Effect of Duplication Techniques on the Fitting Accuracy of CAD-CAM Milled, 3D-Printed, and Injection-Molded Mandibular Complete Denture Bases
Abstract
1. Introduction
2. Materials and Methods
Denture Duplication
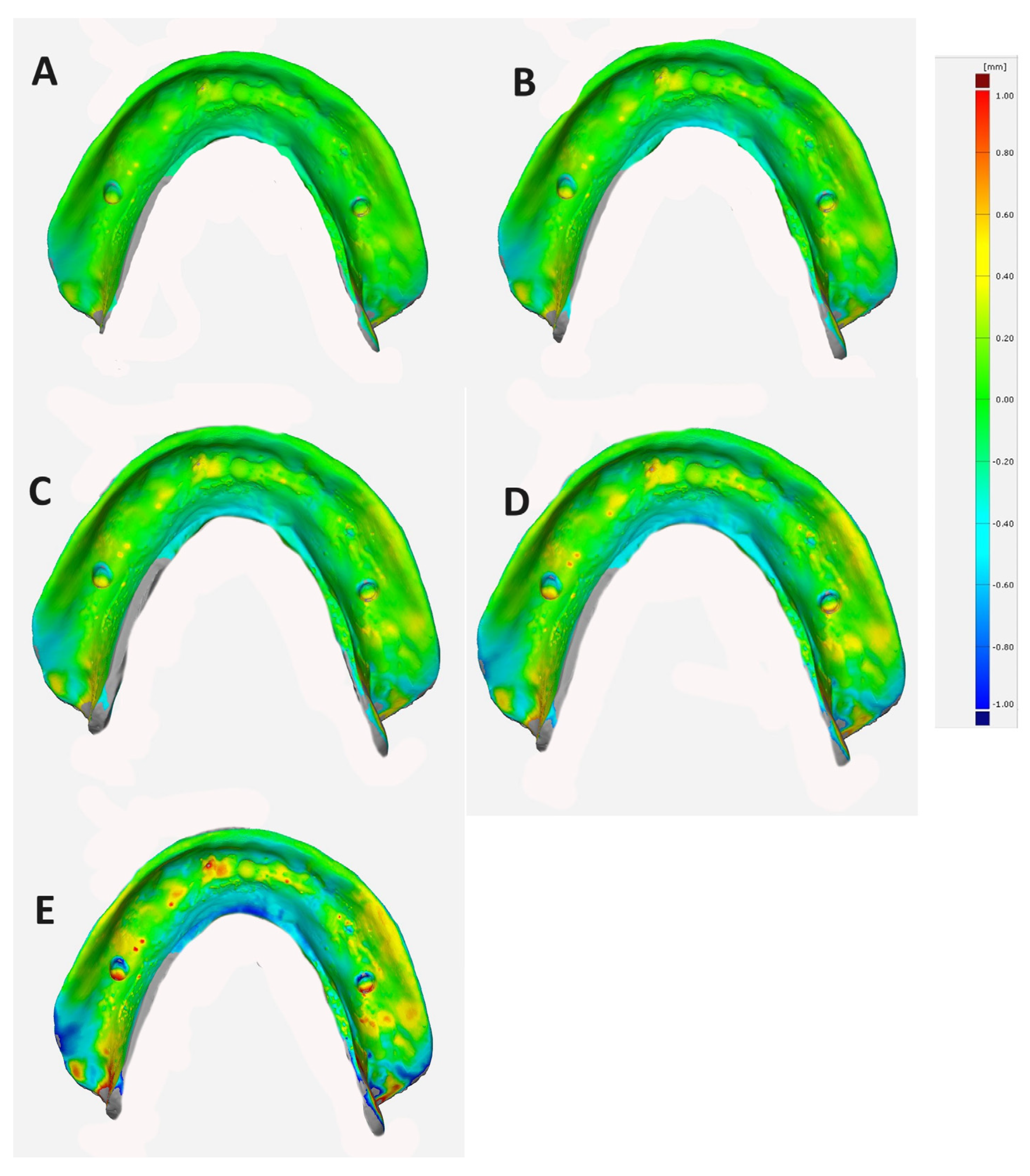
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, L.; Li, D.; Zhou, J.; Lin, W.S.; Tan, J. Duplicating complete dentures with conventional and digital methods: Comparisons of trueness and efficiency. Dent. J. 2022, 10, 35. [Google Scholar] [CrossRef]
- Roessler, D.M. Complete denture success for patients and dentists. Int. Dent. J. 2003, 53, 340–345. [Google Scholar] [CrossRef]
- Mijiritsky, E.; Ben Zaken, H.; Shacham, M.; Cinar, I.C.; Tore, C.; Nagy, K.; Ganz, S.D. Variety of surgical guides and protocols for bone reduction prior to implant placement: A narrative review. Int. J. Environ. Res. Public. Health 2021, 18, 2341. [Google Scholar] [CrossRef]
- Haralur, S.B. Clinical strategies for complete denture rehabilitation in a patient with Parkinson disease and reduced neuromuscular control. Case Rep. Dent. 2015, 2015, 352878. [Google Scholar] [CrossRef]
- Chen, Y.; Luo, Z.; Sun, Y.; Zhou, Y.; Han, Z.; Yang, X.; Kang, X.; Lin, J.; Qi, B.; Lin, W.W.; et al. The effect of denture-wearing on physical activity is associated with cognitive impairment in the elderly: A cross-sectional study based on the CHARLS database. Front. Neurosci. 2022, 16, 925398. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture base adaptation between CAD-CAM and conventional fabrication techniques. J. Prosthet. Dent. 2016, 116, 249–256. [Google Scholar] [CrossRef]
- Soo, S.; Cheng, A.C. Complete denture copy technique-A practical application. Singapore Dent. J. 2014, 35, 65–70. [Google Scholar] [CrossRef]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef]
- Villias, A.; Karkazis, H.; Yannikakis, S.; Theocharopoulos, A.; Sykaras, N.; Polyzois, G. Current status of digital complete dentures technology. Prosthesis 2021, 3, 229–244. [Google Scholar] [CrossRef]
- Lee, S.; Hong, S.J.; Paek, J.; Pae, A.; Kwon, K.R.; Noh, K. Comparing accuracy of denture bases fabricated by injection molding, CAD/CAM milling, and rapid prototyping method. J. Adv. Prosthodont. 2019, 11, 55–64. [Google Scholar] [CrossRef]
- Helal, M.A.; Al-Gazzar, A.E.; Abas, M.; Akhtar, S.; Gad, M.M.; Al-Thobity, A.M. Comparative Effect of Different Surface Treatments on the Shear Bond Strength of Two Types of Artificial Teeth Bonded To Two Types of Denture Base Resins. J. Prosthodont. 2022, 31, 427–433. [Google Scholar] [CrossRef]
