Status of North American Graduate Programs in Periodontics Providing Laser Education and Clinical Training: A Cross-Sectional Survey
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Sample
2.3. Survey
2.4. Statistical Analysis
3. Results
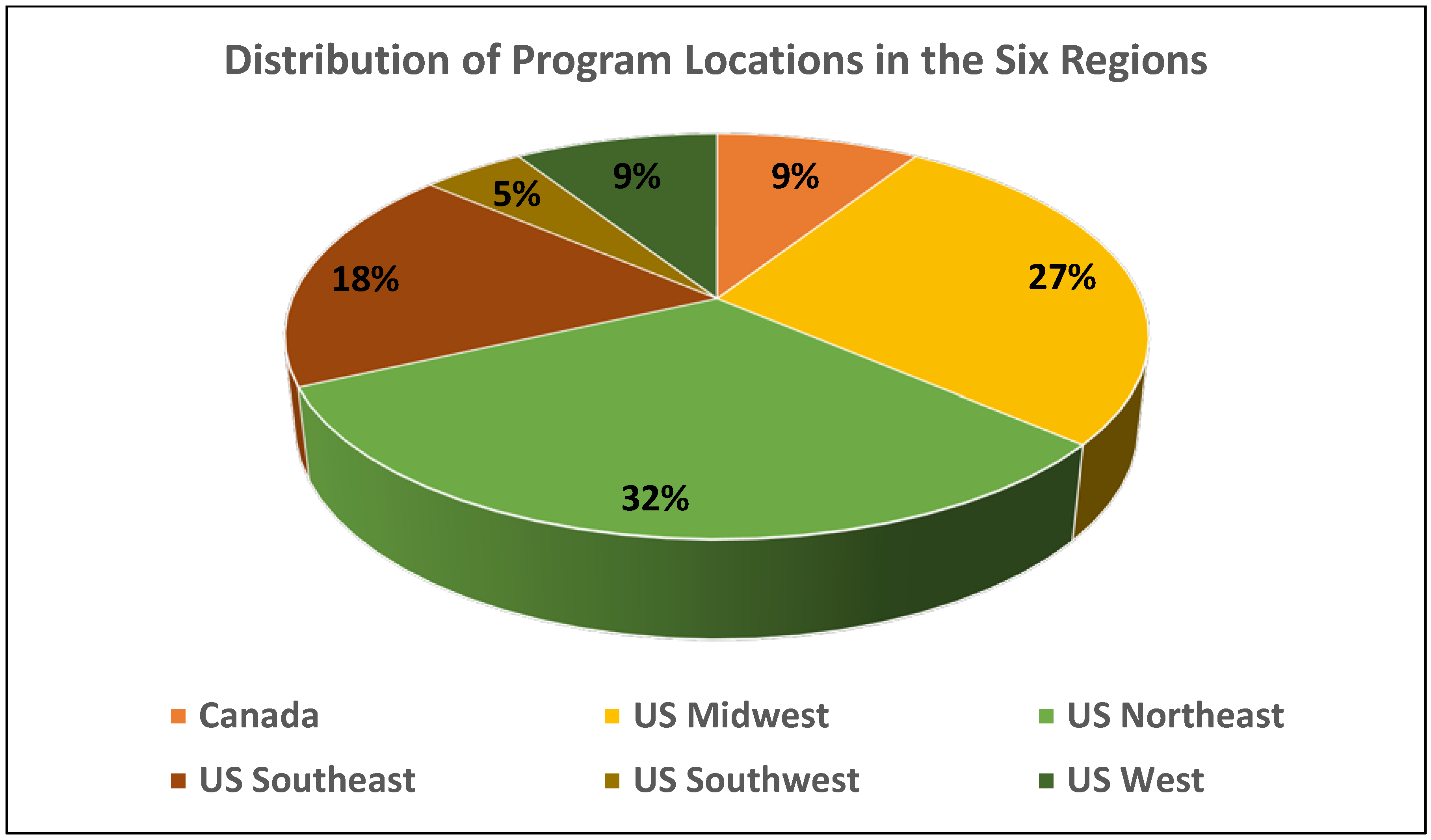
3.1. Periodontology Advanced Program Characteristics and Their Use of Lasers
3.2. Laser Education
3.3. Periodontology Program Directors’ Interest and Plans in Providing Laser Education
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Romanos, G. Current concepts in the use of lasers in periodontal and implant dentistry. J. Indian Soc. Periodontol. 2015, 19, 490–494. [Google Scholar] [CrossRef]
- Jassim, S.D. Laser Applications in Periodontology. In Public Health in Developing Countries—Challenges and Opportunities; Anugwom, E.E., Awofeso, N., Eds.; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef] [Green Version]
- Eberhard, J.; Ehlers, H.; Falk, W.; Açil, Y.; Albers, H.K.; Jepsen, S. Efficacy of subgingival calculus removal with Er:YAG laser compared to mechanical debridement: An in situ study. J. Clin. Periodontol. 2003, 30, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Ben Hatit, Y.; Blum, R.; Severin, C.; Maquin, M.; Jabro, M.H. The effects of a pulsed Nd:YAG laser on subgingival bacterial flora and on cementum: An in vivo study. J. Clin. Laser Med. Surg. 1996, 14, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Moritz, A.; Schoop, U.; Goharkhay, K.; Schauer, P.; Doertbudak, O.; Wernisch, J.; Sperr, W. Treatment of periodontal pockets with a diode laser. Lasers Surg. Med. 1998, 22, 302–311. [Google Scholar] [CrossRef]
- Yaneva, B.; Firkova, E.; Karaslavova, E.; Romanos, G.E. Bactericidal effects of using a fiber-less Er:YAG laser system for treatment of moderate chronic periodontitis: Preliminary results. Quintessence Int. 2014, 45, 489–497. [Google Scholar] [CrossRef]
- McCawley, T.K.; McCawley, M.N.; Rams, T.E. Immediate effect of Nd:YAG laser monotherapy on subgingival periodontal pathogens: A pilot clinical study. J. Periodontal Implant Sci. 2022, 52, 77–87. [Google Scholar] [CrossRef]
