Oral Secondary Syphilis in an HIV-Positive Transgender Patient: A Case Report and Review of the Literature
Abstract
:1. Introduction
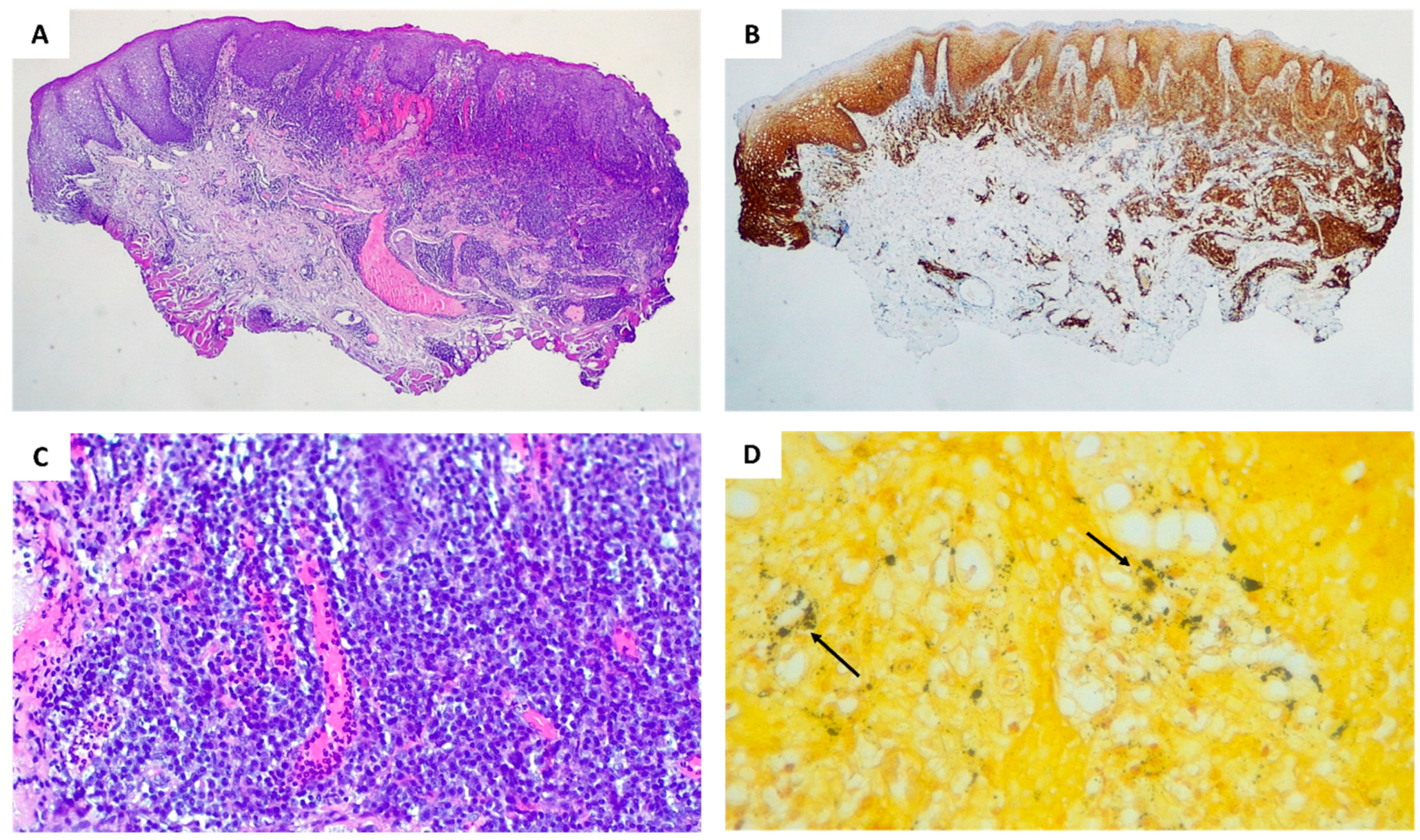
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stamm, L.V. Syphilis: Re-Emergence of an Old Foe. Microb. Cell 2016, 3, 363–370. [Google Scholar] [CrossRef]
- Shockman, S.; Buescher, L.S.; Stone, S.P. Syphilis in the United States. Clin. Dermatol. 2014, 32, 213–218. [Google Scholar] [CrossRef]
- Tsuboi, M.; Evans, J.; Davies, E.P.; Rowley, J.; Korenromp, E.L.; Clayton, T.; Taylor, M.M.; Mabey, D.; Chico, R.M. Prevalence of Syphilis among Men Who Have Sex with Men: A Global Systematic Review and Meta-Analysis from 2000–20. Lancet Glob. Health 2021, 9, e1110–e1118. [Google Scholar] [CrossRef]
- Ficarra, G.; Carlos, R. Syphilis: The Renaissance of an Old Disease with Oral Implications. Head Neck Pathol. 2009, 3, 195–206. [Google Scholar] [CrossRef]
- De Andrade, R.; de Freitas, E.; Rocha, B.; Gusmao, E.; Filho, M.; Junior, H. Oral Findings in Secondary Syphilis. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e138. [Google Scholar] [CrossRef]
- O’Byrne, P.; Orser, L.; MacPherson, P. Discussing Current Syphilis Case Definitions: A Proposal for a “Probable Infectious” Case. Public Health Nurs. 2021, 38, 390–395. [Google Scholar] [CrossRef]
- O’Byrne, P.; MacPherson, P. Syphilis. BMJ 2019, 365, l4159. [Google Scholar] [CrossRef]
- Peeling, R.W.; Mabey, D.; Kamb, M.L.; Chen, X.-S.; Radolf, J.D.; Benzaken, A.S. Syphilis. Nat. Rev. Dis. Primer 2017, 3, 17073. [Google Scholar] [CrossRef]
- Eijmael, M.; Bruin, R.D.; Hira, V.; Koster, T. A Peculiar Case of Syphilis Infection: The Great Imitator Is on the Rise. IDCases 2022, 28, e01521. [Google Scholar] [CrossRef]
- Peeling, R.W.; Hook, E.W. The Pathogenesis of Syphilis: The Great Mimicker, Revisited. J. Pathol. 2006, 208, 224–232. [Google Scholar] [CrossRef]
- Ramírez-Amador, V.; Castillejos-García, I.; Maldonado-Mendoza, J.; Saeb-Lima, M.; Aguilar-León, D.; Anaya-Saavedra, G. Exposing the Great Imitator: Proposal for a Holistic Diagnosis of Oral Secondary Syphilis in People Living with HIV. Head Neck Pathol. 2022, 16, 773–784. [Google Scholar] [CrossRef] [PubMed]