- Clark, W.A.; Duqum, I.; Kowalski, B.J. The digitally replicated denture technique: A case report. J. Esthet. Restor. Dent. 2019, 31, 20–25. [Google Scholar] [CrossRef]
- Ammoun, R.; Bencharit, S. Creating a digital duplicate denture file using a desktop scanner and an open-source software program: A dental technique. J. Prosthet. Dent. 2021, 125, 402–406. [Google Scholar] [CrossRef]
- Renne, W.; Revell, G.; Teich, S. The digital denture replication method (DRM): A simplified method to fabricate a complete removable prosthesis. Quintessence Int. 2020, 51, 838–843. [Google Scholar] [CrossRef]
- Takeda, Y.; Lau, J.; Nouh, H.; Hirayama, H. A 3D printing replication technique for fabricating digital dentures. J. Prosthet. Dent. 2020, 124, 251–256. [Google Scholar] [CrossRef]
- Fekri, L.K.; Abdelaziz, M.S. Digital duplication of maxillary complete denture: A dental technique. J. Esthet. Restor. Dent. 2023, 35, 1139–1143. [Google Scholar] [CrossRef]
- Alehaideb, A.; Lin, W.S.; Levon, J.A.; Chu, T.G.; Yang, C.C. Accuracy of digital duplication scanning methods for complete dentures. J. Prosthodont. 2023. early view. [Google Scholar] [CrossRef]
- Zeidan, A.A.; Sherif, A.F.; Baraka, Y.; Abualsaud, R.; Abdelrahim, R.A.; Gad, M.M.; Helal, M.A. Evaluation of the Effect of Different Construction Techniques of CAD-CAM Milled, 3D-Printed, and Polyamide Denture Base Resins on Flexural Strength: An In Vitro Comparative Study. J. Prosthodont. 2023, 32, 77–82. [Google Scholar] [CrossRef]
- Helal, M.A.; Fadl-Alah, A.; Baraka, Y.M.; Gad, M.M.; Emam, A.M. In-vitro comparative evaluation for the surface properties and impact strength of CAD/CAM milled, 3D printed, and polyamide denture base resins. J. Int. Soc. Prev. Community Dent. 2022, 12, 126–131. [Google Scholar] [CrossRef]
- Hsu, C.-Y.; Yang, T.-C.; Wang, T.-M.; Lin, L.D. Effects of fabrication techniques on denture base adaptation: An in vitro study. J. Prosthet. Dent. 2020, 124, 740–747. [Google Scholar] [CrossRef]
- Kalberer, N.; Mehl, A.; Schimmel, M.; Müller, F.; Srinivasan, M. CAD-CAM milled versus rapidly prototyped (3-D-printed) complete dentures: An in vitro evaluation of trueness. J. Prosthet. Dent. 2019, 121, 637–643. [Google Scholar] [CrossRef]
- Bud, E.S.; Bocanet, V.I.; Muntean, M.H.; Vlasa, A.; Bucur, S.M.; Păcurar, M.; Dragomir, B.R.; Olteanu, C.D.; Bud, A. Accuracy of three-dimensional (3d) printed dental digital models generated with three types of resin polymers by extra-oral optical scanning. J. Clin. Med. 2021, 10, 1908. [Google Scholar] [CrossRef]
- Negm, E.E.; Aboutaleb, F.A.; Alam-Eldein, A.M. Virtual evaluation of the accuracy of fit and trueness in maxillary poly(etheretherketone) removable partial denture frameworks fabricated by direct and indirect CAD/CAM techniques. J. Prosthodont. 2019, 28, 804–810. [Google Scholar] [CrossRef]
