Burning Mouth Syndrome (BMS)—Treatment with Verbal and Written Information, B Vitamins, Probiotics, and Low-Level Laser Therapy: A Randomized Clinical Trial
Abstract
:1. Introduction
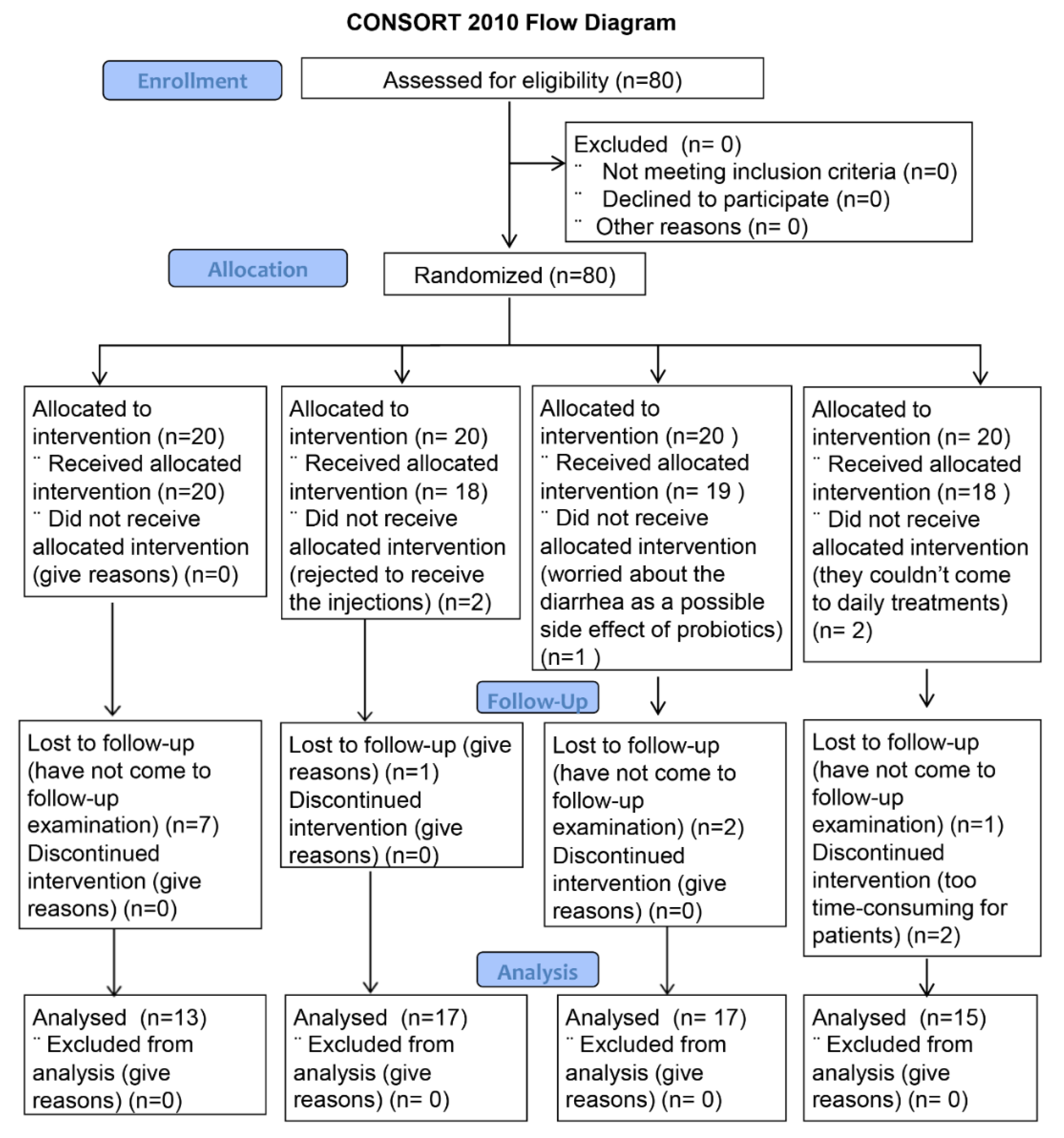
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Study Setting
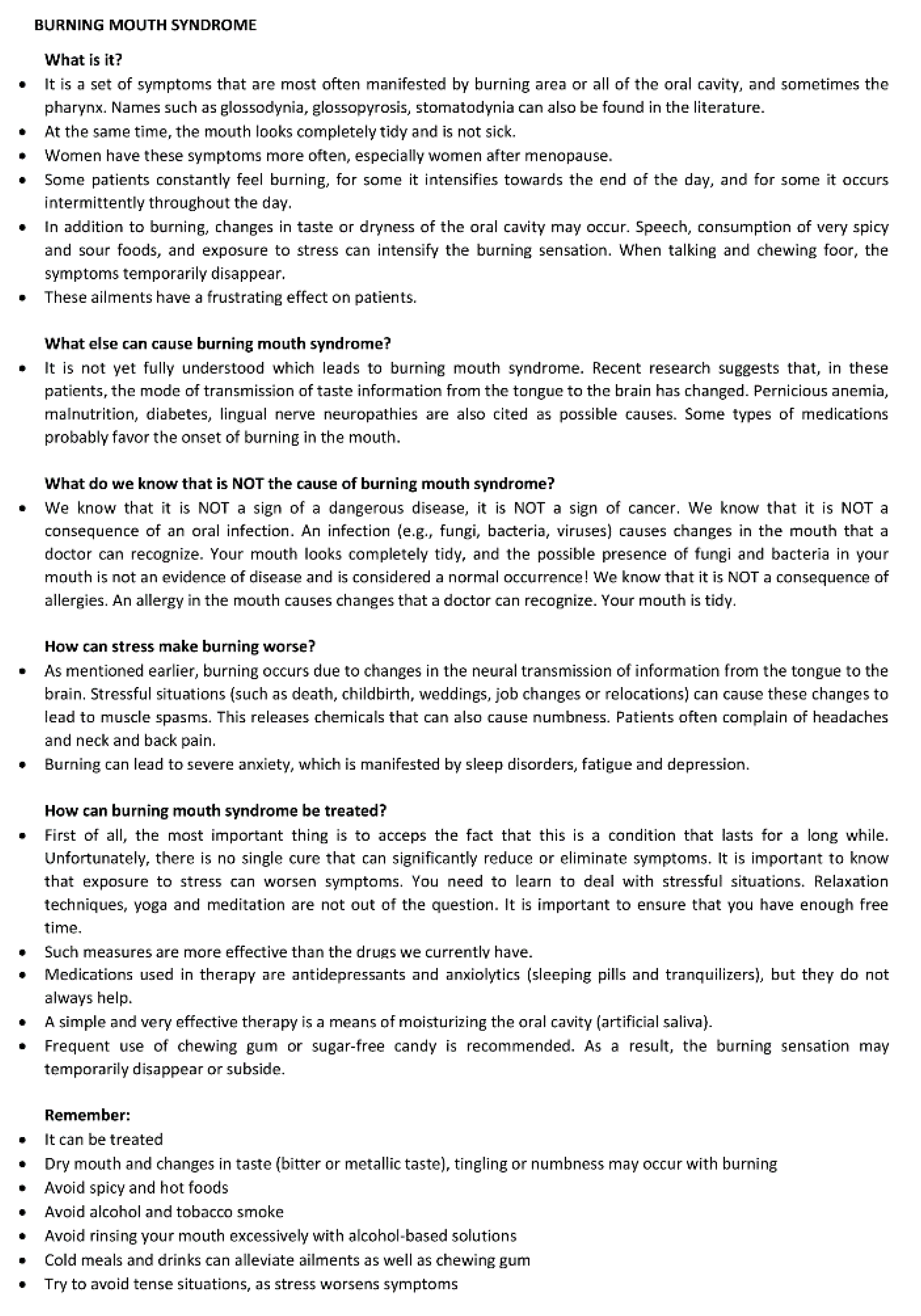
2.3. Interventions
2.4. Primary Outcome Measure
2.5. Secondary Outcome Measures
2.6. Sample Size Determination
2.7. Allocation
2.8. Blinding
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Andabak Rogulj, A.; Lončar Brzak, B.; Vučićević Boras, V.; Vidović Juras, D.; Škrinjar, I. Burning mouth syndrome–A burning enigma. Med. Flum. 2021, 57, 4–16. [Google Scholar] [CrossRef]
- Scala, A.; Checchi, L.; Montevecchi, M.; Marini, I. Update on burning mouth syndrome: Overview and patient management. Crit. Rev. Oral Biol. Med. 2003, 14, 275–291. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Jornet, M.P.; Camacho-Alonso, F.; Andujar-Mateos, P.; SánchezSiles, M.; Gómez-Garcia, F. Burning mouth syndrome: An update. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e562–e568. [Google Scholar] [CrossRef] [PubMed]
- Grushka, M.; Epstein, J.B.; Gorsky, M. Burning mouth syndrome. Am. Fam. Physician 2002, 65, 615–620. [Google Scholar] [PubMed]
- Jäaskeläinen, S.K.; Woda, A. Burning mouth syndrome. Cephalalgia 2017, 37, 627–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zakrzewska, J.; Buchanan, J.A. Burning mouth syndrome. BMJ Clin. Evid. 2016, 2016, 1301. [Google Scholar] [PubMed]
- Matsuoka, H.; Himachi, M.; Furukawa, H.; Kobayashi, S.; Shoki, H.; Motoya, R. Cognitive profile of patients with burning mouth syndrome in Japanese population. Odontology 2010, 98, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Rogulj, A.A.; Richter, I.; Brailo, V.; Krstevski, I.; Boras, V.V. Catastrophizing in patients with burning mouth syndrome. Acta Stomatol. Croat. 2014, 48, 109–115. [Google Scholar] [PubMed]
- McMillan, R.; Forssell, H.; Buchanan, J.A.G.; Glenny, A.M.; Weldon, J.C.; Zakrzewska, J.M. Interventions for treating burning mouth syndrome. Cochrane Database Syst. Rev. 2016, 11, CD002779. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.F.; Kim, Y.; Yoo, T.; Han, P.; Inman, J.C. Burning Mouth Syndrome: A Systematic Review of Treatments. Oral Dis. 2018, 24, 325–334. [Google Scholar] [CrossRef]