- Leuci, S.; Martina, S.; Adamo, D.; Ruoppo, E.; Santarelli, A.; Sorrentino, R.; Favia, G.; Mignogna, M. Oral Syphilis: A Retrospective Analysis of 12 Cases and a Review of the Literature. Oral Dis. 2013, 19, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.H.; Vargo, R.J.; Bilodeau, E.A.; Anderson, K.M.; Trzcinska, A.; Canterbury, C.R.; Fantasia, J.E.; Rawal, Y.B. Oral Manifestations of Syphilis: A Review of the Clinical and Histopathologic Characteristics of a Reemerging Entity with Report of 19 New Cases. Head Neck Pathol. 2021, 15, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chen, R.; Zhang, R. An Unusual Case of Secondary Syphilis Misdiagnosed as Allergic Dermatitis for 2 Years. Clin. Case Rep. 2020, 8, 2610–2612. [Google Scholar] [CrossRef] [PubMed]
- Roberts, C.P.; Klausner, J.D. Global Challenges in Human Immunodeficiency Virus and Syphilis Coinfection among Men Who Have Sex with Men. Expert Rev. Anti-Infect. Ther. 2016, 14, 1037–1046. [Google Scholar] [CrossRef]
- Lynn, W.; Lightman, S. Syphilis and HIV: A Dangerous Combination. Lancet Infect. Dis. 2004, 4, 456–466. [Google Scholar] [CrossRef]
- Zetola, N.M.; Klausner, J.D. Syphilis and HIV Infection: An Update. Clin. Infect. Dis. 2007, 44, 1222–1228. [Google Scholar] [CrossRef]
- Maartens, G.; Celum, C.; Lewin, S.R. HIV Infection: Epidemiology, Pathogenesis, Treatment, and Prevention. Lancet 2014, 384, 258–271. [Google Scholar] [CrossRef]
- Golden, M.R.; Marra, C.M.; Holmes, K.K. Update on Syphilis: Resurgence of an Old Problem. JAMA 2003, 290, 1510. [Google Scholar] [CrossRef]
- Singh, A.E.; Romanowski, B. Syphilis: Review with Emphasis on Clinical, Epidemiologic, and Some Biologic Features. Clin. Microbiol. Rev. 1999, 12, 187–209. [Google Scholar] [CrossRef]
- Thums, M.; Koth, V.; De Figueiredo, M.; Cherubini, K.; Salum, F. Oral Manifestations of Syphilis: An Epidemiological Study in Southern Brazil. Aust. Dent. J. 2021, 66, 289–294. [Google Scholar] [CrossRef] [PubMed]
- De Paulo, L.F.B.; Servato, J.P.S.; Oliveira, M.T.F.; Durighetto, A.F.; Zanetta-Barbosa, D. Oral Manifestations of Secondary Syphilis. Int. J. Infect. Dis. 2015, 35, 40–42. [Google Scholar] [CrossRef] [PubMed]
- Schuch, L.F.; Da Silva, K.D.; De Arruda, J.A.A.; Etges, A.; Gomes, A.P.N.; Mesquita, R.A.; Vasconcelos, A.C.U.; Tarquinio, S.B.C. Forty Cases of Acquired Oral Syphilis and a Review of the Literature. Int. J. Oral Maxillofac. Surg. 2019, 48, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, C.S.; Saturno, J.L.; De Sousa, S.C.O.M.; Da Silveira, F.R.X. Diagnostic Approaches in Unsuspected Oral Lesions of Syphilis. Int. J. Oral Maxillofac. Surg. 2014, 43, 1436–1440. [Google Scholar] [CrossRef]
- Cantisani, C.; Rega, F.; Ambrosio, L.; Grieco, T.; Kiss, N.; Meznerics, F.A.; Bánvölgyi, A.; Vespasiani, G.; Arienzo, F.; Rossi, G.; et al. Syphilis, the Great Imitator—Clinical and Dermoscopic Features of a Rare Presentation of Secondary Syphilis. Int. J. Environ. Res. Public Health 2023, 20, 1339. [Google Scholar] [CrossRef]