- Lamfon, H.A.; Hamouda, I.M. Maxillary denture flange and occlusal discrepancies of Vertex ThermoSens in comparison with conventional heat-cured denture base materials. J. Biomed. Res. 2019, 33, 139–144. [Google Scholar] [CrossRef]
- Yang, Y.; Yang, Z.; Lin, W.-S.; Chen, L.; Tan, J. Digital duplication and 3d printing for implant overdenture fabrication. J. Prosthodont. 2021, 30, 139–142. [Google Scholar] [CrossRef]
- Adali, U.; Peroz, S.; Schweyen, R.; Hey, J. Replica denture technique: Improvements through the use of CAD-CAM technology. Int. J. Comput. Dent. 2021, 24, 439–448. [Google Scholar]
- Chintalacheruvu, V.K.; Balraj, R.U.; Putchala, L.S.; Pachalla, S. Evaluation of three different processing techniques in the fabrication of complete dentures. J. Int. Soc. Prev. Community Dent. 2017, 7, 18–23. [Google Scholar] [CrossRef]
- Habib, S.R. Replacing existing dentures by copy-denture technique for geriatric patients: A case report. JPDA 2013, 22, 265–269. [Google Scholar]
- AlRumaih, H.S. Clinical applications of intraoral scanning in removable prosthodontics: A literature review. J. Prosthodont. 2021, 30, 747–762. [Google Scholar] [CrossRef]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D printing in dentistry: Technologies, affecting factors, and applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef]
- Hwangbo, N.K.; Nam, N.E.; Choi, J.H.; Kim, J.E. Effects of the washing time and washing solution on the biocompatibility and mechanical properties of 3D printed dental resin materials. Polymers 2021, 13, 4410. [Google Scholar] [CrossRef]
- Katheng, A.; Kanazawa, M.; Komagamine, Y.; Iwaki, M.; Namano, S.; Minakuchi, S. Effect of post-rinsing time and method on accuracy of denture base manufactured with stereolithography. J. Adv. Prosthodont. 2022, 14, 45–55. [Google Scholar] [CrossRef]
- Oyamada, Y.; Yonezawa, Y.; Kondo, H. Simple duplication technique of complete denture using an intraoral scanner. J. Prosthodont. 2021, 30, 458–461. [Google Scholar] [CrossRef]
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef]
- Artopoulos, A.; Juszczyk, A.S.; Rodriguez, J.M.; Clark, R.K.; Radford, D.R. Three-dimensional processing deformation of three denture base materials. J. Prosthet. Dent. 2013, 110, 481–487. [Google Scholar] [CrossRef]
- Helal, M.A.; Abd Elrahim, R.A.; Zeidan, A.A. Comparison of Dimensional Changes Between CAD-CAM Milled Complete Denture Bases and 3D Printed Complete Denture Bases: An In Vitro Study. J. Prosthodont. 2023, 32, 11–19. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors influencing the dimensional accuracy of 3d-printed full-coverage dental restorations using stereolithography technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef]