- Škrinjar, I.; Lončar Brzak, B.; Vidranski, V.; Vučičević Boras, V.; Andabak Rogulj, A.; Pavelić, B. Salivary Cortisol Levels and Burning Symptoms in Patients with Burning Mouth Syndrome Before and After Low Level Laser Therapy: A Double Blind Controlled Randomized Clinical Trial. Acta Stomatol. Croat. 2020, 54, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Pelivan, I.; Vucicevic Boras, V.; Skrinjar, I.; Loncar Brzak, B. Vitamin B1, B6 and B12 injections relieve symptoms of burning mouth syndrome. Australas. Med. J. 2018, 11, 253–254. [Google Scholar]
- De Pedro, M.; López-Pintor, R.M.; Casañas, E.; Hernández, G. Effects of photobiomodulation with low-level laser therapy in burning mouth syndrome: A randomized clinical trial. Oral Dis. 2020, 26, 1764–1776. [Google Scholar] [CrossRef] [PubMed]
- Spanemberg, J.C.; Segura-Egea, J.J.; Rodríguez-de Rivera-Campillo, E.; Jané-Salas, E.; Salum, F.G.; López-López, J. Low-level laser therapy in patients with Burning Mouth Syndrome: A double-blind, randomized, controlled clinical trial. J. Clin. Exp. Dent. 2019, 11, e162–e169. [Google Scholar] [CrossRef] [PubMed]
- Al-Maweri, S.A.; Javed, F.; Kalakonda, B.; AlAizari, N.A.; Al-Soneidar, W.; Al-Akwa, A. Efficacy of low level laser therapy in the treatment of burning mouth syndrome: A systematic review. Photodiagn. Photodyn. Ther. 2017, 17, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Moore, K. Lasers and pain treatment. Laser Part Clinix 2004, 72, 1–6. [Google Scholar]
- Morr Verenzuela, C.S.; Davis, M.D.P.; Bruce, A.J.; Torgerson, R.R. Burning mouth syndrome: Results of screening tests for vitamin and mineral deficiencies, thyroid hormone, and glucose levels-experience at Mayo Clinic over a decade. Int. J. Dermatol. 2017, 56, 952–956. [Google Scholar] [CrossRef] [PubMed]
- Calderón-Ospina, C.A.; Nava-Mesa, M.O. B Vitamins in the nervous system: Current knowledge of the biochemical modes of action and synergies of thiamine, pyridoxine, and cobalamin. CNS Neurosci. Ther. 2020, 26, 5–13. [Google Scholar] [CrossRef] [Green Version]
- Stein, J.; Geisel, J.; Obeid, R. Association between neuropathy and B-vitamins: A systematic review and meta-analysis. Eur. J. Neurol. 2021, 28, 2054–2064. [Google Scholar] [CrossRef]
- Klasser, G.D.; Grushka, M.; Su, N. Burning Mouth Syndrome. Oral Maxillofac. Surg. Clin. N. Am. 2016, 28, 381–396. [Google Scholar]
- Vivekananda, M.R.; Vandana, K.L.; Bhat, K.G. Effect of the probiotic Lactobacilli reuteri (Prodentis) in the management of periodontal disease: A preliminary randomized clinical trial. J. Oral Microbiol. 2010, 2, 5344. [Google Scholar] [CrossRef] [PubMed]