- Gold, S.I.; Vilardi, M.A. Pulsed laser beam effects on gingiva. J. Clin. Periodontol. 1994, 21, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E. Clinical applications of the Nd:YAG laser in oral soft tissue surgery and periodontology. J. Clin. Laser Med. Surg. 1994, 12, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Deppe, H.; Horch, H.H. Laser applications in oral surgery and implant dentistry. Lasers Med. Sci. 2007, 22, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Ting, M.; Alluri, L.S.C.; Sulewski, J.G.; Suzuki, J.B.; Paes Batista da Silva, A. Laser Treatment of Peri-Implantitis: A Systematic Review of Radiographic Outcomes. Dent. J. 2022, 10, 20. [Google Scholar] [CrossRef]
- Lin, G.H.; Suárez López Del Amo, F.; Wang, H.L. Laser therapy for treatment of peri-implant mucositis and peri-implantitis: An American Academy of Periodontology best evidence review. J. Periodontol. 2018, 89, 766–782. [Google Scholar] [CrossRef] [PubMed]
- Hamada, Y.; Ricker, A.; Chiou, L.L.; Prabhu, S.; Shin, D.E.; Blanchard, S.B. Dental laser training and education in postgraduate periodontics programs in North America. J. Dent. Educ. 2021, 86, 517–525. [Google Scholar] [CrossRef] [PubMed]
- Dansie, C.O.; Park, J.H.; Makin, I.R. Training and use of lasers in postgraduate orthodontic programs in the United States and Canada. J. Dent. Educ. 2013, 77, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Al-Jobair, A.M. Dental laser education and knowledge among final year dental students at King Saud University in Riyadh, Saudi Arabia. Saudi J. Dent. Res. 2014, 5, 98–103. [Google Scholar] [CrossRef] [Green Version]
- Yadav, S.; Chaudhry, S.; Talwar, S.; Verma, M. Knowledge and practices of dental lasers among dental professionals in India: A survey-based study. J. Dent. Lasers 2018, 12, 50–55. [Google Scholar] [CrossRef]
- Commission on Dental Accreditation. Accreditation Standards for Dental Education Programs. Standards for Predoctoral Dental Education. Chicago: American Dental Association. 2021. Available online: https://coda.ada.org/~/media/CODA/Files/predoc_standards.pdf?la=en (accessed on 8 June 2022).
