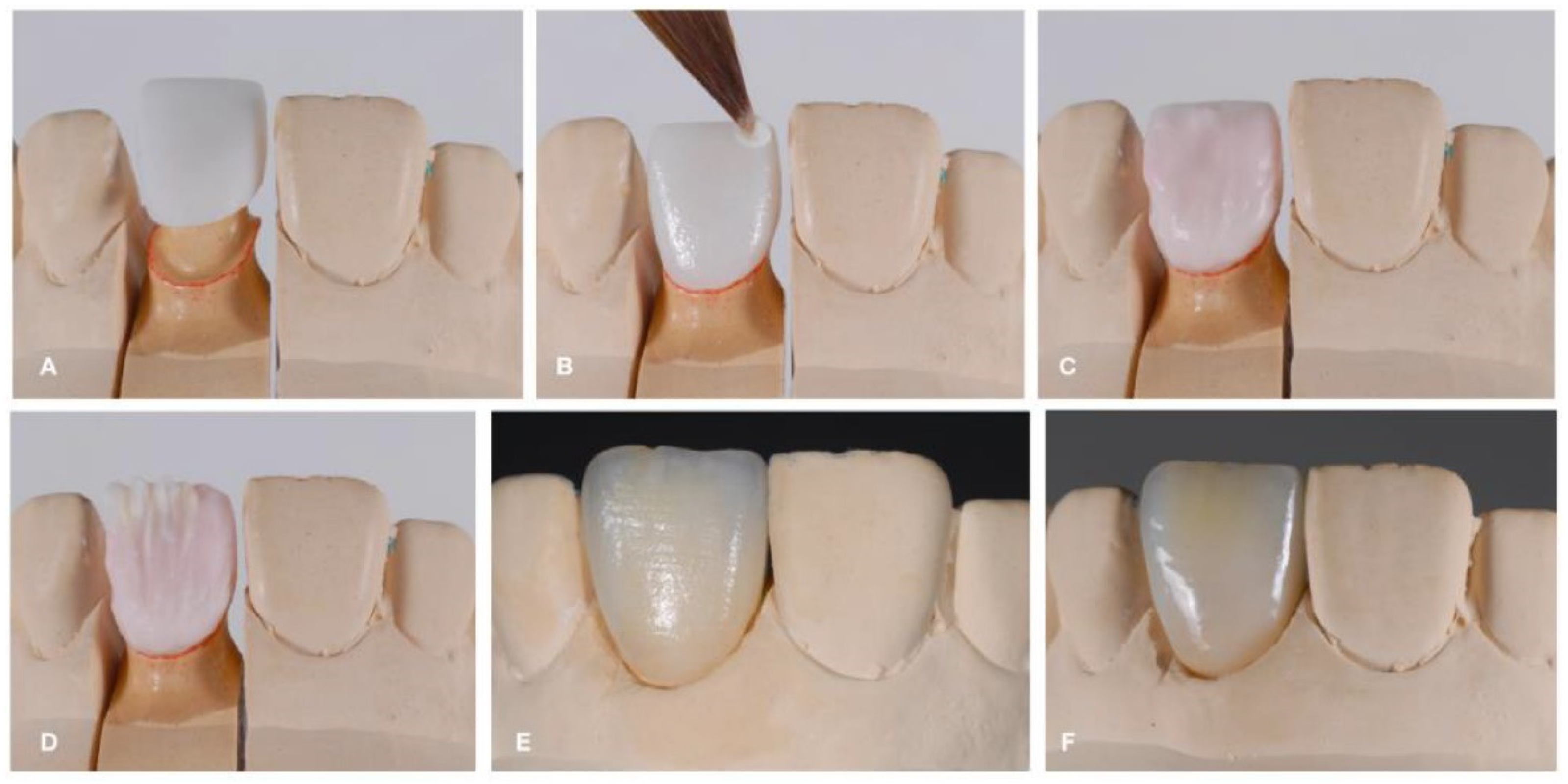
5.2. Production of Glass–Ceramic CAD/CAM Blocks
5.2.1. Raw Material Process
5.2.2. Green-Forming Process
5.2.3. Heating Process
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abraham, C.M. A Brief Historical Perspective on Dental Implants, Their Surface Coatings and Treatments. Open Dent. J. 2014, 8, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.C.; Lee, M.; Yeo, I.-S.L. Three interfaces of the dental implant system and their clinical effects on hard and soft tissues. Mater. Horiz. 2022, 9, 1387. [Google Scholar] [CrossRef] [PubMed]
- Dental Implants: What You Should Know. Available online: https://www.fda.gov/medical-devices/dental-devices/dental-implants-what-you-should-know#:~:text=Dental%20implants%20are%20medical%20devices,crowns%2C%20bridges%2C%20or%20dentures (accessed on 29 September 2023).