- Galofré, M.; Palao, D.; Vicario, M.; Nart, J.; Violant, D. Clinical and Microbiological Evaluation of the Effect of Lactobacillus Reuteri in the Treatment of Mucositis and Peri-Implantitis: A TripleBlind Randomized Clinical Trial. J. Periodontal Res. 2018, 53, 378–390. [Google Scholar] [CrossRef] [PubMed]
- İnce, G.; Gürsoy, H.; İpçi, S.D.; Cakar, G.; Ebru Emekli-Alturfan, E.; Yılmaz, S. Clinical and Biochemical Evaluation of Lozenges Containing Lactobacillus Reuteri as an Adjunct to NonSurgical Periodontal Therapy in Chronic Periodontitis. J. Periodontol. 2015, 86, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Żółkiewicz, J.; Marzec, A.; Ruszczyński, M.; Feleszko, W. Postbiotics—A Step Beyond Pre- and Probiotics. Nutrients 2020, 12, 2189. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, K.H.; Bueno, M.R.; Kawamoto, D.; Simionato, M.R.L.; Mayer, M.P.A. Lactobacilli postbiotics reduce biofilm formation and alter transcription of virulence genes of Aggregatibacter actinomycetemcomitans. Mol. Oral Microbiol. 2021, 36, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Butera, A.; Gallo, S.; Pascadopoli, M.; Taccardi, D.; Scribante, A. Home Oral Care of Periodontal Patients Using Antimicrobial Gel with Postbiotics, Lactoferrin, and Aloe Barbadensis Leaf Juice Powder vs. Conventional Chlorhexidine Gel: A Split-Mouth Randomized Clinical Trial. Antibiotics 2022, 11, 118. [Google Scholar] [CrossRef] [PubMed]
- Grushka, M.; Epstein, J.B.; Gorsky, M. Burning mouth syndrome: Differential diagnosis. Dermatol. Ther. 2002, 15, 287–291. [Google Scholar] [CrossRef]
- Grushka, M.; Bartoshuk, L. Burning mouth syndrome and oral dysesthesias. Can. J. Diagn. 2000, 17, 99–109. [Google Scholar]
- Nasri-Heir, C.; Gomes, J.; Heir, G.M.; Ananthan, S.; Benoliel, R.; Teich, S. The role of sensory input of the chorda tympani nerve and the number of fungiform papillae in burning mouth syndrome. Oral Surg. Oral. Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Petričević, N.; Ćelebić, A.; Papić, M.; Rener-Sitar, K. The Croatian version of the Oral Health Impact Profile Questionnaire. Coll. Antropol. 2009, 33, 841–847. [Google Scholar]
- Marino, R.; Torretta, S.; Capaccio, P.; Pignataro, L.; Spadari, F. Different therapeutic strategies for burning mouth syndrome: Preliminary data. J. Oral Pathol. Med. 2010, 39, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Ettlin, D.A. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorder, 3rd edition (beta version). Cephalalgia 2013, 33, 629–808. [Google Scholar]
- Zakrzewska, J.M.; Forssell, H.; Glenny, A.M. Interventions for the treatment of burning mouth syndrome. Cochrane Database Syst. Rev. 2005, 1, CD002779. [Google Scholar] [CrossRef]
