Camouflage Correction of Skeletal Class III Severe Open Bite with Tooth Ankylosis Treated by Temporary Anchorage Devices: A Case Report
Abstract
1. Introduction
2. Materials and Methods
2.1. Chief Complaints
2.2. History of Present Illness
2.3. History of Past Illness
2.4. Personal and Family History
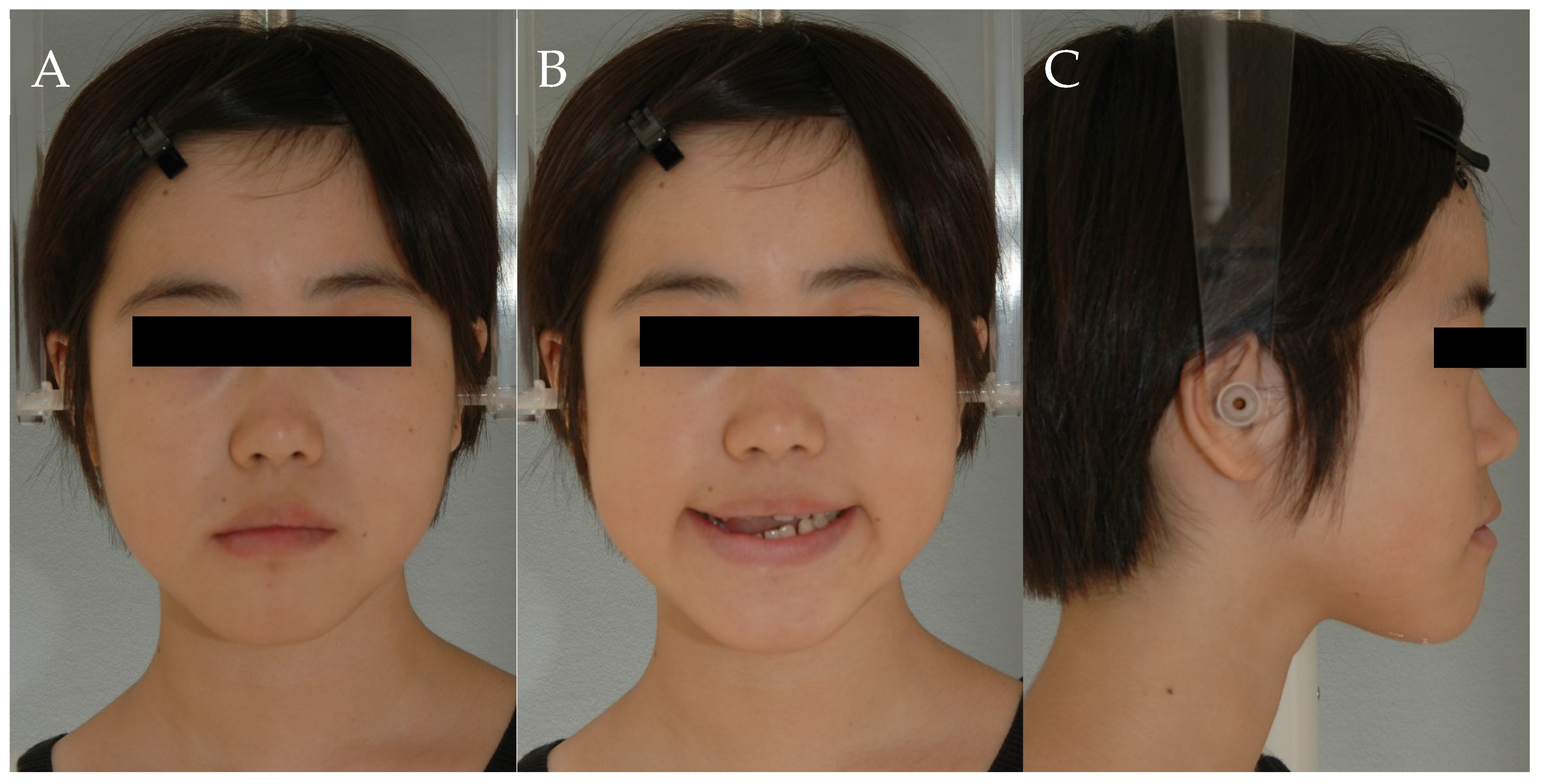
2.5. Clinical Examination
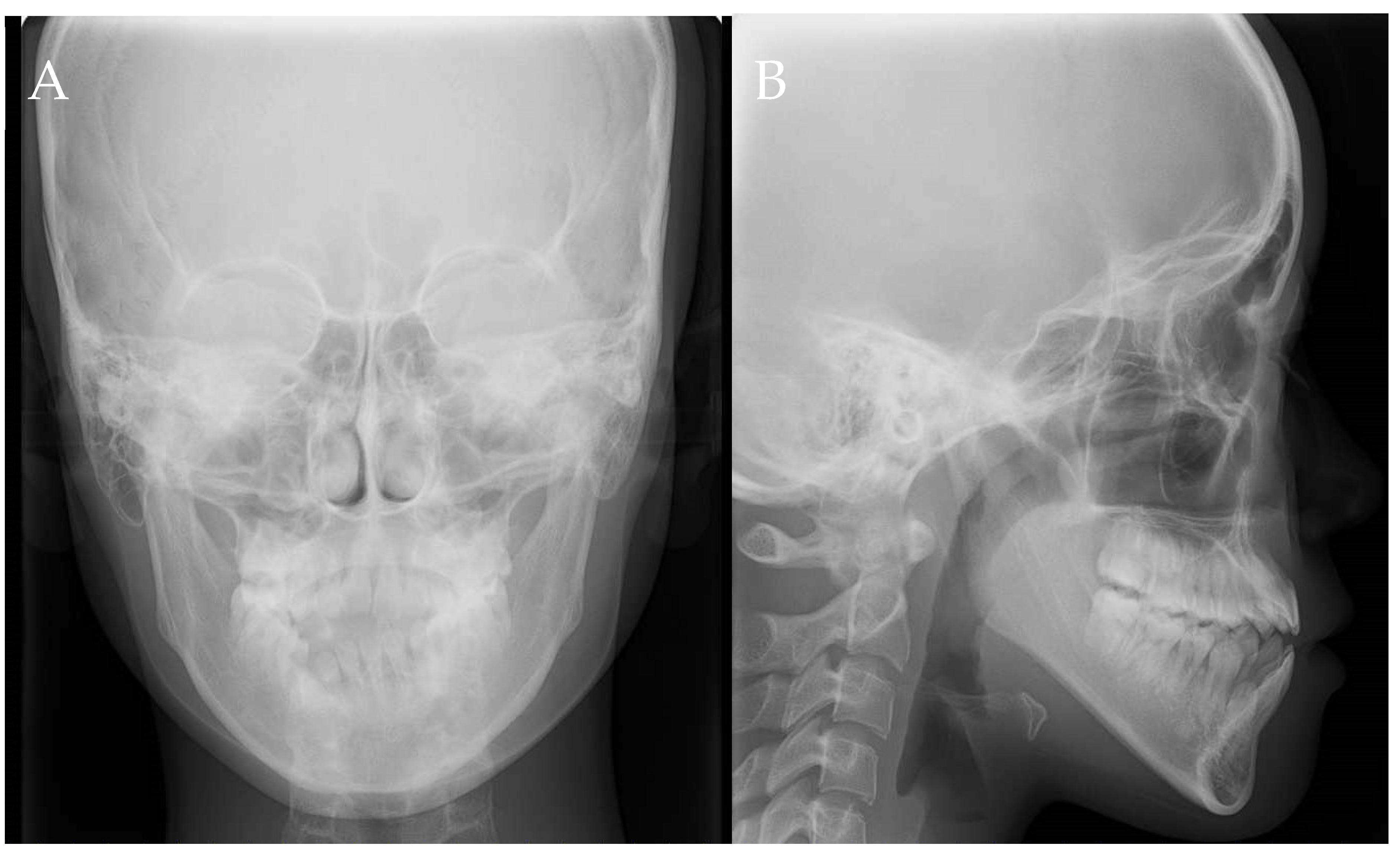
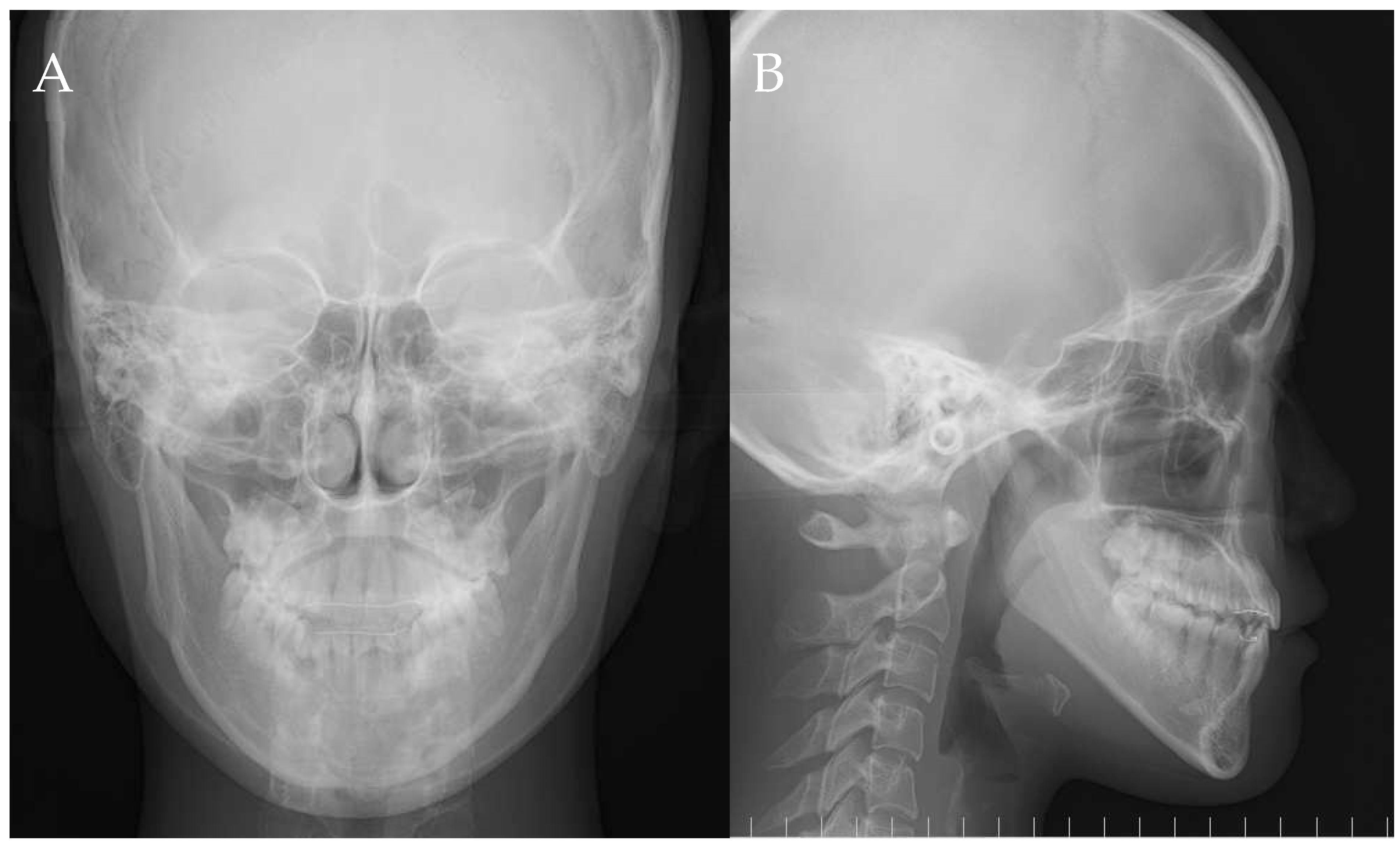
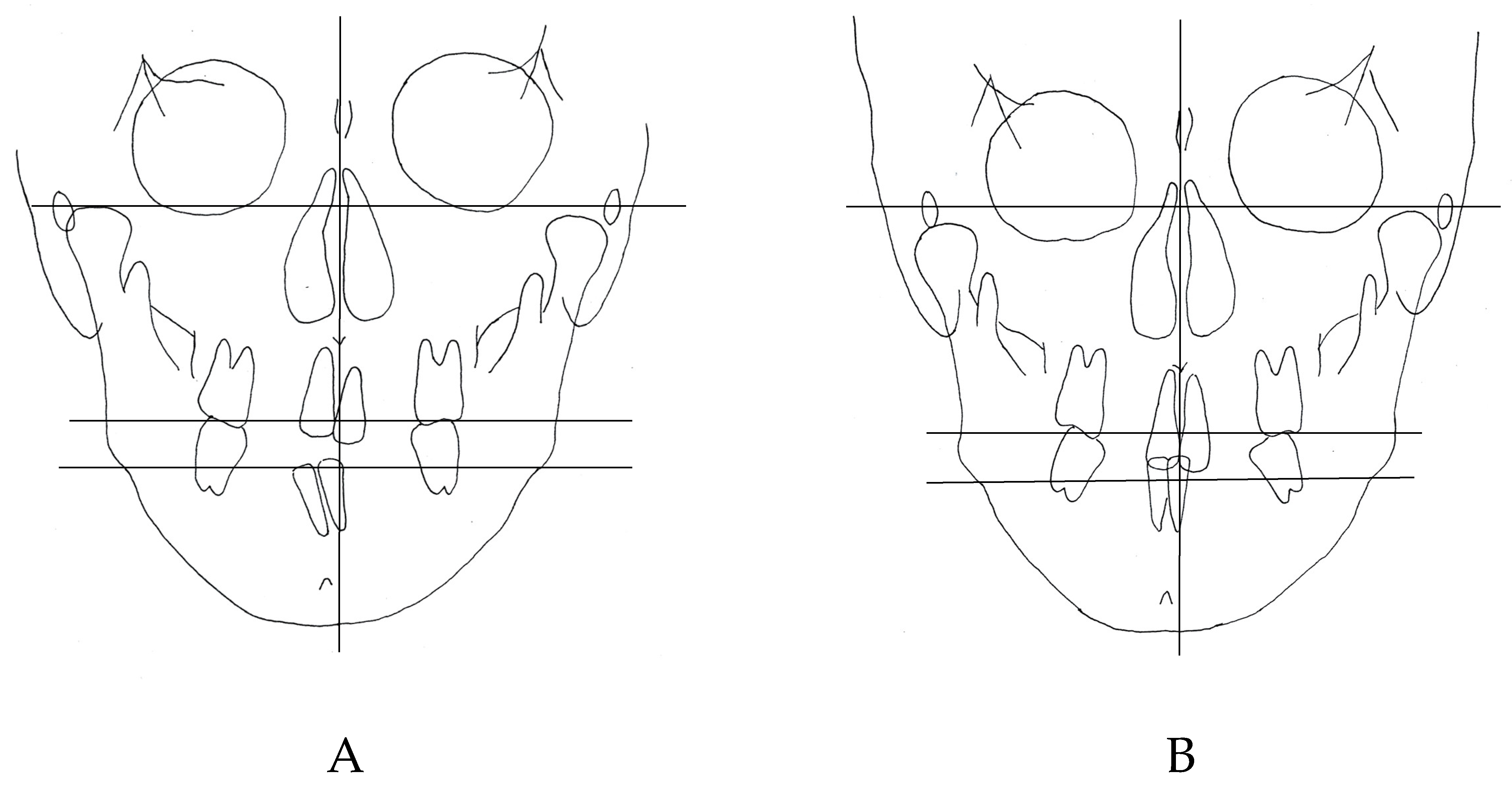
2.6. Imaging Examinations
2.7. Diagnosis
- Fixed rigid lingual arch devices were cemented on both the upper and lower jaws to assist with both anchorage and eruption of the ankylosed teeth.
- All teeth were moved orthodontically to diagnose the ankylosed teeth.
- Surgical luxation was performed on the ankylosed maxillary right central incisor, followed by orthodontic retraction using a nickel-titanium (NiTi) wire.
- The right mandibular lateral incisor and canine were luxated and retracted by intermaxillary elastics from a TAD that was inserted on the buccal alveolar bone between the right maxillary lateral incisor and canine.
2.8. Treatment Procedures
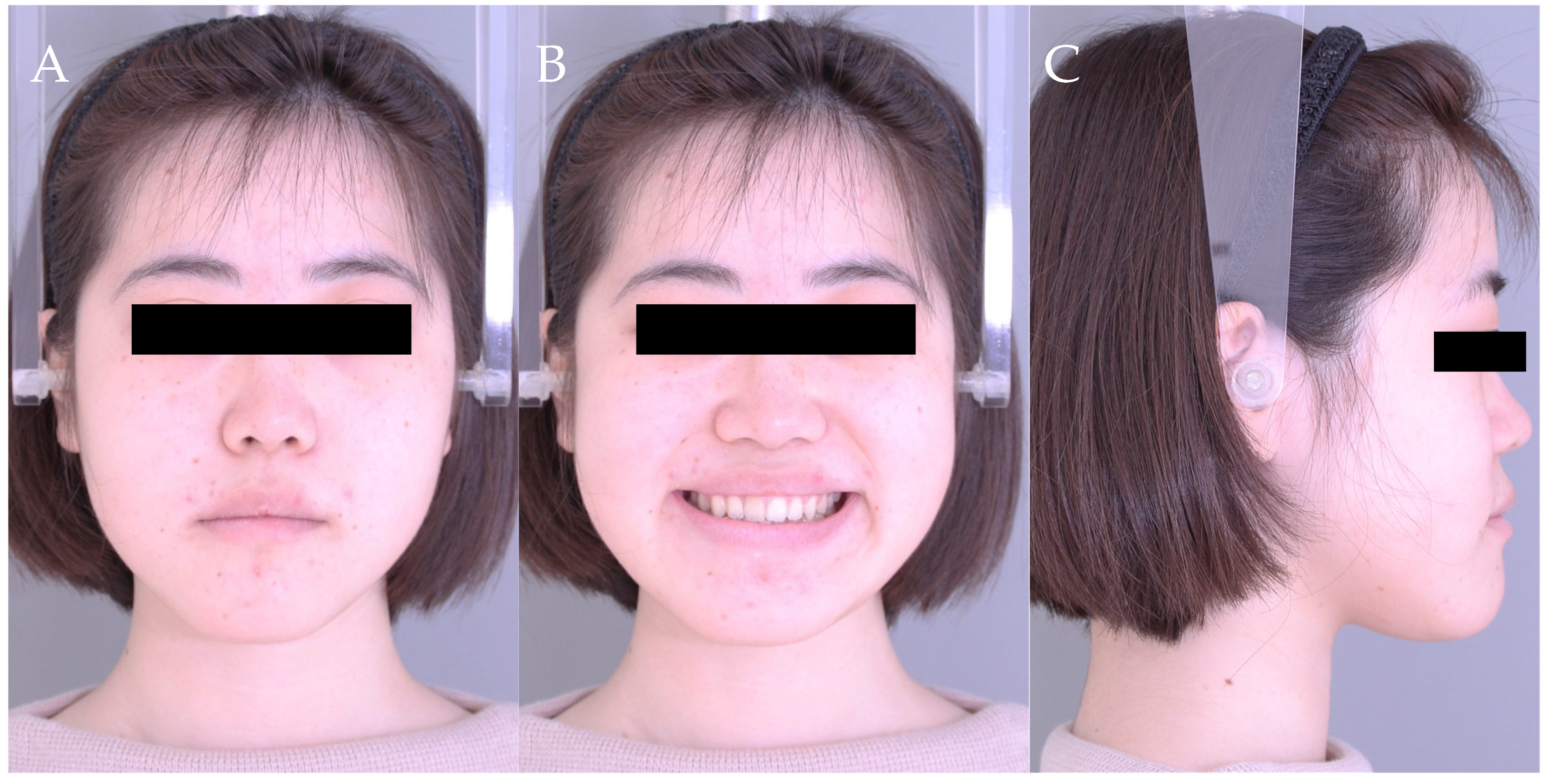
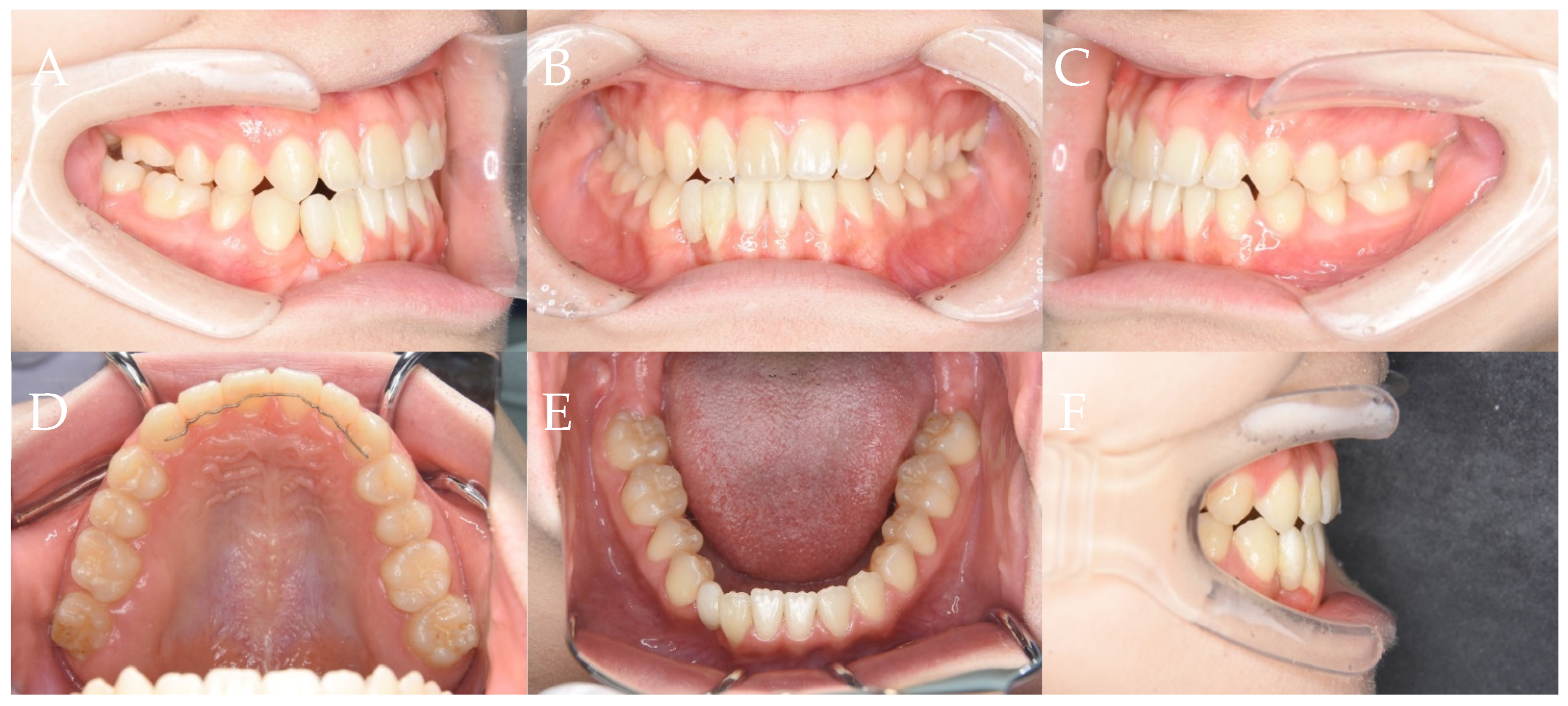
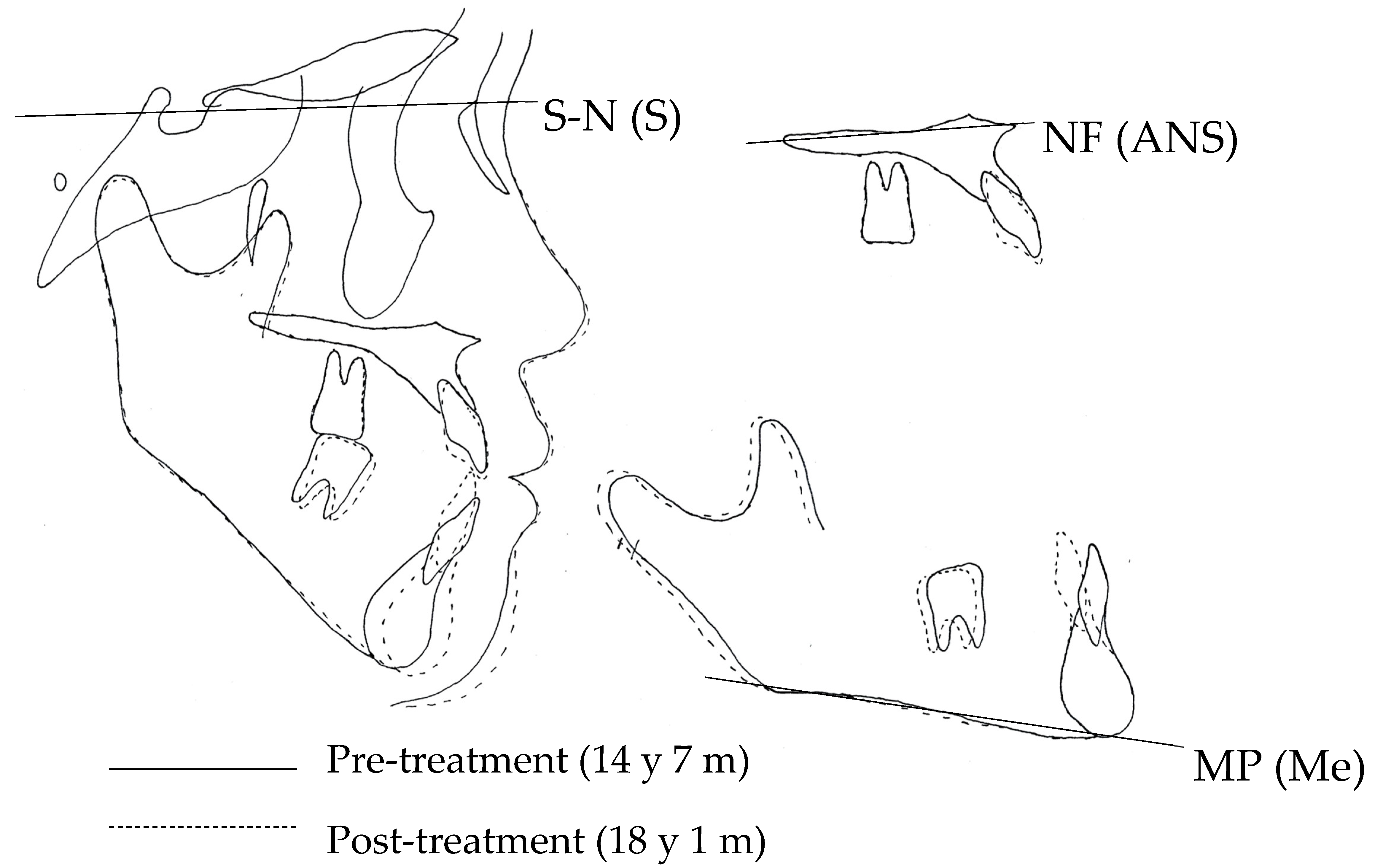