- Robertson, K. Types of Dental Implants: Ceramic, Zirconia, and Metal. Available online: https://lwdd.ca/types-of-dental-implants-ceramic-zirconia-and-metal/ (accessed on 29 September 2023).
- Zirconia Dental Implants and Ceramic Implants. Available online: https://naturaldentistrycenter.com/zirconiaimplants/ (accessed on 29 September 2023).
- Cunha, W.; Carvalho, O.; Henriques, B.; Silva, F.S.; Özcan, M.; Souza, J.C.M. Surface modification of zirconia dental implants by laser texturing. Lasers Med. Sci. 2022, 37, 77–93. [Google Scholar] [CrossRef] [PubMed]
- Frigan, K.; Chevalier, J.; Zhang, F.; Spies, B.C. Is a Zirconia Dental Implant Safe When It Is Available on the Market? Ceramics 2019, 2, 568–577. [Google Scholar] [CrossRef]
- Walls, A.; Nohl, F.; Wassell, R. Crowns and other extra-coronal restorations: Resin-bonded metal restorations. Br. Dent. J. 2002, 193, 135–142. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hammond, B.D.; Machowski, M.; Londono, J.; Pannu, D. Fabrication of Porcelain Veneer Provisional Restorations: A Critical Review. Dent. Rev. 2022, 2, 100004. [Google Scholar] [CrossRef]
- Jorquera, G.; Merino, N.; Walls, S.; Mahnand, E.; Fernández, E. Simplified Classification for Dental Ceramics. J. Dent. Sci. Ther. 2016, 1, 22–25. [Google Scholar] [CrossRef]
- Rampf, M.; Höland, W. Glass-ceramics for dental restoration. In Bone Repair Biomaterials; Woodhead Publishing: Sawston, UK, 2019; pp. 329–340. [Google Scholar] [CrossRef]
- Oleszek-Listopad, J.; Sarna-Bos, K.; Szabelska, A.; Czelej-Piszcz, E.; Borowicz, J.; Szymanska, J. The use of gold and gold alloys in prosthetic dentistry—A literature review. Curr. Issues Pharm. Med. Sci. 2015, 28, 192–195. [Google Scholar] [CrossRef]
- Silman, A. Top 6 Types of Dental Crown Material. Available online: https://www.drsilmansmilespa.com/top-6-types-of-dental-crown-material (accessed on 29 September 2023).
- Ozcelik, T.B.; Yilmaz, B. Galvanic gold plating for fixed dental prosthesis. Eur. J. Dent. 2013, 7, 373–376. [Google Scholar] [CrossRef][Green Version]
- Crowns: Common Materials Used for Making Dental Crowns. Available online: https://westcoastinternational.com/crowns-materials-making-dental-crowns.html/ (accessed on 29 September 2023).
- Janyavula, S.; Lawson, N.; Cakir, D.; Beck, P.; Ramp, L.C.; Burgess, J.O. The wear of polished and glazed zirconia against enamel. J. Prosth. Dent. 2013, 109, 22–29. [Google Scholar] [CrossRef]
- Quinn, J.B.; Sundar, V.; Lloyd, I.K. Influence of microstructure and chemistry on the fracture toughness of dental ceramics. Dent. Mater. 2003, 19, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Homaei, E.; Farhangdoost, K.; Tsoi, J.K.; Pow, E.H. Static and fatigue mechanical behavior of three dental CAD/CAM ceramics. J. Mech. Behav. Biomed. Mater. 2016, 59, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Makhija, S.K.; Lawson, N.C.; Gilbert, G.H.; Litaker, M.S.; McClelland, J.A.; Louis, D.R.; Gordan, V.V.; Pihlstrom, D.J.; Meyerowiz, C.; Mungia, R.; et al. Dentist material selection for single-unit crowns: Findings from the National Dental Practice-Based Research Network. J. Dentist. 2016, 55, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Ivoclar. The Pros Make It E.Max. Available online: https://www.ivoclar.com/makeitemax (accessed on 29 September 2023).
- A Brief History of a Great Invention. Advanced Esthetics & High Quality. Available online: https://www.blog.ivoclar.com/lab/en/dental-ceramics-a-brief-history-of-a-great-invention (accessed on 29 September 2023).