- Henriques, A.C.; Maia, A.M.; Cimões, R.; Castro, J.F. The laser therapy in Dentistry: Properties, indications and current aspects. Odontol. Clín. Científ. 2008, 7, 197–200. [Google Scholar]
- Kuhn, A.; Porto, F.A.; Miraglia, P.; Brunetto, A.L. Low-level infrared laser therapy in chemotherapy-induced oral mucositis: A randomized placebo-controlled trial in children. J. Pediatr. Hematol. Oncol. 2009, 31, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Scardina, G.A.; Casella, S.; Bilello, G.; Messina, P. Photobiomodulation Therapy in the Management of Burning Mouth Syndrome: Morphological Variations in the Capillary Bed. Dent. J. 2020, 8, 99. [Google Scholar] [CrossRef] [PubMed]
- Spanemberg, J.C.; Figueiredo, M.A.; Cherubini, K.; Salum, F.G. Low-level Laser Therapy: A Review of Its Applications in the Management of Oral Mucosal Disorders. Altern. Ther. Health Med. 2016, 22, 24–31. [Google Scholar]
- Bardellini, E.; Amadori, F.; Conti, G.; Majorana, A. Efficacy of the photobiomodulation therapy in the treatment of the burning mouth syndrome. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e787–e791. [Google Scholar] [CrossRef] [PubMed]
- Sikora, M.; Včev, A.; Siber, S.; Vučićević Boras, V.; Rotim, Ž.; Matijević, M. The Efficacy of Low-Level Laser Therapy in Burning Mouth Syndrome–A Pilot Study. Acta Clin. Croat. 2018, 57, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Grushka, M.; Sessle, B. Taste dysfunction in burning mouth syndrome. Gerodontics 1988, 4, 256–258. [Google Scholar] [CrossRef]
- Kveton, J.F.; Bartoshuk, L.M. The effect of unilateral chorda tympani damage on taste. Laryngoscope 1994, 104, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Halpern, B.P.; Nelson, L.M. Bulbar gustatory responses to anteriorand posterior tongue stimulation in the rat. Am. J. Physiol. 1965, 209, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, K.; Bartoshuk, L.M.; Catalanotto, F.A.; Karrer, T.A.; Kveton, J.F. Anesthesia of the chorda tympani nerve and tastephantoms. Physiol. Behav. 1998, 63, 329–335. [Google Scholar] [CrossRef]
- Formaker, B.K.; Frank, M.E. Taste function in patients with oral burning. Chem. Senses 2000, 25, 575–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stough, C.; Scholey, A.; Lloyd, J.; Spong, J.; Myers, S.; Downey, L.A. The effect of 90 day administration of a high dose vitamin B-complex on work stress. Hum. Psychopharmacol. 2011, 26, 470–476. [Google Scholar] [CrossRef] [PubMed]