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grant, D.A.; Stern, I.B.; Listgarten, M.A. Periodontics in the Tradition of Gottlieb and Orban, 6th ed.; Mosby: St Louis, MO, USA, 1988; pp. 1215–1216. [Google Scholar]
- Alruwaithi, M.; Jumah, A.; Alsadoon, S.; Berri, Z.; Alsaif, M. Tooth ankylosis and its orthodontic implication. J. Dent. Med. Sci. 2017, 16, 108–112. [Google Scholar] [CrossRef]
- Thilander, B.; Myrberg, N. The prevalence of malocclusion in Swedish schoolchildren. Eur. J. Oral Sci. 1973, 81, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Biederman, W. The incidence and etiology of tooth ankyloses. Am. J. Orthod. 1956, 42, 921–926. [Google Scholar] [CrossRef]
- Dolanmaz, D.; Karaman, A.I.; Pampu, A.A.; Topkara, A. Orthodontic treatment of an ankylosed maxillary central incisor through osteogenic distraction. Angle Orthod. 2010, 80, 391–395. [Google Scholar] [CrossRef]
- Mitchell, D.L.; West, J.D. Attempted orthodontic movement in the presence of suspected ankylosis. Am. J. Orthod. 1975, 68, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L.; Blomlöf, L.; Lindskog, S.; Feiglin, B.; Hammarström, L. Tooth ankylosis. Clinical, radiographic and histological assessments. Int. J. Oral Surg. 1984, 13, 423–431. [Google Scholar] [CrossRef]