- Willard, A.; Gabriel Chu, T.-M. The science and application of IPS e.Max dental ceramic. Kaohsiung J. Med. Sci. 2018, 34, 238–242. [Google Scholar] [CrossRef] [PubMed]
- EMAX Crown: The Best Translucent Dental Material. Available online: https://xdentcenter.com/emax-crown-the-best-translucent-dental-material-2/ (accessed on 29 September 2023).
- E-max Crowns. Available online: https://www.dental-treatment-guide.com/dental-crowns/emax-crowns (accessed on 29 September 2023).
- Davidowitz, G.; Kotick, P.G. The use of CAD/CAM in dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef] [PubMed]
- Javaid, M.; Haleem, A.; Kumar, L. Current status and applications of 3D scanning in dentistry. Clin. Epidemiol. Glob. Health 2018, 7, 228–233. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Eichberger, M.; Kappert, H.F.; Gernet, W.; Edelhoff, D. High-strength CAD/CAM-fabricated veneering material sintered to zirconia copings–a new fabrication mode for all-ceramic restorations. Dent Mater. 2009, 25, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, S. Metal ceramic versus all ceramic restorations: Part I. J. Ir. Dent. Assoc. 2010, 56, 196–199. [Google Scholar] [PubMed]
- Taylor, J.A. History of Dentistry: A Practical Treatise for the Use of Dental Students and Practitioners; Lea & Febiger: Philadelphia, PA, USA, 1922; pp. 142–156. [Google Scholar]
- The History of Dental Crowns. Available online: https://leetrevinodental.com/history-dental-crown/ (accessed on 29 September 2023).
- Helvey, G. A History of Dental Ceramics. Compendium. 2010; Volume 31. Available online: https://www.aegisdentalnetwork.com/cced/2010/05/a-history-of-dental-ceramics (accessed on 29 September 2023).
- Podilsky, N. The History of Dental Crowns. Available online: https://www.cosmeticdentistryedmonton.com/blog/2021/07/22/the-history-of-dental-crowns-210259 (accessed on 29 September 2023).
- McLean, J.W.; Hughes, T.H. The reinforcement of den tal porcelain with ceramic oxides. Br. Dent. J. 1965, 119, 251–267. [Google Scholar]
- Kelly, J.R.; Nishimura, I.; Campbell, S.D. Ceramics in dentistry: Historical roots and current perspectives. J. Prosthet. Dent. 1996, 75, 18–32. [Google Scholar] [CrossRef]
- Leinfelder, K.F.; Kurdziolek, S.M. Contemporary CAD/CAM technologies: The evolution of restorative systems. Pract Proced Aesthet Dent. 2004, 16, 224–231. [Google Scholar] [PubMed]
- Rosenblum, M.A.; Schulman, A. A Review of All-Ceramic Restorations. J. Am. Dent. Assoc. 1997, 128, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Hulbert, S.F.; Bokros, J.C.; Hench, L.L.; Wilson, J.; Heimke, G. Ceramics in clinical applications, past, present and future. In High Tech Ceramics; Vincenzinc, P., Ed.; Elsevier Science: Amsterdam, The Netherlands, 1987; pp. 3–27. [Google Scholar]
- Willmann, G. Ceramic femoral heads retrievals data. Clin. Orthop. Relat. Res. 2000, 379, 173–177. [Google Scholar] [CrossRef]
- Willmann, G.; Von Chamier, W. Bioceramics in Orthopedics: New Applications; Enke Verlag: Stuttgart, Germany, 1998. [Google Scholar]
- Hannouche, D.; Zingg, M.; Miozzari, H.; Nizard, R.; Lübbeke, A. Third-generation pure alumina and alumina matrix composites in total hip arthroplasty: What is the evidence? EFORT Open Rev. 2018, 3, 7–14. [Google Scholar] [CrossRef]
- Willmann, G. Ceramics for total hip replacement–What a surgeon should know. Orthopedics 1998, 21, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Fan, D.; Swain, M.V.; Zhao, K. A systematic review of all-ceramic crowns: Clinical fracture rates in relation to restored tooth type. Int. J. Prosthodont. 2012, 25, 441–450. [Google Scholar]