- Brownstein, S.A.; Murad, A.; Hunt, R.J. Implementation of new technologies in U.S. dental school curricula. J. Dent. Educ. 2015, 79, 259–264. [Google Scholar] [CrossRef]
- Mehdipour, M.; Mortazavi, H.; Bahramian, A.; Haghighi Enayat, N.; Azari-Marhabi, S. The viewpoints of last-year dentistry students of Shahid Beheshti University on the application of lasers as an independent credit in the education of general dentistry. J. Lasers Med. Sci. 2020, 11, 193–196. [Google Scholar] [CrossRef] [Green Version]
- Ashnagar, S.; Nowzari, H.; Nokhbatolfoghahaei, H.; Yaghoub Zadeh, B.; Chiniforush, N.; Choukhachi Zadeh, N. Laser treatment of peri-implantitis: A literature review. J. Lasers Med. Sci. 2014, 5, 153–162. [Google Scholar]
- Yadwad, K.J.; Veena, H.R.; Patil, S.R.; Shivaprasad, B.M. Diode laser therapy in the management of chronic periodontitis—A clinico-microbiological study. Interv. Med. Appl. Sci. 2017, 9, 191–198. [Google Scholar] [CrossRef]
- Patil, P.; Kabbur, K.J.; Madaiah, H.; Satyanarayana, S. Diode laser frenectomy: A case report with review of literature. J. Dent. Lasers 2019, 13, 19–22. [Google Scholar] [CrossRef]
- Jha, A.; Gupta, V.; Adinarayan, R. LANAP, Periodontics and Beyond: A Review. J. Lasers Med. Sci. 2018, 9, 76–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crespi, R.; Cappare, P.; Gherlone, E.; Romanos, G.E. Comparison of modified widman and coronally advanced flap surgery combined with Co2 laser root irradiation in periodontal therapy: A 15-year follow-up. Int. J. Periodontics Restor. Dent. 2011, 31, 641–651. [Google Scholar]
- Zhao, Y.; Yin, Y.; Tao, L.; Nie, P.; Tang, Y.; Zhu, M. Er:YAG laser versus scaling and root planing as alternative or adjuvant for chronic periodontitis treatment: A systematic review. J. Clin. Periodontol. 2014, 41, 1069–1079. [Google Scholar] [CrossRef] [PubMed]
- Academy of Laser Dentistry, About the ALD Certification Programs. 2021. Available online: https://www.laserdentistry.org/certification (accessed on 3 May 2022).
- Waldron, R. Considering Laser Dentistry Certification? Here’s What You Should Know. 2/4/2019. Colgate. Available online: https://www.colgatetalks.com/laser-dentistry-certification/ (accessed on 3 May 2022).
- Convissar, R.A. Laser Dentistry in 2020: Technology Excels While Training Has Flaws. Compend. Contin. Educ. Dent. 2020, 41, 50–53. [Google Scholar] [PubMed]
- Mills, M.P.; Rosen, P.S.; Chambrone, L.; Greenwell, H.; Kao, R.T.; Klokkevold, P.R.; McAllister, B.S.; Reynolds, M.A.; Romanos, G.E.; Wang, H.L. American Academy of Periodontology best evidence consensus statement on the efficacy of laser therapy used alone or as an adjunct to non-surgical and surgical treatment of periodontitis and peri-implant diseases. J. Periodontol. 2018, 89, 737–742. [Google Scholar] [CrossRef] [Green Version]
- American Academy of Periodontology. 9/11/2018. American Academy of Periodontology Publishes Proceedings from Best Evidence Consensus Meeting on Lasers. Periodontal Experts Address Clinical Efficacy of Laser Usage in Patient Care. Available online: https://www.perio.org/press-release/american-academy-of-periodontology-publishes-proceedings-from-best-evidence-consensus-meeting-on-lasers/ (accessed on 3 May 2022).