- Stenvik, A.; Beyer-Olsen, E.M.S.; Abyholm, F.; Haanaes, H.R.; Gerner, N.W. Validity of the radiographic assessment of ankylosis. Evaluation of long-termreactions in 10 monkeys. Acta Odontol. Scand. 1990, 48, 265–269. [Google Scholar] [CrossRef]
- Campbell, K.M.; Casas, M.J.; Kenny, D.J. Ankylosis of traumatized permanent incisors: Pathogenesis and current approaches to diagnosis and management. J. Can. Dent. Assoc. 2005, 71, 763–768. [Google Scholar]
- Bert, M.H.; Weinberger, T.; Schwarz, K.; Gruber, R.; Crismani, A.G. Resonance frequency analysis: A new diagnostic tool for dental ankylosis. Eur. J. Oral Sci. 2012, 20, 255–258. [Google Scholar] [CrossRef]
- Jacobs, S.G. Ankylosis of permanent teeth: A case report and literature review. Aust. Orthod. J. 1989, 11, 38–44. [Google Scholar]
- Takahashi, T.; Takagi, T.; Moriyama, K. Orthodontic treatment of a traumatically intruded tooth with ankylosis by traction after surgical luxation. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Biederman, W.; Chem, B. Etiology and treatment of tooth ankylosis. Am. J. Orthod. 1962, 48, 670–684. [Google Scholar] [CrossRef]
- Köle, H. Surgical operation on the alveolar ridge to correct occlusal abnormalities. Oral Surg. 1959, 12, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Bell, W.H. Surgical-orthodontic treatment of interincisal diastemas. Am. J. Orthod. 1970, 57, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Epker, B.N.; Paulus, P.J. Surgical-orthodontic correction of adult malocclusions: Single-tooth dento-osseous osteotomies. Am. J. Orthod. 1978, 74, 551–563. [Google Scholar] [CrossRef]