- Imad, H.A.; Lakanavisid, P.; Pisutsan, P.; Trerattanavong, K.; Ngamprasertchai, T.; Matsee, W.; Piyaphanee, W.; Leaungwutiwong, P.; Nguitragool, W.; Nakayama, E.E.; et al. A Case Report of Secondary Syphilis Co-Infected with Measles: A Diagnostic Dilemma with Fever and Rash. Trop. Med. Infect. Dis. 2022, 7, 70. [Google Scholar] [CrossRef]
- Corti, M.; Solari, R.; De Carolis, L.; Figueiras, O.; Vittar, N.; Maronna, E. Sífilis maligna en un paciente con infección por VIH: Presentación de un caso y revisión de la literatura. Rev. Chil. Infectol. 2012, 29, 678–681. [Google Scholar] [CrossRef]
- Compilato, D.; Amato, S.; Campisi, G. Resurgence of Syphilis: A Diagnosis Based on Unusual Oral Mucosa Lesions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 108, e45–e49. [Google Scholar] [CrossRef]
- Zhang, W.; Mao, Q.; Lyu, X.; Hua, H.; Yan, Z. Diagnosis of Oral Syphilis Remains a Challenge—A Case Report. Int. J. Infect. Dis. 2020, 99, 231–232. [Google Scholar] [CrossRef]
- De Andrade, B.A.B.; De Arruda, J.A.A.; Gilligan, G.; Piemonte, E.; Panico, R.; Molina Ávila, I.; Pimentel Sola, J.M.; Carmona Lorduy, M.C.; Pupo Marrugo, S.; Sánchez Tatis, A.S.; et al. Acquired Oral Syphilis: A Multicenter Study of 339 Patients from South America. Oral Dis. 2022, 28, 1561–1572. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mauceri, R.; Coppini, M.; Cascio, A.; Trizzino, M.; Crivello, V.; Florena, A.M.; Campisi, G. Oral Secondary Syphilis in an HIV-Positive Transgender Patient: A Case Report and Review of the Literature. Dent. J. 2023, 11, 231. https://doi.org/10.3390/dj11100231
Mauceri R, Coppini M, Cascio A, Trizzino M, Crivello V, Florena AM, Campisi G. Oral Secondary Syphilis in an HIV-Positive Transgender Patient: A Case Report and Review of the Literature. Dentistry Journal. 2023; 11(10):231. https://doi.org/10.3390/dj11100231
Chicago/Turabian StyleMauceri, Rodolfo, Martina Coppini, Antonio Cascio, Marcello Trizzino, Valentina Crivello, Ada Maria Florena, and Giuseppina Campisi. 2023. "Oral Secondary Syphilis in an HIV-Positive Transgender Patient: A Case Report and Review of the Literature" Dentistry Journal 11, no. 10: 231. https://doi.org/10.3390/dj11100231
APA StyleMauceri, R., Coppini, M., Cascio, A., Trizzino, M., Crivello, V., Florena, A. M., & Campisi, G. (2023). Oral Secondary Syphilis in an HIV-Positive Transgender Patient: A Case Report and Review of the Literature. Dentistry Journal, 11(10), 231. https://doi.org/10.3390/dj11100231