- Øilo, M.; Gjerdet, N.R. Fractographic analysis of all-ceramic crowns: A study of 27 clinically-fractured crowns. Dent. Mater. 2013, 29, e78–e84. [Google Scholar] [CrossRef] [PubMed]
- Grigoriev, S.; Smirnov, A.; Pinargote, N.W.S.; Yanushevich, O.; Kriheli, N.; Kramar, O.; Pristinskiy, Y.; Peretyagin, P. Evaluation of Mechanical and Electrical Performance of Aging Resistance ZTA Composites Reinforced with Graphene Oxide Consolidated by. SPS. Materials 2022, 15, 2419. [Google Scholar] [CrossRef] [PubMed]
- Smirnov, A.V.; Yushin, D.I.; Pinargote, N.W.S.; Peretyagin, P.Y.; Torrecillas, R. Spark plasma sintering of nanostructured powder materials. Russ. Eng. Res. 2016, 36, 249–254. [Google Scholar] [CrossRef]
- Bona, A.D.; Pecho, O.E.; Alessandretti, R. Zirconia as a Dental Biomaterial. Materials 2015, 8, 4978–4991. [Google Scholar] [CrossRef] [PubMed]
- Grech, J.; Antunes, E. Zirconia in dental prosthetics: A literature review. J. Mater. Res. Technol. 2019, 8, 4956–4964. [Google Scholar] [CrossRef]
- Khodaii, J.; Barazandeh, F.; Rezaei, M.; Adibi, H.; Sarhan, A.A.D. Influence of grinding parameters on phase transformation, surface roughness, and grinding cost of bioceramic partially stabilized zirconia (PSZ) using diamond grinding wheel. Int. J. Adv. Manufact. Technol. 2019, 105, 4715–4729. [Google Scholar] [CrossRef]
- Della Bona, A. Bonding to Ceramics: Scientific Evidences for Clinical Dentistry; Artes Medicas: Sao Paulo, Brazil, 2009. [Google Scholar]
- Becher, P.F.; Swain, M.V. Grain-size-dependent transformation behavior in polycrystalline tetragonal zirconia. J. Am. Ceram. Soc. 1992, 75, 493–502. [Google Scholar] [CrossRef]
- Zhang, Y.; Kelly, J.R. Dental Ceramics for Restoration and Metal Veneering. Dent. Clin. N. Am. 2017, 61, 797–819. [Google Scholar] [CrossRef] [PubMed]
- Smirnov, A.; Solís Pinargote, N.W.; Peretyagin, N.; Pristinskiy, Y.; Peretyagin, P.; Bartolomé, J.F. Zirconia Reduced Graphene Oxide Nano-Hybrid Structure Fabricated by the Hydrothermal Reaction Method. Materials 2020, 13, 687. [Google Scholar] [CrossRef] [PubMed]
- Žmak, I.; Ćorić, D.; Mandić, V.; Ćurković, L. Hardness and Indentation Fracture Toughness of Slip Cast Alumina and Alumina-Zirconia Ceramics. Materials 2019, 13, 122. [Google Scholar] [CrossRef] [PubMed]
- Shahmiri, R.; Standard, O.C.; Hart, J.N.; Sorrell, C.C. Optical properties of zirconia ceramic for esthetic dental restorations: A systemic review. J. Prosthet. Dent. 2018, 119, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Saridan, S.; Tak, O.; Alniacik, G. Basic properties and types of zirconia: An overview. World J. Stomatol. 2013, 2, 40–47. [Google Scholar] [CrossRef]
- Guazzato, M.; Albakry, M.; Ringer, S.P.; Swain, M.V. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part, I. Pressable and alumina glass-infiltrated ceramics. Dent. Mater. 2004, 20, 441e8. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R.; Benetti, P. Ceramic materials in dentistry: Historical evolution and current practice. Aust. Dent. J. 2011, 56, 84e96. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, N. Optical Properties of Lithium Disilicate Glass Ceramic in Different Firing Temperatures and Thicknesses. Master's Thesis, Department of Prosthodontics, Indiana University School of Dentistry, Indianapolis, IN, USA, 2016; p. 130. [Google Scholar] [CrossRef]
- Vivadent Ivoclar. Scientific Documentaion IPS e.max CAD. Liechtenstein. 2011. Available online: https://ivodent.hu/__docs/768_865d8476b1360c8ac461ae57f9c6b3c4.pdf (accessed on 21 February 2024).