- Turley, P.K.; Jolner, M.W.; Hellstrom, S. The effect of orthodontic extrusion on traumatically intruded teeth. Am. J. Orthod. 1984, 85, 47–56. [Google Scholar] [CrossRef]
- Fukui, K.; Ogawa, H.; Ishihara, S.; Himuro, T. Approach to an ankylosed tooth using single-tooth dento-ooseous osteotomy. Orthod. Waves. 2005, 64, 38–44. [Google Scholar]
- Issacson, R.J.; Strauss, R.A.; Bridges-Poquis, A.; Peluso, A.R.; Lindauer, S.J. Moving an ankylosed central incisor using orthodontics, surgery and distraction osteogenesis. Angle Orhtod. 2001, 71, 411–418. [Google Scholar]
- Kinzinger, G.S.; Janicke, S.; Riediger, D.; Diedrich, P.R. Orthodontic fine adjusutment after vertical callus distraction of an ankylosed incisor using the floating bone concept. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 582–590. [Google Scholar] [CrossRef]
- Susami, T.; Matsuzaki, M.; Ogihara, Y.; Sakiyama, M.; Takato, T.; Sugawara, Y.; Matsumoto, S. Segmental alveolar distraction for the correction of unilateral open-bite caused by multiple ankylosed teeth: A case report. J. Orthod. 2006, 33, 153–159. [Google Scholar] [CrossRef]