- White, D.J.; Cox, K.H.; Peters, R.; Pipingas, A.; Scholey, A.B. Effects of four-week supplementation with a multi-vitamin/mineral preparation on mood and blood biomarkers in young adults: A randomised, double-blind, placebo-controlled trial. Nutrients 2015, 7, 9005–9017. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ford, T.C.; Downey, L.A.; Simpson, T.; McPhee, G.; Oliver, C.; Stough, C. The Effect of a High-Dose Vitamin B Multivitamin Supplement on the Relationship between Brain Metabolism and Blood Biomarkers of Oxidative Stress: A Randomized Control Trial. Nutrients 2018, 10, 1860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarado, A.M.; Navarro, S.A. Complex B vitamins: Physiology and Therapeutic Effect on Pain. Am. J. Pharmacol. Sci. 2016, 4, 20–27. [Google Scholar]
- Lamey, P.J.; Hammond, A.; Allam, B.F.; McIntosh, W.B. Vitamin status of patients with burning mouth syndrome and the response to replacement therapy. Br. Dent. J. 1986, 160, 81–84. [Google Scholar] [CrossRef] [PubMed]
| Type of the Treatment | Informative Conversation and Translated and Adapted Leaflet (Facial Pain Team Based at the Royal National ENT and Eastman Dental Hospitals) | Neurobion Injections (100 mg of Vitamin B1 and B6 and 1 mg of Vitamin B12) | Oral Probiotics (BioGaiaProdentis, BioGaia AB, Stockholm, Sweden) One Lozenge Contains the Patented Lactic Acid Bacterium Lactobacillus reuteri Pro-Dentis® (L. reuteri DSM 17938 and L. reuteri ATCC PTA 5289) | LLLT (Aluminium Gallium Arsenide Laser; Ga–Al–As Diode Type of Laser) |
|---|---|---|---|---|
| Application mode | At the first appointment. | Total of nine vitamin B injections every other day into the gluteal muscle (i.m.), for three weeks, excluding weekends. | One lozenge to melt in the mouth every evening after flossing and toothbrushing for one month. | Applied on three reported burning sites, with a total of 10 treatments once a day for 10 consecutive days, excluding weekends. |
| Parameter | Value |
|---|---|
| Wavelength (nm) | 685 |
| Dose (J/cm2) | 2.0 |
| Power (mW) | 30 |
| Power density (W/cm2) | 0.003 |
| Single treatment duration (s) | 381 |
| Distance (cm) | 0.5 |
| Treated surface area (cm2) | 3 |
| Frequency (Hz) | 50 |
| Cumulative dose (J/cm2) | 60 |
| Number of treatments | 10 |
| Treatment | Age (Median, Range) (Years) | Sex (F = Female, M = Male) |
|---|---|---|
| Informative | 55 (38–83) | 10 F, 3 M |
| B vitamins | 62 (39–60) | 13 F, 4 M |
| Oral probiotics | 67 (43–84) | 13 F, 4 M |
| LLLT | 60 (44–83) | 11 F, 4 M |
| p | >0.05 | >0.05 |
| Intergroup Comparison (OHIP) | z-Score | p-Value |