- Commission on Dental Accreditation. Accreditation Standards for Dental Education Programs. Standards for Advanced Dental Education Programs. Periodontics. Chicago: American Dental Association. 2020. Available online: https://coda.ada.org/~/media/CODA/Files/perio.pdf?la=en (accessed on 8 June 2022).
| General Information | Number (%) |
|---|---|
| Number of residents in the graduate periodontics programs (n = 22): | |
| 1–3 | 1 (4.6) |
| 4–6 | 3 (13.6) |
| 7–12 | 14 (63.6) |
| Over 13 | 4 (18.2) |
| Lasers used in the periodontics graduate program (n = 22): | |
| Yes | 19 (86.4) |
| No | 3 (13.6) |
| Types of lasers used: * | |
| Diode | 17 (89.5) |
| NdYag | 10 (52.6) |
| Erbium | 7 (36.8) |
| CO2 | 7 (36.8) |
| Lasers used for: | |
| Clinical Treatment | 10 (52.6) |
| Clinical treatment and research | 9 (47.4) |
| Laser treatments provided by: | |
| Periodontics faculty | 1 (5.3) |
| Periodontics residents | 4 (21.1) |
| Both periodontics faculty and residents | 12 (63.2) |
| Periodontics faculty with resident assisting | 2 (10.5) |
| Types of Treatment Using Lasers | Number (%) |
|---|---|
| Periodontitis treatment | 11 (57.9) |
| Periimplantitis treatment | 16 (84.2) |
| Gingivectomy | 13 (68.4) |
| Frenectomy | 15 (78.9) |
| Canine exposure | 7 (36.8) |
| Crown lengthening | 5 (26.3) |
| Biopsies | 8 (42.1) |
| Biostimulation (intraoral) | 6 (31.6) |
| Biostimulation (extraoral) | 5 (26.3) |
| Implant uncovering | 4 (21.1) |
| Socket preservation | 1 (5.3) |
| Other: | |
| Coagulation; bone removal; Leukopl | 1 (5.3) |
| Laser Training Procedures | Number (%) |
|---|---|
| Type of Laser Training: | |
| Didactic only | 2 (9.1) |
| Clinical only | 2 (9.1) |
| Didactic and Clinical | 15 (68.2) |
| No laser training | 3 (13.6) |
| Is didactic course specific to laser training? | |
| Yes | 9 (60.0) |
| No | 6 (40.0) |
| Contact hours of didactic laser training: | |
| 1–3 h | 2 (13.3) |
| 4–6 h | 6 (40.0) |
| 7–12 h | 1 (6.7) |
| Over 12 h | 6 (40.0) |
| Number of clinical laser procedures (CLP) performed by residents during residency: | |
| 0 CLP | 1 (5.9) |
| 1–3 CLP | 3 (17.7) |
| 4–10 CLP | 9 (52.9) |
| 11–19 CLP | 2 (11.8) |
| Over 20 CLP | 2 (11.8) |
| Number of faculty members providing laser training in periodontics department: | |
| 1 Faculty member | 7 (63.6) |
| 2 Faculty members | 4 (36.4) |
| Laser Certification Protocol | Number (%) |
|---|---|
| Minimum number of clinical cases completed for certification: | |
| 1–4 clinical cases | 2 (40.0) |
| 5–9 clinical cases | 2 (40.0) |
| 10–15 clinical cases | 1 (20.0) |
| Certification given to: | |
| All residents receive certification | 4 (23.5) |
| Some residents receive certification based on certification program requirements | |
| Residents do not receive certification | 1 (5.9) |
| N/A | 9 (52.9) |
| 3 (17.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paes Batista da SIlva, A.; Irfan, U.M.; Furman, E.; Jasinevicius, T.R. Status of North American Graduate Programs in Periodontics Providing Laser Education and Clinical Training: A Cross-Sectional Survey. Dent. J. 2022, 10, 119. https://doi.org/10.3390/dj10070119
Paes Batista da SIlva A, Irfan UM, Furman E, Jasinevicius TR. Status of North American Graduate Programs in Periodontics Providing Laser Education and Clinical Training: A Cross-Sectional Survey. Dentistry Journal. 2022; 10(7):119. https://doi.org/10.3390/dj10070119
Chicago/Turabian StylePaes Batista da SIlva, Andre, Uma M. Irfan, Elena Furman, and T. Roma Jasinevicius. 2022. "Status of North American Graduate Programs in Periodontics Providing Laser Education and Clinical Training: A Cross-Sectional Survey" Dentistry Journal 10, no. 7: 119. https://doi.org/10.3390/dj10070119
APA StylePaes Batista da SIlva, A., Irfan, U. M., Furman, E., & Jasinevicius, T. R. (2022). Status of North American Graduate Programs in Periodontics Providing Laser Education and Clinical Training: A Cross-Sectional Survey. Dentistry Journal, 10(7), 119. https://doi.org/10.3390/dj10070119