- Chang, H.Y.; Chang, Y.L.; Chen, H.L. Treatment of a severely ankylosed central incisor and a missing lateral incisor by distraction osteogenesis and orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 829–838. [Google Scholar] [CrossRef]
- Kim, Y.; Park, S.; Son, W.; Kim, S.; Kim, Y.; Mah, J. Treatment of an ankylosis maxillary incisor by intraoral alveolar bone distraction osteogenesis. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 215–220. [Google Scholar] [CrossRef]
- Senisik, N.E.; Koqer, G.; Kaya, B.U. Ankylosed maxillary incisor with severe root resorption treated with a single-tooth dento-osseous osteotomy, vertical alveolar distraction osteogenesis and mini-implant anchorage. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 371–384. [Google Scholar] [CrossRef]
- You, K.H.; Min, Y.S.; Baik, H.S. Treatment of ankylosed maxillary central incisors by segmental osteotomy with autogenous bone graft. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 495–503. [Google Scholar] [CrossRef]
- Hwang, D.H.; Park, K.H.; Kwon, Y.D.; Kim, S.J. Treatment of Class II open bite complicated by an ankylosed maxillary central incisor. Angle Orthod. 2011, 81, 726–735. [Google Scholar] [CrossRef]
- Geiger, A.M.; Bronsky, M.J. Orthodontic management of ankylosed permanent posterior teeth: A clinical report of three cases. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 543–548. [Google Scholar] [CrossRef]