|---|---|---|
| Informative: B vitamins | −0.23 | 0.409 |
| Informative: probiotics | 0.502 | 0.617 |
| Informative: LLLT | −0.102 | 0.92 |
| B vitamins: probiotics | −1.016 | 0.307 |
| B vitamins: LLLT | −0.669 | 0.502 |
| Probiotics: LLLT | 0.314 | 0.756 |
| Intergroup Comparison (VAS) | z-Score | p-Value |
|---|---|---|
| Informative: B vitamins | 0.146 | 0.88 |
| Informative: probiotics | 0.921 | 0.357 |
| Informative: LLLT | 0 | 1 |
| B vitamins: probiotics | −0.499 | 0.617 |
| B vitamins: LLLT | 0.460 | 0.645 |
| Probiotics: LLLT | 1.001 | 0.317 |
| Informative | B Vitamins | Oral Probiotics | LLLT | |
|---|---|---|---|---|
| OHIP-1, median (range) | 13 (3–24) | 24 (0–48) | 22 (2–50) | 20 (4–35) |
| OHIP-2, median (range) | 11 (0–24) | 16 (0–51) | 12 (0–46) | 14 (2–31) |
| N | 13 | 17 | 17 | 15 |
| p | 0.12 | 0.42 | 0.003 | 0.006 |
| Standardized effect size | 0.45 | 0.17 | 0.62 | 0.58 |
| Informative | B Vitamins | Oral Probiotics | LLLT | |
|---|---|---|---|---|
| VAS-1, median (range) | 5 (3–7) | 7 (3–10) | 6 (2–10) | 6 (4–9) |
| VAS-2, median (range) | 3 (0–6.5) | 4 (0–10) | 5 (0–7) | 5 (3–7) |
| N | 13 | 17 | 17 | 15 |
| P | 0.001 | 0.003 | 0.004 | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lončar-Brzak, B.; Škrinjar, I.; Brailo, V.; Vidović-Juras, D.; Šumilin, L.; Andabak-Rogulj, A. Burning Mouth Syndrome (BMS)—Treatment with Verbal and Written Information, B Vitamins, Probiotics, and Low-Level Laser Therapy: A Randomized Clinical Trial. Dent. J. 2022, 10, 44. https://doi.org/10.3390/dj10030044
Lončar-Brzak B, Škrinjar I, Brailo V, Vidović-Juras D, Šumilin L, Andabak-Rogulj A. Burning Mouth Syndrome (BMS)—Treatment with Verbal and Written Information, B Vitamins, Probiotics, and Low-Level Laser Therapy: A Randomized Clinical Trial. Dentistry Journal. 2022; 10(3):44. https://doi.org/10.3390/dj10030044
Chicago/Turabian StyleLončar-Brzak, Božana, Ivana Škrinjar, Vlaho Brailo, Danica Vidović-Juras, Lada Šumilin, and Ana Andabak-Rogulj. 2022. "Burning Mouth Syndrome (BMS)—Treatment with Verbal and Written Information, B Vitamins, Probiotics, and Low-Level Laser Therapy: A Randomized Clinical Trial" Dentistry Journal 10, no. 3: 44. https://doi.org/10.3390/dj10030044
APA StyleLončar-Brzak, B., Škrinjar, I., Brailo, V., Vidović-Juras, D., Šumilin, L., & Andabak-Rogulj, A. (2022). Burning Mouth Syndrome (BMS)—Treatment with Verbal and Written Information, B Vitamins, Probiotics, and Low-Level Laser Therapy: A Randomized Clinical Trial. Dentistry Journal, 10(3), 44. https://doi.org/10.3390/dj10030044