- Srinivasa, R.D.; Rama, K.A.; Venkata, R.A.; Jithendra, B.P.; Anusha, K. Dental Ceramics: Part II–Recent Advances in Dental Ceramics. Am. J. Mater. Eng. Technol. 2015, 3, 19–26. [Google Scholar]
- Ritter, R.G. Multifunctional uses of a novel ceramic-lithium disilicate. J. Esthet. Restor. Dent. 2010, 22, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Rizkalla, A.S.; Jones, D.W. Mechanical properties of commercial high strength ceramic core materials. Dent. Mater. 2004, 20, 207–212. [Google Scholar] [CrossRef]
- Culp, L.; McLaren, E.A. Lithium disilicate: The restorative material of multiple options. Compend. Contin. Educ. Dent. 2010, 31, 716–725. [Google Scholar] [PubMed]
- Yang, Y.; Yu, J.; Gao, J.; Guo, J.; Li, L.; Zhao, Y.; Zhang, S. Clinical outcomes of different types of tooth-supported bilayer lithium disilicate all-ceramic restorations after functioning up to 5 years: A retrospective study. J. Dent. 2016, 51, 56–61. [Google Scholar] [CrossRef]
- Valenti, M.; Valenti, A. Retrospective survival analysis of 261 lithium disilicate crowns in a private general practice. Quintessence Int. 2009, 40, 573–579. [Google Scholar]
- Li, R.W.; Chow, T.W.; Matinlinna, J.P. Ceramic dental biomaterials and CAD/CAM technology: State of the art. J. Prosthodont. Res. 2014, 58, 208.e16. [Google Scholar] [CrossRef] [PubMed]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral Health 2019, 19, 134. [Google Scholar] [CrossRef] [PubMed]
- Fabian Fonzar, R.; Carrabba, M.; Sedda, M.; Ferrari, M.; Goracci, C.; Vichi, A. Flexural resistance of heat-pressed and CAD-CAM lithium disilicate with different translucencies. Dent. Mater. 2017, 33, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Puri, S. Techniques used to fabricate all-ceramic restorations in the dental practice. Compend. Contin. Educ. Dent. 2005, 26, 519–525. [Google Scholar] [PubMed]
- de Matos, J.D.M.; Lopes, G.R.S.; Queiroz, D.A.; Nakano, L.J.N.; Ribeiro, N.C.R.; Barbosa, A.B.; Anami, L.C.; Bottino, M.A. Dental Ceramics: Fabrication Methods and Aesthetic Characterization. Coatings 2022, 12, 1228. [Google Scholar] [CrossRef]
- Sharkey, S. Metal-ceramic versus all-ceramic restorations: Part III. J. Ir. Dent. Assoc. 2011, 57, 110–113. [Google Scholar] [PubMed]
- Jithendra, B.P.; Rama, K.A.; Venkata, R.A.; Srinivasa, R.D.; Anusha, K. Dental Ceramics: Part I – An Overview of Composition, Structure and Properties. Am. J. Mater. Eng. Technol. 2015, 3, 1318. Available online: http://pubs.sciepub.com/materials/3/1/3 (accessed on 21 February 2024).
- Ritzberger, C.; Apel, E.; Ho¨land, W.; Peschke, A.; Rheinberger, V.M. Properties and Clinical Application of Three Types of Dental Glass-Ceramics and Ceramics for CAD-CAM Technologies. Materials 2010, 3, 3700–3713. [Google Scholar] [CrossRef]
- Andersson, M.; Oden, A. A new all-ceramic crown. A densesintered, high purity alumina coping with porcelain. Acta Odontol. Scand. 1993, 51, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Aboushelib, M.N.; de Jagger, N.; Kleverlaan, C.J.; Feilzer, A.J. Microtensile bond strength of different components of core veneered all-ceramic restorations. Dent. Mater. 2005, 21, 984–991. [Google Scholar] [CrossRef] [PubMed]
- VITA In-Ceram Classic SPINELL. Available online: http://www.artdentallab.com.br/pdf/manual/spinell_va.pdf (accessed on 29 September 2023).