- Lim, W.H.; Kim, H.J.; Chun, Y.S. Treatment of ankylosed mandibular first permanent molar. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 95–101. [Google Scholar] [CrossRef]
- Pithon, M.M.; Bernardes, L.A. Treatment of ankylosis of the mandibular first molar with orthodontic traction immediately after surgical luxation. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 396–403. [Google Scholar] [CrossRef]
- Lin, F.; Sun, H.; Yao, L.; Chen, Q.; Ni, Z. Orthodontic treatment of severe anterior open bite and alveolar bone defect complicated by an ankylosed maxillary central incisor: A case report. Head Face Med. 2014, 10, 47. [Google Scholar] [CrossRef]
- Pithon, M.M. Surgical luxation and orthodontic traction of an ankylosed upper first molar. J. Clin. Orthod. 2016, 50, 299–306. [Google Scholar]
- Moon, C.H.; Lee, D.G.; Lee, H.S.; Im, J.S.; Baek, S.H. Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal region. Angle Orthod. 2008, 78, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Gandini, P.; Alcozer, R.; Vallittu, P.K.; Scribante, A. Failure load and stress analysis of orthodontic miniscrews with different transmucosal collar diameter. J. Mech. Behav. Biomed. Mater. 2018, 87, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Brugnolo, E.; Mazzocco, C.; Cordioll, G.; Majzoub, Z. Clinical and radiographic findings following placement of single-tooth implants in young patients-case reports. Int. J. Periodontics Restor. Dent. 1996, 16, 421–433. [Google Scholar]
- Pjetursson, B.E.; Tan, K.; Lang, N.P.; Brägger, U.; Egger, M.; Zwahlen, M. A systematic review of the survival and complication rates of implant supported fixed partial dentures (FPDs) after an observation period of at least 5 years. I. Implant-supported FPDs. Clin. Oral Implants Res. 2004, 15, 625–642. [Google Scholar] [CrossRef]
- Montasser, M.A.; Scribante, A. Root Injury During Interradicular Insertion is the most Common Complication Associated with Orthodontic Miniscrews. J. Evid. Based Dent. Pract. 2022, 22, 101688. [Google Scholar] [CrossRef]






| Tooth (FDI System) | 13 | 12 | 11 | 31 | 32 | 41 | 42 | 43 | 44 |
|---|---|---|---|---|---|---|---|---|---|
| Periotest value (PTV) | 8.0 | 17.5 | 1.7 | 19.9 | 20.0 | 17.6 | 4.5 | −1.7 | 5.1 |
| Measurements | Pre-Treatment | Post-Treatment |
|---|---|---|
| SNA (°) | 81.5 | 81.5 |
| SNB (°) | 81.3 | 82.8 |
| ANB (°) | 0.2 | −1.3 |
| FMA (°) | 36.2 | 36.5 |
| FMIA (°) | 64.3 | 74.6 |
| IMPA (°) | 79.5 | 68.9 |
| U1-SN (°) | 110.9 | 106.9 |
| U1 to A-Pog (mm) | 7.7 | 6.2 |
| L1 to B-Pog (mm) | 7.1 | 4.0 |
| E-line: Upper (mm) | 0.1 | −0.9 |