- Jeong, Y.G.; Lee, W.S.; Lee, K.B. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J. Adv. Prosthodont. 2018, 10, 245–251. [Google Scholar] [CrossRef]
- Schubert, O.; Edelhoff, D.; Erdelt, K.J.; Nold, E.; Güth, J.F. Accuracy of surface adaptation of complete denture bases fabricated using milling, material jetting, selective laser sintering, digital light processing, and conventional injection molding. Int. J. Comput. Dent. 2022, 25, 151–159. [Google Scholar] [CrossRef]
- Li, D.; Yang, S.T.; Yuan, Q.; Mo, A.C.; Yue, L. Accuracy and retention of denture bases fabricated by injection molding, milling, and three-dimensional printing. Zhonghua Kou Qiang Yi Xue Za Zhi. 2022, 57, 927–931. (In Chinese) [Google Scholar] [CrossRef]
- Einarsdottir, E.R.; Geminiani, A.; Chochlidakis, K.; Feng, C.; Tsigarida, A.; Ercoli, C. Dimensional stability of double-processed complete denture bases fabricated with compression molding, injection molding, and CAD-CAM subtraction milling. J. Prosthet. Dent. 2020, 124, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Kane, B.; Shah, K.C. In Vitro Analysis of Shear Stress: CAD Milled vs. Printed Denture Base Resins with Bonded Denture Tooth. J. Prosthodont. 2023, 32, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Tzanakakis, E.G.; Pandoleon, P.; Sarafianou, A.; Kontonasaki, E. Adhesion of Conventional, 3D-Printed and Milled Artificial Teeth to Resin Substrates for Complete Dentures: A Narrative Review. Polymers 2023, 15, 2488. [Google Scholar] [CrossRef] [PubMed]


| Measurement Points | ANOVA Test | Tukey’s Post Hoc Test | |||||
|---|---|---|---|---|---|---|---|
| Variable | Mean + SD (mm) | p | Pairwise-Comparison | p | |||
| Antero-posterior | A–B | Reference Denture | 1 | (33.07) | 0.000 * | G 1 vs. G 2 | 0.012 |
| G1 (AvaDent) | 10 | 33.06 ± 0.11 | G 1 vs. G 3 | 0.000 | |||
| G2 (IvoBase) | 10 | 32.88 ± 0.08 | G 1 vs. G 4 | 0.000 | |||
| G3 (NextDent) | 10 | 32.70 ± 0.07 | G 1 vs. G 5 | 0.000 | |||
| G4 (Harzlab) | 10 | 32.68 ± 0.08 | G 2 vs. G 3 | 0.013 | |||
| G5 (iFlext) | 10 | 32.51 ± 0.15 | G 2 vs. G 4 | 0.006 | |||
| G 2 vs. G 5 | 0.000 | ||||||
| G 3 vs. G 4 | 0.764 | ||||||
| G 3 vs. G 5 | 0.010 | ||||||
| G 4 vs. G 5 | 0.019 | ||||||
| A–C | Reference Denture | 1 | (32.00) | 0.000 * | G 1 vs. G 2 | 0.002 | |
| G 1 | 10 | 31.99 ± 0.07 | G 1 vs. G 3 | 0.000 | |||
| G 2 | 10 | 31.69 ± 0.09 | G 1 vs. G 4 | 0.000 | |||