- Mormann, W.H. The evolution of the CEREC system. J. Am. Dent. Assoc. 2006, 137, 7S–13S. [Google Scholar] [CrossRef]
- Vereschaka, A.S.; Grigoriev, S.N.; Sotova, E.S.; Vereschaka, A.A. Improving the efficiency of the cutting tools made of mixed ceramics by applying modifying nano-scale multilayered coatings. Adv. Mat. Res. 2013, 712–715, 391–394. [Google Scholar] [CrossRef]
- Vereschaka, A.A.; Grigoriev, S.N.; Volosova, M.A.; Batako, A.; Vereschaka, A.A.; Sitnikov, N.N.; Seleznev, A.E. Nano-scale multi-layered coatings for improved efficiency of ceramic cutting tools. Int. J. Adv. Manuf. Technol. 2017, 90, 27–43. [Google Scholar] [CrossRef]
- Grigoriev, S.N.; Volosova, M.A.; Vereschaka, A.A.; Sitnikov, N.N.; Milovich, F.; Bublikov, J.I.; Fyodorov, S.V.; Seleznev, A.E. Properties of (Cr,Al,Si)N-(DLC-Si) composite coatings deposited on a cutting ceramic substrate. Ceram. Int. 2020, 46, 18241–18255. [Google Scholar] [CrossRef]
- Volosova, M.; Grigoriev, S.; Metel, A.; Shein, A. The Role of Thin-Film Vacuum-Plasma Coatings and Their Influence on the Efficiency of Ceramic Cutting Inserts. Coatings 2018, 8, 287. [Google Scholar] [CrossRef]
- Grigoriev, S.N.; Volosova, M.A.; Fedorov, S.V.; Okunkova, A.A.; Pivkin, P.M.; Peretyagin, P.Y.; Ershov, A.A. Development of DLC-Coated Solid SiAlON/TiN Ceramic End Mills for Nickel Alloy Machining: Problems and Prospects. Coatings 2021, 11, 532. [Google Scholar] [CrossRef]
- Mörmann, W.H.; Bindl, A. All-ceramic, chair-side computer-aided design/computer-aided machining restorations. Dent. Clin. N. Am. 2002, 46, 405–426. [Google Scholar] [CrossRef]
- The Use of CAD/CAM in Dentistry. Available online: https://pocketdentistry.com/the-use-of-cadcam-in-dentistry/ (accessed on 29 September 2023).
- Baroudi, K.; Ibraheem, S.N. Assessment of Chair-side Computer-Aided Design and Computer-Aided Manufacturing Restorations: A Review of the Literature. J. Int. Oral Health 2015, 7, 96–104. [Google Scholar] [PubMed]
- Denry, I.; Kelly, J.R. State of the art of zirconia for dental applications. Dent. Mater. 2008, 24, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Tomova, Z.; Zhekov, Y.; Alexandrov, G.; Vlahova, A.; Vasileva, E. Application of CAD/CAM technologies and materials for prosthetic restoration of severely damaged teeth—Clinical cases. Aust. Dent. J. 2023, 68, 294–302. [Google Scholar] [CrossRef]
- Dao-Ngoc, L. Re: What Are the Engineering Ways Zirconia Block (Used Later in Fabrication of CAD CAM FDP PRosthesis) Manufactured? Available online: https://www.researchgate.net/post/What-are-the-engineering-ways-zirconia-block-used-later-in-fabrication-of-CAD-CAM-FDP-PRosthesis-manufactured/5e0d864e36d2350c03340e36/citation/download (accessed on 21 February 2024).
- Ivoclar. Production of Glass-Ceramic CAD/CAM Blocks. Available online: https://www.youtube.com/watch?v=0luQ2LWYBKw (accessed on 29 September 2023).





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Solís Pinargote, N.W.; Yanushevich, O.; Krikheli, N.; Smirnov, A.; Savilkin, S.; Grigoriev, S.N.; Peretyagin, P. Materials and Methods for All-Ceramic Dental Restorations Using Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) Technologies—A Brief Review. Dent. J. 2024, 12, 47. https://doi.org/10.3390/dj12030047
Solís Pinargote NW, Yanushevich O, Krikheli N, Smirnov A, Savilkin S, Grigoriev SN, Peretyagin P. Materials and Methods for All-Ceramic Dental Restorations Using Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) Technologies—A Brief Review. Dentistry Journal. 2024; 12(3):47. https://doi.org/10.3390/dj12030047
Chicago/Turabian StyleSolís Pinargote, Nestor Washington, Oleg Yanushevich, Natella Krikheli, Anton Smirnov, Sergey Savilkin, Sergey N. Grigoriev, and Pavel Peretyagin. 2024. "Materials and Methods for All-Ceramic Dental Restorations Using Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) Technologies—A Brief Review" Dentistry Journal 12, no. 3: 47. https://doi.org/10.3390/dj12030047
APA StyleSolís Pinargote, N. W., Yanushevich, O., Krikheli, N., Smirnov, A., Savilkin, S., Grigoriev, S. N., & Peretyagin, P. (2024). Materials and Methods for All-Ceramic Dental Restorations Using Computer-Aided Design (CAD) and Computer-Aided Manufacturing (CAM) Technologies—A Brief Review. Dentistry Journal, 12(3), 47. https://doi.org/10.3390/dj12030047