| E-line: Lower (mm) | 2.4 | 0.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yashima, Y.; Kaku, M.; Yamamoto, T.; Medina, C.C.; Ono, S.; Takeda, Y.; Tanimoto, K. Camouflage Correction of Skeletal Class III Severe Open Bite with Tooth Ankylosis Treated by Temporary Anchorage Devices: A Case Report. Dent. J. 2023, 11, 107. https://doi.org/10.3390/dj11040107
Yashima Y, Kaku M, Yamamoto T, Medina CC, Ono S, Takeda Y, Tanimoto K. Camouflage Correction of Skeletal Class III Severe Open Bite with Tooth Ankylosis Treated by Temporary Anchorage Devices: A Case Report. Dentistry Journal. 2023; 11(4):107. https://doi.org/10.3390/dj11040107
Chicago/Turabian StyleYashima, Yuka, Masato Kaku, Taeko Yamamoto, Cynthia Concepcion Medina, Shigehiro Ono, Yosuke Takeda, and Kotaro Tanimoto. 2023. "Camouflage Correction of Skeletal Class III Severe Open Bite with Tooth Ankylosis Treated by Temporary Anchorage Devices: A Case Report" Dentistry Journal 11, no. 4: 107. https://doi.org/10.3390/dj11040107
APA StyleYashima, Y., Kaku, M., Yamamoto, T., Medina, C. C., Ono, S., Takeda, Y., & Tanimoto, K. (2023). Camouflage Correction of Skeletal Class III Severe Open Bite with Tooth Ankylosis Treated by Temporary Anchorage Devices: A Case Report. Dentistry Journal, 11(4), 107. https://doi.org/10.3390/dj11040107