| G 3 | 10 | 31.30 ± 0.07 | G 1 vs. G 5 | 0.000 | |||
| G 4 | 10 | 31.30 ± 0.12 | G 2 vs. G 3 | 0.000 | |||
| G 5 | 10 | 29.38 ± 0.22 | G 2 vs. G 4 | 0.000 | |||
| G 2 vs. G 5 | 0.000 | ||||||
| G 3 vs. G 4 | 0.000 | ||||||
| G 3 vs. G 5 | 0.000 | ||||||
| G 4 vs. G 5 | 0.000 | ||||||
| Medio-lateral | B–C | Reference Denture | 1 | (47.20) | 0.000 * | G 1 vs. G 2 | 0.000 |
| G 1 | 10 | 47.09 ± 0.14 | G 1 vs. G 3 | 0.000 | |||
| G 2 | 10 | 46.8 ± 0.02 | G 1 vs. G 4 | 0.000 | |||
| G 3 | 10 | 46.29 ± 0.04 | G 1 vs. G 5 | 0.000 | |||
| G 4 | 10 | 45.89 ± 0.07 | G 2 vs. G 3 | 0.000 | |||
| G 5 | 10 | 45.34 ± 0.15 | G 2 vs. G 4 | 0.000 | |||
| G 2 vs. G 5 | 0.000 | ||||||
| G 3 vs. G 4 | 0.000 | ||||||
| Denture Base Resins | Mean ± SD Mm | ANOVA Test | Tukey’s Post Hoc Test | ||
|---|---|---|---|---|---|
| Milled | G 1 | 0.155 ± 0.004 | 0.000 | G 2 | 0.000 |
| G 3 | 0.000 | ||||
| G 4 | 0.000 | ||||
| G 5 | 0.000 | ||||
| G 2 | 0.191 ± 0.002 | G 1 | 0.000 | ||
| G 3 | 0.000 | ||||
| G 4 | 0.000 | ||||
| G 5 | 0.000 | ||||
| 3D Printed | G 3 | 0.236 ± 0.111 | G 1 | 0.000 | |
| G 2 | 0.000 | ||||
| G 4 | 0.000 | ||||
| G 5 | 0.000 | ||||
| G 4 | 0.296 ± 0.005 | G 1 | 0.000 | ||
| G 2 | 0.000 | ||||
| G 3 | 0.000 | ||||
| G 5 | 0.000 | ||||
| Injected | G 5 | 0.626 ± 0.186 | G 1 | 0.000 | |
| G 2 | 0.000 | ||||
| G 3 | 0.000 | ||||
| G 4 | 0.000 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Emam, A.-N.M.; El-Esawy, A.A.; Alyami, M.H.; Baraka, Y.; Gad, M.M.; Helal, M.A. Effect of Duplication Techniques on the Fitting Accuracy of CAD-CAM Milled, 3D-Printed, and Injection-Molded Mandibular Complete Denture Bases. Dent. J. 2024, 12, 32. https://doi.org/10.3390/dj12020032
Emam A-NM, El-Esawy AA, Alyami MH, Baraka Y, Gad MM, Helal MA. Effect of Duplication Techniques on the Fitting Accuracy of CAD-CAM Milled, 3D-Printed, and Injection-Molded Mandibular Complete Denture Bases. Dentistry Journal. 2024; 12(2):32. https://doi.org/10.3390/dj12020032
Chicago/Turabian StyleEmam, Abdel-Naser M., Ahmed Ayman El-Esawy, Mohammed Hamad Alyami, Yasser Baraka, Mohammed M. Gad, and Mohamed Ahmed Helal. 2024. "Effect of Duplication Techniques on the Fitting Accuracy of CAD-CAM Milled, 3D-Printed, and Injection-Molded Mandibular Complete Denture Bases" Dentistry Journal 12, no. 2: 32. https://doi.org/10.3390/dj12020032
APA StyleEmam, A.-N. M., El-Esawy, A. A., Alyami, M. H., Baraka, Y., Gad, M. M., & Helal, M. A. (2024). Effect of Duplication Techniques on the Fitting Accuracy of CAD-CAM Milled, 3D-Printed, and Injection-Molded Mandibular Complete Denture Bases. Dentistry Journal, 12(2), 32. https://doi.org/10.3390/dj12020032







